First, let's talk about your correct use of the word "therapy". Because that word is important in the context of this thread's discussion IMO. When you said "therapy", I assume you meant that:Mary Z wrote: I don't know of any OSA/ Complex sleep apnea, central sleep apnea treatment that would disable your spontaneous respiratory drive. ASV inserts a breath or breaths when you're supposed to take a breath and don't, but no therapy inhibits your own drive to breathe.
1) a suitable treatment platform is being utilized, and
2) that treatment platform is already optimized (rather than introducing iatrogenic effect(s) at unacceptable rates)
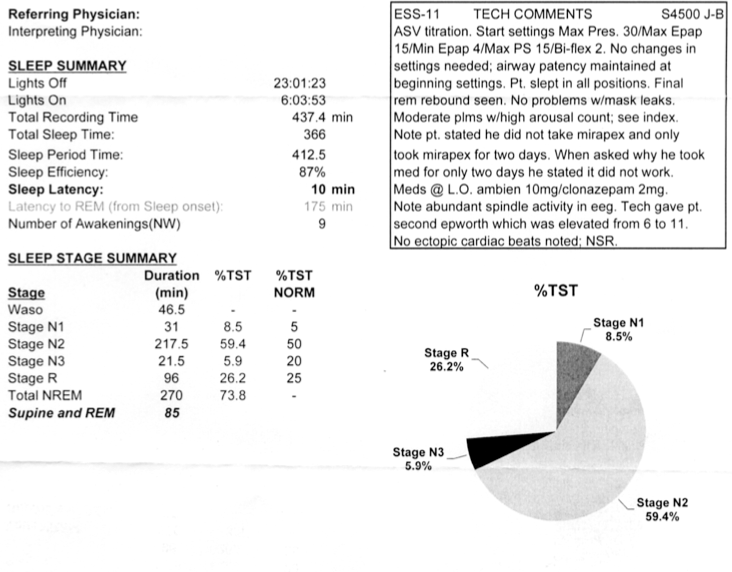
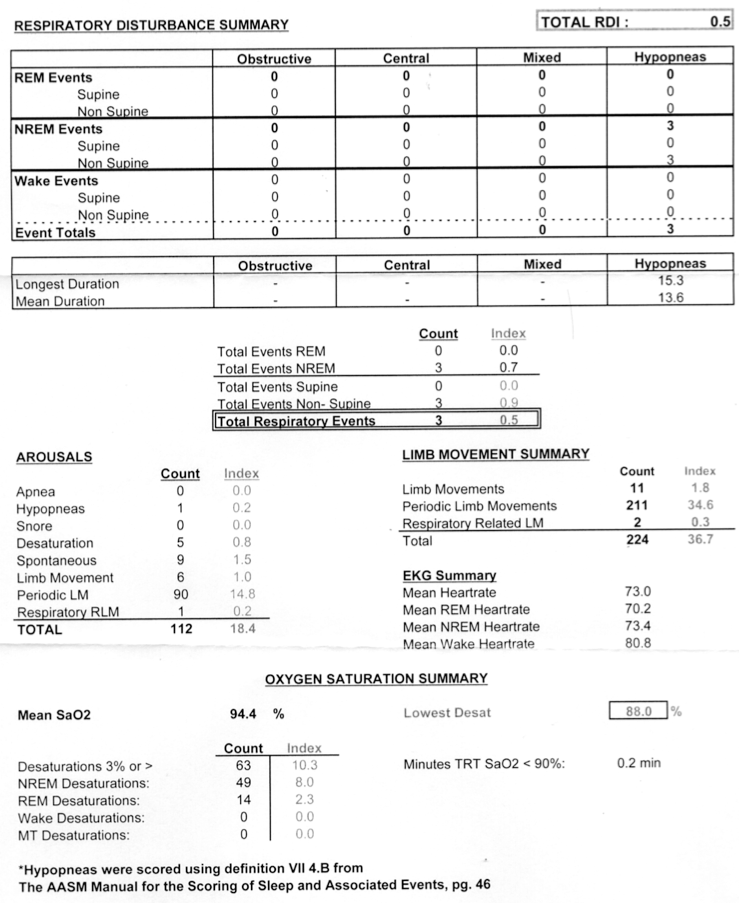
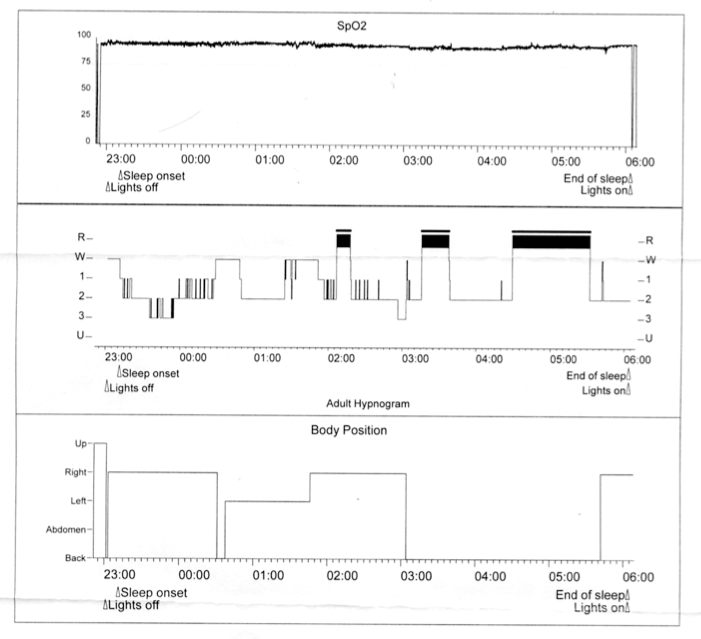
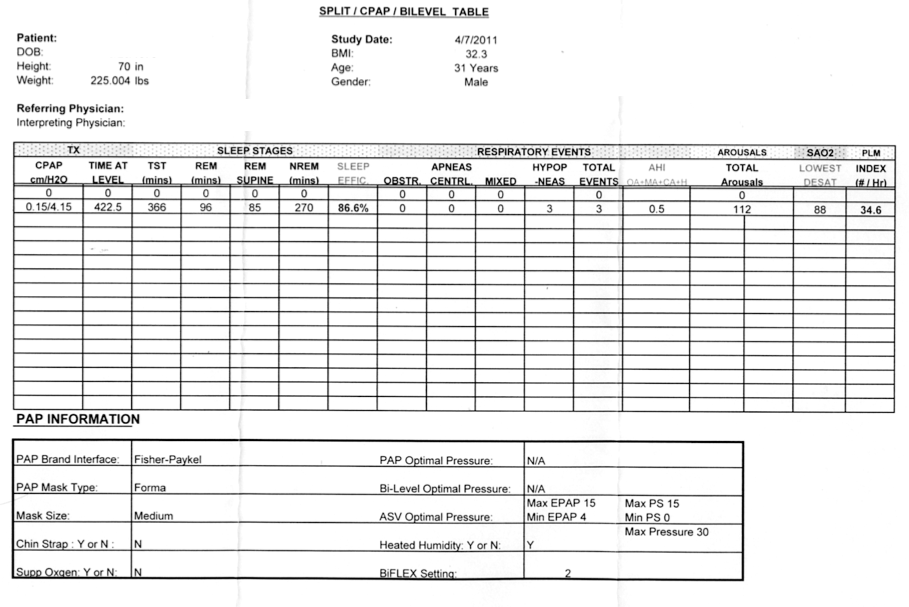
Let's take a peek at the seventh row in Brian's data below:
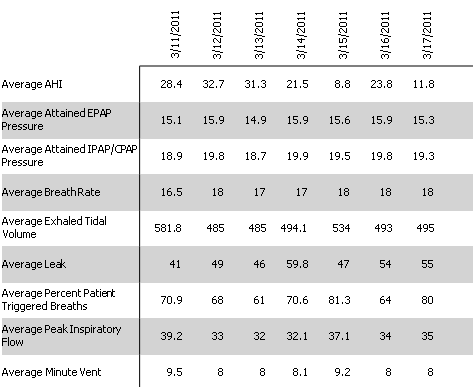
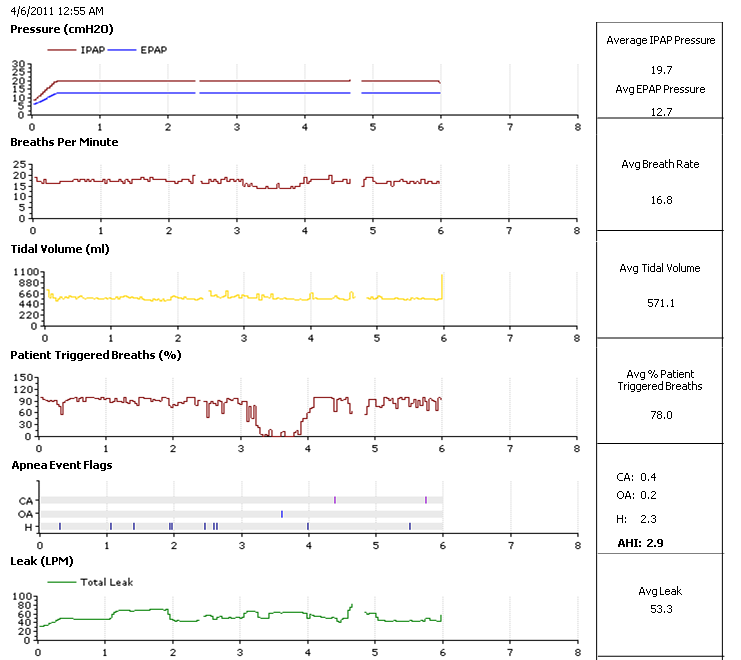
