I guess it's time for me to start doing some reading on PLM's.kteague wrote:It's not unusual with limb movements.Tom W wrote: ...Neither of my last sleep studies have shown any SWS but I guess that's not unusual when you're 50.
National (U.S.) Sleep Clinic Recommendations
Re: National (U.S.) Sleep Clinic Recommendations
Re: National (U.S.) Sleep Clinic Recommendations
Sorry to be so targeted on the limb movements. Not saying it's your only issue to address, just know that for me, nothing was as it seemed until both the movements and the breathing were addressed, and that leaving either one unattended has the potential to cloud the view of the other. I have a tendency to hold my breath with any exertion, even when awake. Can't help but wonder if holding my breath with my movements affects my nightly data. I am now off the limb movement soapbox unless solicited.Tom W wrote:I guess it's time for me to start doing some reading on PLM's.kteague wrote:It's not unusual with limb movements.Tom W wrote: ...Neither of my last sleep studies have shown any SWS but I guess that's not unusual when you're 50.
_________________
| Mask: TAP PAP Nasal Pillow CPAP Mask with Improved Stability Mouthpiece |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Bleep/DreamPort for full nights, Tap Pap for shorter sessions |
My SleepDancing Video link https://www.youtube.com/watch?v=jE7WA_5c73c
Re: National (U.S.) Sleep Clinic Recommendations
If anyone has a right to bring up limb movements in sleep on a regular basis, it is YOU, Kathy. Thanks for the timely, balanced way you do so. It is a very valuable service to this board, in my opinion.
Re: National (U.S.) Sleep Clinic Recommendations
Not to worry I fully understand.kteague wrote:Sorry to be so targeted on the limb movements. Not saying it's your only issue to address, just know that for me, nothing was as it seemed until both the movements and the breathing were addressed, and that leaving either one unattended has the potential to cloud the view of the other. I have a tendency to hold my breath with any exertion, even when awake. Can't help but wonder if holding my breath with my movements affects my nightly data. I am now off the limb movement soapbox unless solicited.Tom W wrote:I guess it's time for me to start doing some reading on PLM's.kteague wrote:It's not unusual with limb movements.Tom W wrote: ...Neither of my last sleep studies have shown any SWS but I guess that's not unusual when you're 50.
I work with systems at my job and I realize that very rarely does one thing NOT affect everything else in the system. Most times it's not enough to matter but unless you know that for sure you have to look at everything.
I've been doing the CPAP thing for 12 years now and rarely have I felt as good as I thought I should or at least wished I would. I will admit that at times I stop dwelling on it but it does sort of bother me. When it gets bad enough to become a major distraction I take another crack at it.
Re: National (U.S.) Sleep Clinic Recommendations
kteague wrote:That is home video of me several years ago. I have video of me (not posted) when not on Mirapex and my movements then look more like the many other PLMD vids on YouTube, the movements are more contractions without the wild flailing. Multiple sleep studies have captured both the normal and the augmented movements, depending on where I was in their treatment. At this time my movements are consistent with normal PLMD movements. I don't know if the TENS Unit could have helped when augmentation was in play or not. Kinda doubt how effective anything could be against what is seen in the video.avi123 wrote:Question,kteague wrote:avi123 wrote:. (For the newbies who may not have seen my home video of what my augmentation looked like, the link is below. Ranks right up there with the embarassing mask pics. But I don't mind taking a hit for the team. lol)
Is it you doing the "augmentation" in the youtube piece?
Comment,
If the jerking of the legs are so profound as shown in your YouTube link then it could replace going to the gym:)
Your YouTube link:
https://www.youtube.com/watch?v=jE7WA_5c73c
I thought that the limb movements are mostly extentsion of the big toe and flexion of the ankle, and the movements are seperated by 5 to 90 seconds.
But those in the YouTube could be measured by sticking a pedometer to a leg and it would show a total leg jerks for the night.
