National (U.S.) Sleep Clinic Recommendations
Re: National (U.S.) Sleep Clinic Recommendations
[quote="kteague"][/quote]
From the links posted in this thread (by Dave, jnk, in WebMD, and your) I have gained the following info:
1) My RLS and PMLD started as did the OSA two years ago when I came down with Peripheral Neuropathy (Numbness in the soles of the feet.)
2) I should discontinue the Paxil and Xanax that I take now.
3) I should double the Gabapentin (generic Neurontin) dose from 300 mg to 600 mg, daily.
The idea is to stop my RES (residual excessive sleepiness) in the daytime.
THANKS!
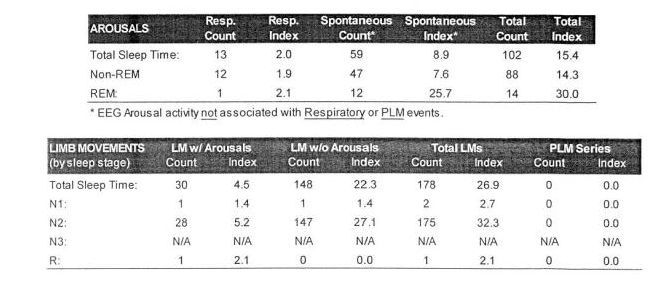
In 2010 sleep study I had PLM Index of 79, and PLM Arousal Index of 5.
In 2012 sleep study I had PLM Index of 55, and PLM Arousal Index of 2.
From the links posted in this thread (by Dave, jnk, in WebMD, and your) I have gained the following info:
1) My RLS and PMLD started as did the OSA two years ago when I came down with Peripheral Neuropathy (Numbness in the soles of the feet.)
2) I should discontinue the Paxil and Xanax that I take now.
3) I should double the Gabapentin (generic Neurontin) dose from 300 mg to 600 mg, daily.
The idea is to stop my RES (residual excessive sleepiness) in the daytime.
THANKS!
In 2010 sleep study I had PLM Index of 79, and PLM Arousal Index of 5.
In 2012 sleep study I had PLM Index of 55, and PLM Arousal Index of 2.
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 Autoset machine; Ruby chinstrap under the mask straps; ResScan 5.6 |
see my recent set-up and Statistics:
http://i.imgur.com/TewT8G9.png
see my recent ResScan treatment results:
http://i.imgur.com/3oia0EY.png
http://i.imgur.com/QEjvlVY.png
http://i.imgur.com/TewT8G9.png
see my recent ResScan treatment results:
http://i.imgur.com/3oia0EY.png
http://i.imgur.com/QEjvlVY.png
Re: National (U.S.) Sleep Clinic Recommendations
Just curious, were these results from diagnostic studies or titrations?avi123 wrote:
In 2010 sleep study I had PLM Index of 79, and PLM Arousal Index of 5.
In 2012 sleep study I had PLM Index of 55, and PLM Arousal Index of 2.
_________________
| Mask: TAP PAP Nasal Pillow CPAP Mask with Improved Stability Mouthpiece |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Bleep/DreamPort for full nights, Tap Pap for shorter sessions |
My SleepDancing Video link https://www.youtube.com/watch?v=jE7WA_5c73c
Re: National (U.S.) Sleep Clinic Recommendations
Hey Dave, got a general question for you, or if you you know of a reference. In the titration studies of people who end up (or are already) diagnosed with PLMD, is there a pattern of the PLMs increasing in either frequency or intensity as the night progresses and the pressure becomes increasingly therapeutic? In my mind it seems logical, but I don't know if the facts bear that out. Seems I remember reading that on PubMed years ago but can't seem to find the articles now.deltadave wrote: That said, here's the current Practice Parameter for RLS/PLMD:
http://www.aasmnet.org/Resources/Practi ... entRLS.pdf
_________________
| Mask: TAP PAP Nasal Pillow CPAP Mask with Improved Stability Mouthpiece |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Bleep/DreamPort for full nights, Tap Pap for shorter sessions |
My SleepDancing Video link https://www.youtube.com/watch?v=jE7WA_5c73c
Re: National (U.S.) Sleep Clinic Recommendations
Perhaps a better assessment of the above would be, "There may be a few other things to look at that may give you a better bang for the buck".Tom W wrote:Reading between the lines does this mean, "This is as good as it gets"?deltadave wrote: I did look at his arousals, and frankly I am not particularly impressed:
While I personally consider 100 arousals to be the cut-off for eyebrow raising, a lot of folks say that's NBD for a night in the Sleep Center. And if we're not going to do anything about the PLMAs, and probably can't do anything about the RAs, expecting positive results from addressing this area may not be reasonable.
These could include, but are not limited to:
- Identifying the cause of the anemic REM and correcting it if possible.
- Determining if there is a sleep maintenance issue. I think that's a little too much Wake in the NPSG for a 50 year old, and if the high AHI in Encore is in fact, simply reflecting Wake, Sleep Efficiency could be sub-optimal.
- Do you need an alarm clock to wake up in the AM? Are you groggy when you first wake up? There could simply be Sleep Insufficiency.
- While everyone is yelling Not Enough Pressure, there could be Too Much Pressure. There were NO obstructive events in titration, and that should have prompted a trial pressure reduction.
...other than food...
Re: National (U.S.) Sleep Clinic Recommendations
