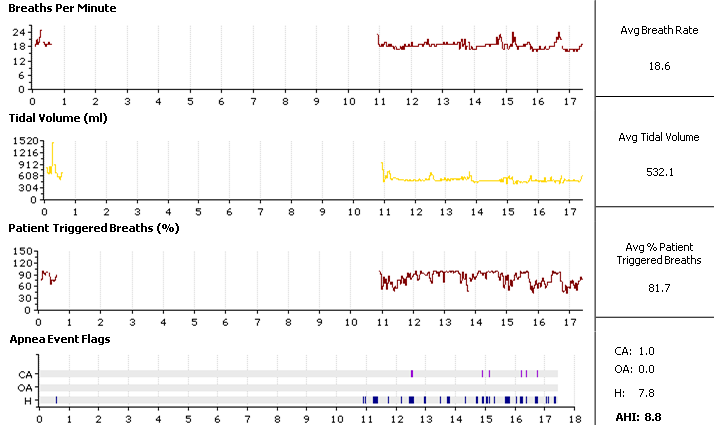
I've been using a new BiPAP S/T for a week with the settings of: IPAP 20, EPAP 20, Ti 1.0, 16 BPM, rise time 3. This comes on the heels of being prescribed a CPAP last summer with a pressure of 13. The old CPAP data and my latest sleep study showed a lot of central apneas while under CPAP therapy -- hence the BiPAP S/T prescription.
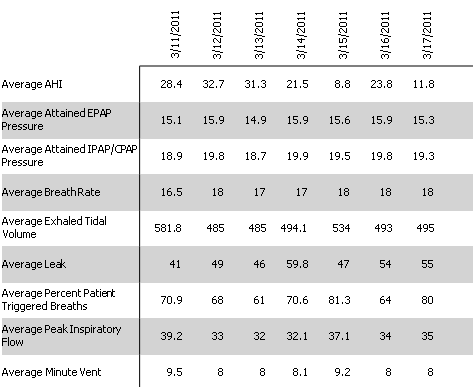
The BiPAP has eliminated the OSA events, but I still have a couple centrals per hour and, perhaps more alarmingly, a lot of hypopnea events. My mean and median AHI for the last week are both around 23.
As was the case with the CPAP, I'm absolutely exhausted the next day after using the unit. I realize this may be the "sleep debt" phenomenon at work, but given that I know my data doesn't look good, I'd like to read what others think.