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 Autoset machine; Ruby chinstrap under the mask straps; ResScan 5.6 |
see my recent set-up and Statistics:
http://i.imgur.com/TewT8G9.png
see my recent ResScan treatment results:
http://i.imgur.com/3oia0EY.png
http://i.imgur.com/QEjvlVY.png
http://i.imgur.com/TewT8G9.png
see my recent ResScan treatment results:
http://i.imgur.com/3oia0EY.png
http://i.imgur.com/QEjvlVY.png
Re: National (U.S.) Sleep Clinic Recommendations
Thanks all. Yeah, the movements in the video are not at all the typical PLMD movements. If I was told to do those movements I couldn't perform like that to save my life. Not strong enough. Interestingly, this didn't seem to use my muscles, it was more like getting an electrical shock - repeatedly. Wish it would have worked as exercise - I'd be the fittest granny I know.
_________________
| Mask: TAP PAP Nasal Pillow CPAP Mask with Improved Stability Mouthpiece |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Bleep/DreamPort for full nights, Tap Pap for shorter sessions |
My SleepDancing Video link https://www.youtube.com/watch?v=jE7WA_5c73c
Re: National (U.S.) Sleep Clinic Recommendations
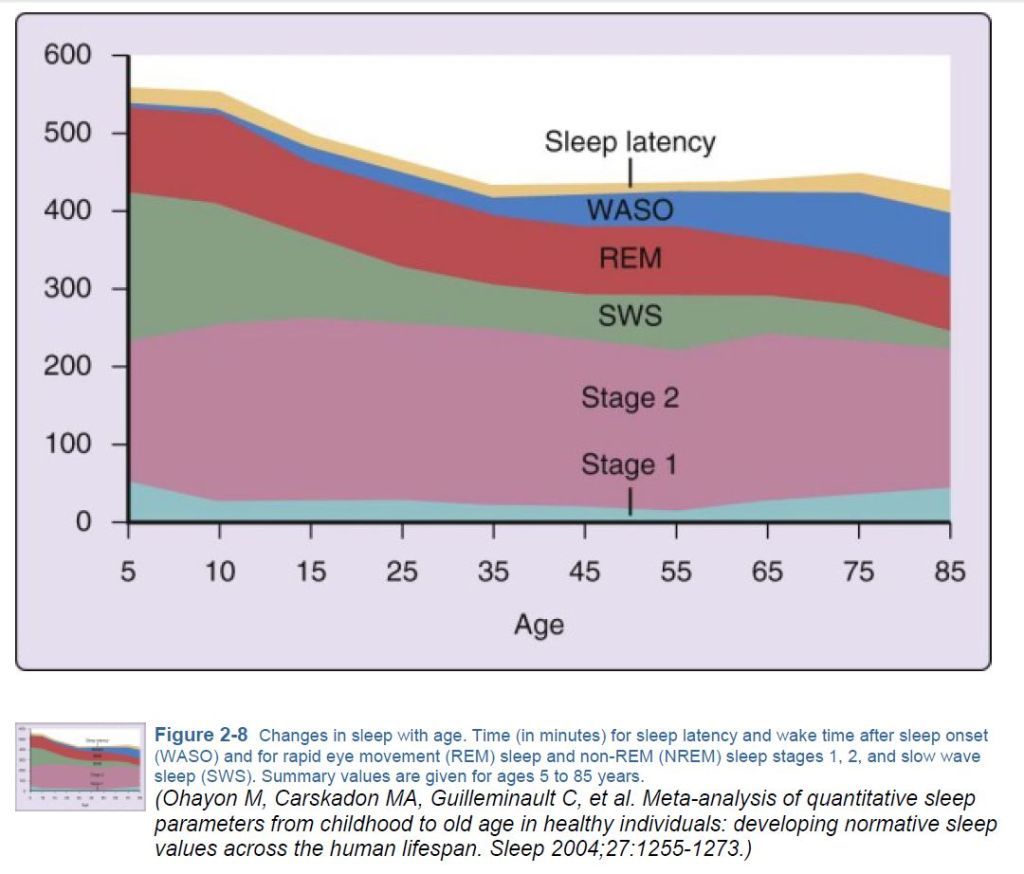
At 50, I believe most nomograms say you should be getting at least some SWS:Tom W wrote: ...Neither of my last sleep studies have shown any SWS but I guess that's not unusual when you're 50.