It has been my general observation that PLMs like Sleep Stability, so once respiratory events have been successfully treated and sleep becomes continuous, huge runs are allowed to appear.kteague wrote:In the titration studies of people who end up (or are already) diagnosed with PLMD, is there a pattern of the PLMs increasing in either frequency or intensity as the night progresses and the pressure becomes increasingly therapeutic? In my mind it seems logical, but I don't know if the facts bear that out.
Consequently, when one sees a solid PLM block like Tom has, one should not immediately go for the benzos because it's often benign.
Conversely, RLS gets the press because it's frequently a problem.
...other than food...
Re: National (U.S.) Sleep Clinic Recommendations
So they've been running the wrong time for 10+ weeks and nobody noticed it yet?Tom W wrote:I saw that too...I'm assuming it didn't take into account daylight savings time?deltadave wrote:Not for nothin', but the Sleep Study started and 8:32PM and finished at 3:46AM?
What's up with THAT?
I'd say it was more like 9:32 to 4:46.
...other than food...
Re: National (U.S.) Sleep Clinic Recommendations
kteague wrote:Just curious, were these results from diagnostic studies or titrations?avi123 wrote:
In 2010 sleep study I had PLM Index of 79, and PLM Arousal Index of 5.
In 2012 sleep study I had PLM Index of 55, and PLM Arousal Index of 2.
Reply:
Diagnostic, 10/11, 2010:
24 isolated limb movements, 6 periodic limb movements with PLM index of 1.7,
and Limb movement arousal index of 1.2, and PLM arousal of zero.
These values not significant.
Titration, 11/4, 2010:
51 isolated limb movements, 299 periodic movements, with a PLM index of 79 per hour.
Limb movement arousal Index of 1.6, and PLM arousal Index of 5.0
These values are borderline significant. Normal PLM-AI is less than 5-10 events per hour.
Titration, 02/14/2012:
52 isolated limb movements. 211 periodic limb movements, with PLM index of 55.
Limb movement arousal Index of 0.5, and PLM arousal Index of 2.1.
These values are not significant.
I take 20 mg of Paxil, 0.5 mg of Alprazolam ER (generic Xanax), and 300 mg of Gabapentin (generic Neurontin), daily.
According to the links in this thread, Paxil, and Benzodiazepines, contribute to RLS. But Gabapentin is good.
My OSA treatment is good but I want to get rid of residual excessive sleepiness in the mornings.
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 Autoset machine; Ruby chinstrap under the mask straps; ResScan 5.6 |
Last edited by avi123 on Mon Aug 13, 2012 10:20 pm, edited 3 times in total.
Re: National (U.S.) Sleep Clinic Recommendations
During my titration all of my REM periods were ended by events. 1 from limb movements and 2 by centrals. Of course you could look at this the other way and say the ending REM periods caused 3 events...deltadave wrote: Perhaps a better assessment of the above would be, "There may be a few other things to look at that may give you a better bang for the buck".
These could include, but are not limited to:
Identifying the cause of the anemic REM and correcting it if possible.
Determining if there is a sleep maintenance issue. I think that's a little too much Wake in the NPSG for a 50 year old, and if the high AHI in Encore is in fact, simply reflecting Wake, Sleep Efficiency could be sub-optimal.
Do you need an alarm clock to wake up in the AM? Are you groggy when you first wake up? There could simply be Sleep Insufficiency.
Yes I do need an alarm clock (and usually an elbow from the wife) in order to wake up. I often wake with that hangover type fog/headache even though I don't drink.
It has been the PR System One's high Obstructive Index that has prompted the increase in pressure from both doctors. In fact when I saw that there were no obstructives during the titration I was first shocked but then remembered that I originally felt that the machine was improperly tagging my events and it began to make much more sense.deltadave wrote: While everyone is yelling Not Enough Pressure, there could be Too Much Pressure. There were NO obstructive events in titration, and that should have prompted a trial pressure reduction.
I would agree that there is a very strong possibility that they're ALL central.
Of course now this leads to me having to suggest that the PR System One might have 'mis-tagged' over 70 events per evening for over a year straight....no easy feat.
But in a way it might partially explain why there is very little, if any, correlation between pressure and and AHI. If you look at one of the first SleepyHead recaps that I posted in this thread there are several periods where the Doctor returned to the baseline pressure of 12cm and the AHI averages are all over the place.