I was surprised at the high pressures prescribed, given that I'm 31, mostly healthy (other than moderate hypertension), and not extremely overweight. I mention this only in case overtitration is a possible culprit for anything.
Images are posted in chronological order, starting with the summary report of indexes. Thanks in advance for any insights you all can provide.
AGGREGATE DATA
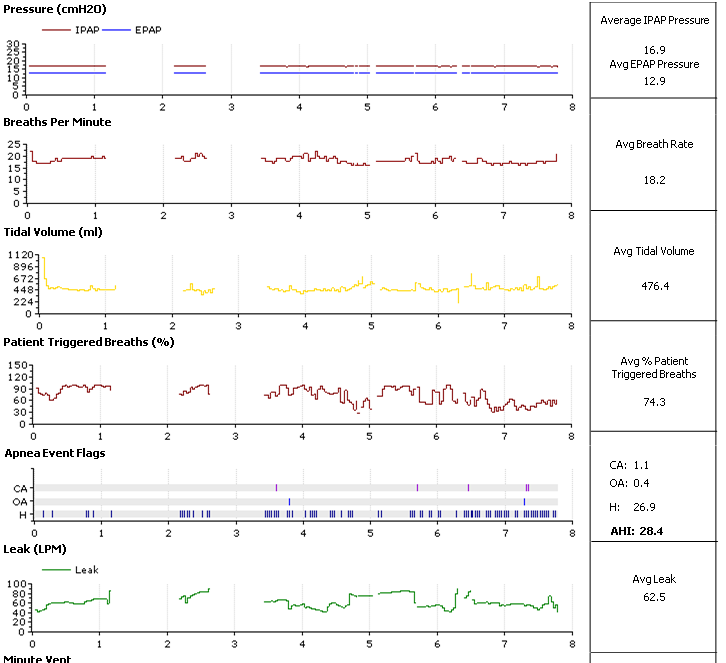
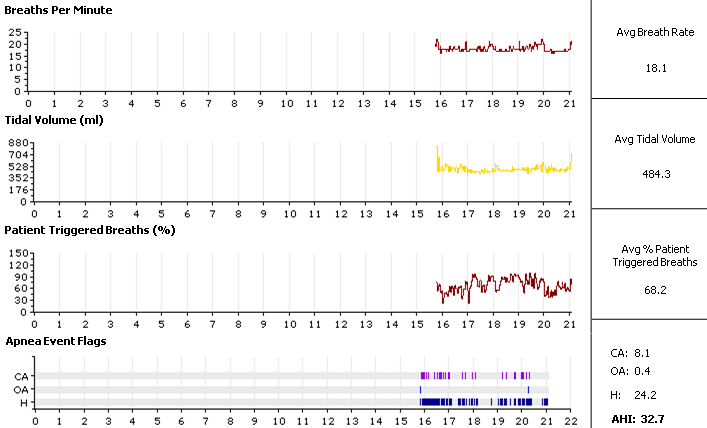
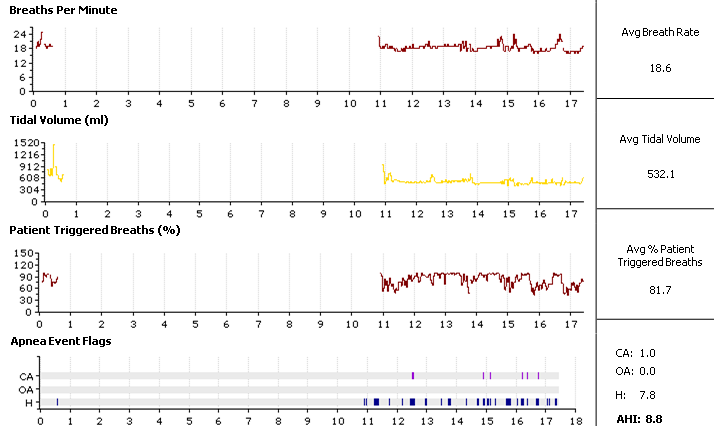
MARCH 12
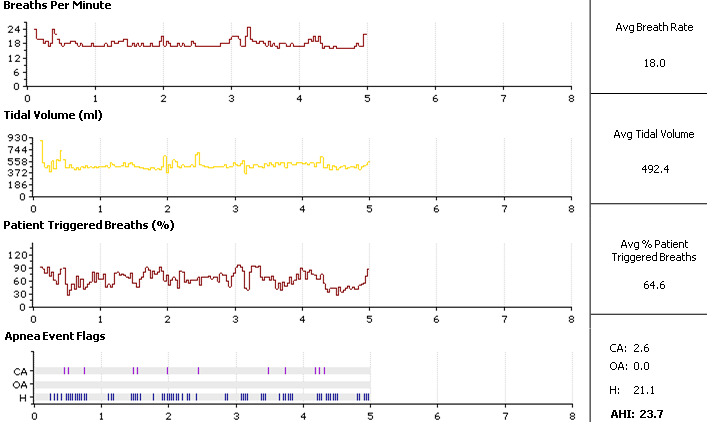
MARCH 14
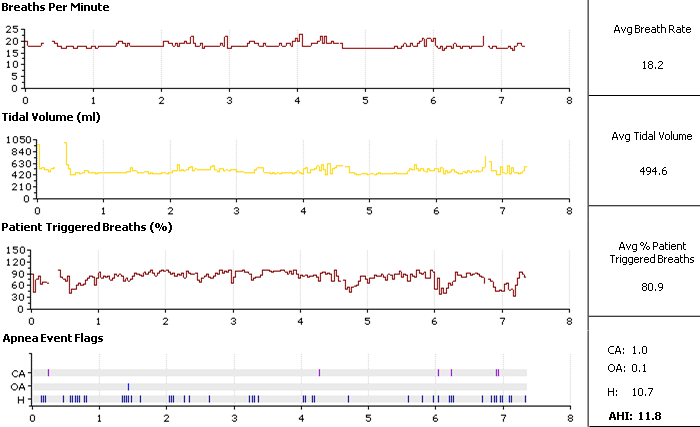
MARCH 15
MARCH 17
MARCH 18