...other than food...
Re: National (U.S.) Sleep Clinic Recommendations
In looking at whether or not to treat PLMs, one must look at only those that cause arousals, and your index (PLMAI) is only 4.5. Consequently, even if you are able to get PLMAI down to 0.0, it may not result in appreciable benefit.Tom W wrote:Should I be looking to clear up the PLM's (which might help the sleep) or clearing up the apneas (which might clear up some of the PLM's and the sleep)?
That said, here's the current Practice Parameter for RLS/PLMD:
http://www.aasmnet.org/Resources/Practi ... entRLS.pdf
In re: the apneas, if they are all Wake phenomena, or post-arousal in nature (a result, and not a cause of arousal), then expecting any benefit from beating them to death with an ASV would be unrealistic.
...other than food...
- MarquisdeStyle
- Posts: 20
- Joined: Sun Apr 03, 2005 12:39 pm
- Location: Nashville, TN
Re: National (U.S.) Sleep Clinic Recommendations
Kteague,
I watched your video, and while the nurse in me is horrified at what your body goes through at night, the silly part of me LOVES your sense of humor with the music choice!
Thanks for being willing to share in a way that can help so many who are suffering!
I watched your video, and while the nurse in me is horrified at what your body goes through at night, the silly part of me LOVES your sense of humor with the music choice!
Thanks for being willing to share in a way that can help so many who are suffering!
Good promises to feed the sparrows, but He doesn't drop the worms in their nests.
Re: National (U.S.) Sleep Clinic Recommendations
deltadave wrote:In looking at whether or not to treat PLMs, one must look at only those that cause arousals, and your index (PLMAI) is only 4.5. Consequently, even if you are able to get PLMAI down to 0.0, it may not result in appreciable benefit.Tom W wrote:Should I be looking to clear up the PLM's (which might help the sleep) or clearing up the apneas (which might clear up some of the PLM's and the sleep)?
That said, here's the current Practice Parameter for RLS/PLMD:
http://www.aasmnet.org/Resources/Practi ... entRLS.pdf
In re: the apneas, if they are all Wake phenomena, or post-arousal in nature (a result, and not a cause of arousal), then expecting any benefit from beating them to death with an ASV would be unrealistic.
Thanks for posting that link. It was disheartening to read that PLMD seems nearly off the radar as far as dedicated research.
In regards to a PLMAI of 4.5 being insignificant, I think one must consider that true PLMD is sometimes (usually? often?) known to worsen with CPAP treatment simply because there are no barriers from apnea arousals to prevent movement manifestation. What showed up in the lab during titration may be totally different from what's happening once therapeutic OSA treatment is in place. Only a repeat study done while using their usual and proven effective pressure will tell the whole story on PLMD. An arousal rate of 4.5 in an 8 hour night nets a grand total of 36 PLMD arousals. Add those to respiratory related and other arousals, and that's pretty fractured sleep. Even if there are no arousals, a complaint of chronic pain, especially in the legs, makes them very significant from a patient's perspective, just not from the current thoughts in sleep medicine. My limb movements severely harmed my lower back, hips, and knees. If they'd never woke me up, that effect would remain an issue. It saddens me that it's probably going to be many years before the powers that be in sleep medicine figure this stuff out. And sad that dopamine agonists are presented as to be so unlikely to be problematic. What am I - just one of the unlucky ones? I spent years dealing with augmentation before "I" figured out it was the medicine causing the problem, not a progression of my disorder. And I developed the compulsive behavior side effect too. No one warned me it could happen and I had no idea for YEARS what was changing me into a person I didn't like very much. Sorry. I can't get off my soapbox on this stuff. Every time I think I've made my peace with what happened to me I realize that the anger is just below the surface waiting to erupt. This frustration is NOT aimed at you Dave. In your line of work you report what you see by the parameters set forth by experts in the field. It's those so-called experts that I'd like to see live my life and see how quick their research target and funding and their treatment recommendations changed. Oh, and of course there is still no mention of TENS as an alternative for treatment.
