BleepingBeauty wrote:Aside from a pharmacological solution (which I will consider, if necessary) and going to bed earlier and on a regular basis, what can I do to improve this situation?
Pick out a "sleep hygiene" handout (Google, they're all over the place) and follow it to the letter. There is no wiggle room, no "bargaining", because your sleep architecture is marginal and you have symptoms (that's a very key point-- like naps are OK, but only if they don't disrupt your sleep).
Get an absolutely fixed bedtime and awakening time, use it 7 days a week, do not drift. Sleep is a heap of biorhythms that must be set and/or taken advantage of.
At this point, no naps. Naps count towards total sleep time. Napping in the late afternoon might be a good idea for those people who need it and it doesn't affect their sleep, but if you're napping in the morning, that's not napping. That's part of a messed up night of sleep. In your case, I think all of your sleep needs to be consolidated during the night.
No alcohol, caffeine, chocolate, smoking.
Maybe a light snack before bed, no sugar. Stick to carbohydrates or dairy products.
Exercise program.
Cut BMI in
half.
Evaluate bedding for comfort. Cool room temperature. No noise (especially TV).
Relaxation techniques before bed. Yoga, deep breathing, Herb Benson. Clear mind. No computer before bed (the screen eats up the melatonin). No bright lights during the sleeping period.
Establish pre-sleep ritual.
Being female has associated sleep maintainance issues. Morph into Roger.
Bright light therapy-- as soon as you get up in the morning, go outside and get 15-30 minutes of face-sun.
A lavender sachet (lavender helps sleep).
Address any pain issues.
Optimize medications-- are you on anything else other than what's listed? (Baseline heart rate looks OK, could take a look at the graph of that, but chances are they don't generate it)(as in the levothyroxine creating issues).
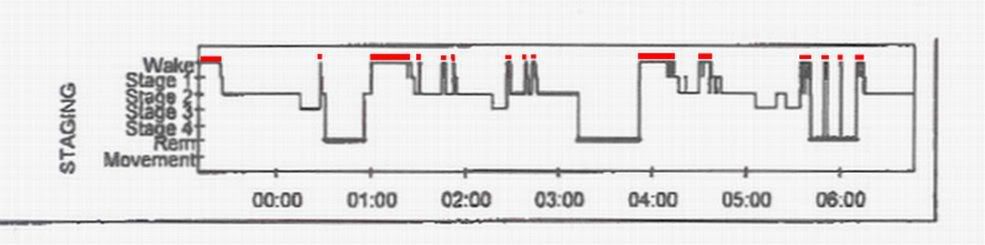
If I were to guess, I would say consolidating your sleep would do the most for improving architecture, followed closely by rigid sleep times to set the biorhythms (think of sleep as matching up a pile of undulating chemicals. If you're in the wrong place during a "peak" (or a "trough", depending on the chemical) you're trying to swim upstream.
BleepingBeauty wrote:But this is making me scratch my head: Why does my new "CPAP Prescription" say that my AHI is 15.4? Where did that number come from?
Insurance coverage number, the AHI on ambient pressure. She probably made it up.
BleepingBeauty wrote:My fear is that I'll choose the wrong machine and wind up in the same boat a year from now.
IMO, you could use a Shop-Vac with one end stuck in 12 cmH2O of "H2O" (just set it to "blow" instead of "suck") and "Warcraft" for software and be fine (fiddling with lowest effective pressure is your choice, but look what happens in every piece of data that has aggressive "fiddling"). Right now, your problem is not "sleep-disordered breathing", it's "sleep".
Muffy