Re: National (U.S.) Sleep Clinic Recommendations
How about on the weekends? Do you "sleep in" to catch up?Tom W wrote:Yes I do need an alarm clock (and usually an elbow from the wife) in order to wake up. I often wake with that hangover type fog/headache even though I don't drink.
People need a certain quantity of sleep. In turn, this sleep, if properly constructed, has distinctive characteristics, termed architecture.
While in the last NPSG, your architecture looked like

a "normal" architecture should look like

I think the next "dial wingin'" experiment should be to add 30 minutes of sleep per day to try to add one more REM period.
...other than food...
Re: National (U.S.) Sleep Clinic Recommendations
And no naps. They disturb Process S:


...other than food...
Re: National (U.S.) Sleep Clinic Recommendations
deltadave wrote:And no naps. They disturb Process S:
What's the meaning of these curves and what's Process S?
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 Autoset machine; Ruby chinstrap under the mask straps; ResScan 5.6 |
Re: National (U.S.) Sleep Clinic Recommendations
I typically get more (30-60 min) sleep on the weekends but rarely sleep until I get up naturally.deltadave wrote:How about on the weekends? Do you "sleep in" to catch up?Tom W wrote:Yes I do need an alarm clock (and usually an elbow from the wife) in order to wake up. I often wake with that hangover type fog/headache even though I don't drink.
I think the next "dial wingin'" experiment should be to add 30 minutes of sleep per day to try to add one more REM period.
When I do sleep until I wake up on my own the results are mixed. Sometimes I wake up refreshed and other times I wake up feeling worse.
Re: National (U.S.) Sleep Clinic Recommendations
Do you know that staring at a computer screen destroys melatonin?Posted: Tue Aug 14, 2012 2:53 am by Tom W
I think I'd also get rid of any afternoon tea and cut the coffee in half.
Are you sure the medication list is complete? That architecture sure has the fingerprint of an SSRI.
Do you have a screenshot of your last couple of months of Patterns of Use (Encore Report, or equivalent)?
...other than food...
Re: National (U.S.) Sleep Clinic Recommendations
Interesting - I did not know that computer screen usage reduced melatonin. My daily usage is 9-10 hours just at work alone.deltadave wrote:Do you know that staring at a computer screen destroys melatonin?Posted: Tue Aug 14, 2012 2:53 am by Tom W
I think I'd also get rid of any afternoon tea and cut the coffee in half.
Are you sure the medication list is complete? That architecture sure has the fingerprint of an SSRI.
Do you have a screenshot of your last couple of months of Patterns of Use (Encore Report, or equivalent)?
Medication list is complete other than a few supplements I take.
Daily baby aspirin
Flax seed oil
multi-vitamin
occasional iron supplement

Re: National (U.S.) Sleep Clinic Recommendations
Using 7.5 hours as a minimum amount of sleep (not counting any Sleep Maintenance issues, which evidence suggests you also have), I would say you're operating with a significant Sleep Debt, represented by the white area in the red box:
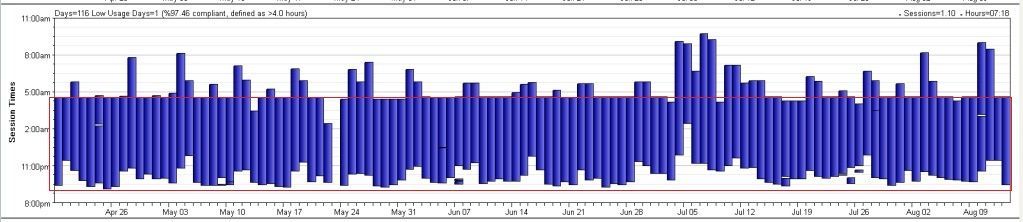
"IMHO", until that debt is paid, difficulty will persist.
Try 9:00 PM bedtime for 2 weeks (and even that won't start paying off the debt, only meet basic requirements)(and hoping that Sleep Maintenance issues aren't extracting a big chunk of sleep).
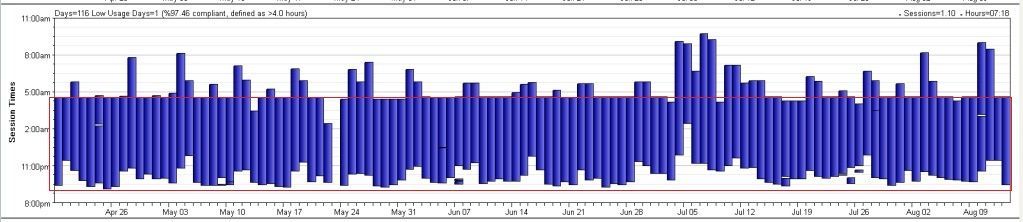
"IMHO", until that debt is paid, difficulty will persist.
Try 9:00 PM bedtime for 2 weeks (and even that won't start paying off the debt, only meet basic requirements)(and hoping that Sleep Maintenance issues aren't extracting a big chunk of sleep).
...other than food...