_________________
| Mask: TAP PAP Nasal Pillow CPAP Mask with Improved Stability Mouthpiece |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Bleep/DreamPort for full nights, Tap Pap for shorter sessions |
My SleepDancing Video link https://www.youtube.com/watch?v=jE7WA_5c73c
Re: National (U.S.) Sleep Clinic Recommendations
Actually, I did not say that a PLMAI of 4.5 was "insignificant". I saidkteague wrote:In regards to a PLMAI of 4.5 being insignificant...
He only showed 30 PLMAs during NPSG, and while the symptom of EDS should be the determining factor in deciding to pharmacologically intervene or not, it should be noted that a previous attempt to treat did not have favorable results. That result should remind us that medication activity is rarely confined to where we want it to be, and the net result of trying to snuff out 30 crummy PLMAs may not (probably not) be worth it....even if you are able to get PLMAI down to 0.0, it may not result in appreciable benefit.
That said, the current Practice Parameters were posted if the "drug wingin'" approach is chosen.
I did look at his arousals, and frankly I am not particularly impressed:kteague wrote:An arousal rate of 4.5 in an 8 hour night nets a grand total of 36 PLMD arousals. Add those to respiratory related and other arousals, and that's pretty fractured sleep.
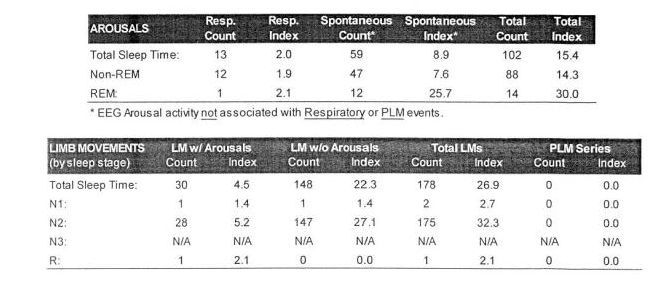
While I personally consider 100 arousals to be the cut-off for eyebrow raising, a lot of folks say that's NBD for a night in the Sleep Center. And if we're not going to do anything about the PLMAs, and probably can't do anything about the RAs, expecting positive results from addressing this area may not be reasonable.
BTW Kathy, did you ever get/post your NPSG? As noted previously, the frequency of your leg movements actually put them out of the accepted range of PLM and into HFLM (or whatever we're calling them today).
Further, because of the severity and muscle groups employed, they could be either parasomnia or REM Behavior Disorder.
...other than food...
Re: National (U.S.) Sleep Clinic Recommendations
Dave, I have not posted any graphs. I only got them for one of the several sleep studies. The rest are so historical I wouldn't want to even try to track them down. In the early years (1990's) my limb movements were much less ominous, and in some studies the arousals were not considered worthy of further attention. Yes, I remember past discussion of the frequency of my limb movements. At the time of my video, my movements did not fit within all of the PLMD parameters. Once I was off the medication, the frequency and characteristics of my movements changed. If my movements had remained at that high frequency there would likely have been a more definitive look at my movements by the doctors. In a more recent video it was actually boring to watch because of the lag time between what usually looked like a repeated stretching of the lower leg and spasms (?) of the toes, or sometimes it was a bicycling motion. I would be real curious if any correlation is seen between HFLM and medications.
I'm really not trying to say I know more than medical professionals. Believe me, I am well aware of my limitations - I'm not one of the great scientific minds, just experienced. I am always impressed with those technical types in discussions here, including you Dave. I'm just saying that understanding (or at least the revelation of any understanding) of the potential effect of some medications on a patient with PLMD, and PLMD knowedge in general, has not "arrived". I was under the care of a family doctor, a sleep doctor, an orthopedic doctor, a pulmonologist, and a neurologist. Not one of them said, "Hey, maybe you are experiencing augmentation on your medication." Only my last sleep doc was inclined to look at it further as a possibility. Am I off base to think that legs never really resting is harmful unrelated to sleep disturbances? That's something I want to understand more. I have more questions than answers, but if someone is not asking the questions, who will feel the need to find answers?
I'm really not trying to say I know more than medical professionals. Believe me, I am well aware of my limitations - I'm not one of the great scientific minds, just experienced. I am always impressed with those technical types in discussions here, including you Dave. I'm just saying that understanding (or at least the revelation of any understanding) of the potential effect of some medications on a patient with PLMD, and PLMD knowedge in general, has not "arrived". I was under the care of a family doctor, a sleep doctor, an orthopedic doctor, a pulmonologist, and a neurologist. Not one of them said, "Hey, maybe you are experiencing augmentation on your medication." Only my last sleep doc was inclined to look at it further as a possibility. Am I off base to think that legs never really resting is harmful unrelated to sleep disturbances? That's something I want to understand more. I have more questions than answers, but if someone is not asking the questions, who will feel the need to find answers?
_________________
| Mask: TAP PAP Nasal Pillow CPAP Mask with Improved Stability Mouthpiece |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Bleep/DreamPort for full nights, Tap Pap for shorter sessions |
My SleepDancing Video link https://www.youtube.com/watch?v=jE7WA_5c73c
Re: National (U.S.) Sleep Clinic Recommendations
Reading between the lines does this mean, "This is as good as it gets"?deltadave wrote: I did look at his arousals, and frankly I am not particularly impressed:
While I personally consider 100 arousals to be the cut-off for eyebrow raising, a lot of folks say that's NBD for a night in the Sleep Center. And if we're not going to do anything about the PLMAs, and probably can't do anything about the RAs, expecting positive results from addressing this area may not be reasonable.
Re: National (U.S.) Sleep Clinic Recommendations
Hi Tom:
Sorry you are having such difficulty in getting your AHI down to a good number.
When I started CPAP, my numbers averaged around 12 (I never had a titration so I don't know what a titration study result could have been.) My machine is an older model of your same machine. The machine was originally set to 4/25 cm H2O. The auto mode jacked up the pressure to deal with the OSA event, but not fast enough to avoid the arousal that resulted. Hence, serious sleep fragmentation.
Based on information from this discussion group, I started my own titration and eventually got to 14.5/17.5 cm H2O.
With that and weight loss, I routinely get down to an AHI of 1.5 to 3.5 depending on the phases of the moon and other exotic criteria .
That said, I have many of your same problems. My PLMS rate is 49 per hour somewhat less than yours at 66 but enough to contribute to fragmenting my sleep. The number of arousals associated with leg movements was 4 per hour and that seems to be what still it is two years later. CPAP doesn't help with RLS/PLMS at all. Separate condition, separate treatment.
First, PLMS (restless leg syndrome) can really make a difference so you should pursue getting a real diagnosis and real treatment. A first test is a serum ferritin level. If it's too low, it makes the RLS/PLMS much worse.
There are medications that can help.
Second, the first study you posted had a note about excess leakage at 12 cm H2O and a suggestion of changing masks.
Looking at you data suggests to me that rasing the IPAP pressure substantially will be needed to cope with the OSA's and that you (and the sleep lab) couldn't do that because of leakage. I would go back to, or find a new, DME who can fit you properly with your existing mask or find one that fits better. Get agreement from your sleep doc to experiment with pressures and then, during the fitting, be lying down with the new higher pressures you'd like to try as they help you with the fitting. Getting a mask adjusted while at a lower pressure or while seated is a waste of time. You need to be in the position you sleep in and with the anticipated pressure.
Third, one of the graphs you posted showed that IPAP got up to 18 cm H2O for that night. In my case, my obstructive events were being handled by the machine in auto mode, and I still felt crappy during the day. Only after the OSA's were almost completely suppressed by the higher IPAP / EPAP pressures did I start getting better rest. Even so, I couldn''t get below an AHI of 5-8 until I lost 36 pounds from my inital weight of 266. Then the AHI started to come down. One of the recommendations seemed to be to lose weight - so that's something to think about.
Hope this is some help.
Sorry you are having such difficulty in getting your AHI down to a good number.
When I started CPAP, my numbers averaged around 12 (I never had a titration so I don't know what a titration study result could have been.) My machine is an older model of your same machine. The machine was originally set to 4/25 cm H2O. The auto mode jacked up the pressure to deal with the OSA event, but not fast enough to avoid the arousal that resulted. Hence, serious sleep fragmentation.
Based on information from this discussion group, I started my own titration and eventually got to 14.5/17.5 cm H2O.
With that and weight loss, I routinely get down to an AHI of 1.5 to 3.5 depending on the phases of the moon and other exotic criteria .
That said, I have many of your same problems. My PLMS rate is 49 per hour somewhat less than yours at 66 but enough to contribute to fragmenting my sleep. The number of arousals associated with leg movements was 4 per hour and that seems to be what still it is two years later. CPAP doesn't help with RLS/PLMS at all. Separate condition, separate treatment.
First, PLMS (restless leg syndrome) can really make a difference so you should pursue getting a real diagnosis and real treatment. A first test is a serum ferritin level. If it's too low, it makes the RLS/PLMS much worse.
There are medications that can help.
Second, the first study you posted had a note about excess leakage at 12 cm H2O and a suggestion of changing masks.
Looking at you data suggests to me that rasing the IPAP pressure substantially will be needed to cope with the OSA's and that you (and the sleep lab) couldn't do that because of leakage. I would go back to, or find a new, DME who can fit you properly with your existing mask or find one that fits better. Get agreement from your sleep doc to experiment with pressures and then, during the fitting, be lying down with the new higher pressures you'd like to try as they help you with the fitting. Getting a mask adjusted while at a lower pressure or while seated is a waste of time. You need to be in the position you sleep in and with the anticipated pressure.
Third, one of the graphs you posted showed that IPAP got up to 18 cm H2O for that night. In my case, my obstructive events were being handled by the machine in auto mode, and I still felt crappy during the day. Only after the OSA's were almost completely suppressed by the higher IPAP / EPAP pressures did I start getting better rest. Even so, I couldn''t get below an AHI of 5-8 until I lost 36 pounds from my inital weight of 266. Then the AHI started to come down. One of the recommendations seemed to be to lose weight - so that's something to think about.
Hope this is some help.
_________________
| Mask: Oracle HC452 Oral CPAP Mask |
| Humidifier: DreamStation Heated Humidifier |
| Additional Comments: EverFlo Q 3.0 Liters O2 PR DSX900 ASV |
Oracle 452 Lessons Learned Updated
DSX900 AutoSV with HC150 extra humidifier and Hibernite heated hose
Settings: EPAP Min-10.0, EPAP Max-17, PS Min-3, PS Max-10, Max Pressure-20, Rate-Auto, Biflex-1.
Sleepyhead and Encore Pro 2.21.
DSX900 AutoSV with HC150 extra humidifier and Hibernite heated hose
Settings: EPAP Min-10.0, EPAP Max-17, PS Min-3, PS Max-10, Max Pressure-20, Rate-Auto, Biflex-1.
Sleepyhead and Encore Pro 2.21.