That seventh row means that Brian's machine (and not his spontaneous drive) initiated his breaths: 29.1%, 32%, 39%, 29.4%, 18.7%, 36%, and 20% of the time on each respective night.
Now let's see how often Brian's machine (versus his own spontaneous drive) initiated his breaths that first night he moved his machine's Pressure Support (PS) to a fixed value of 7cm (recall that PS=IPAP-EPAP):
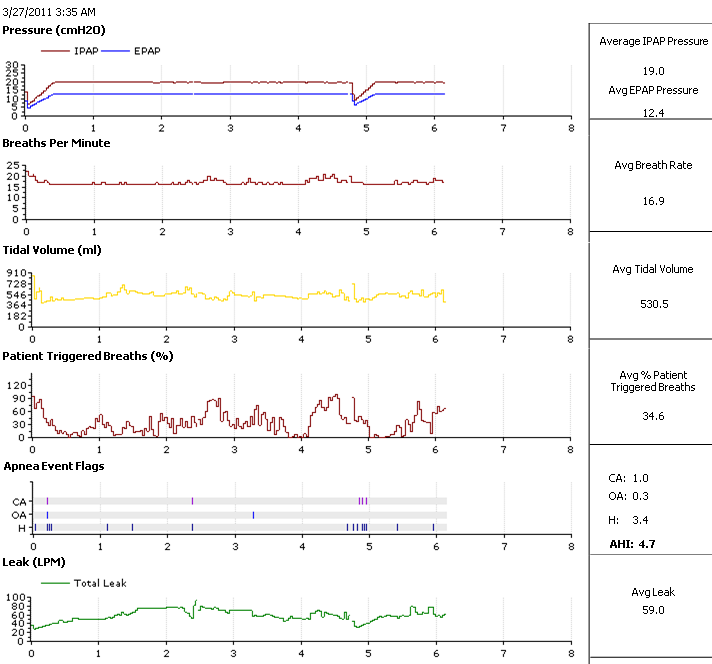
Also bear in mind Brian is using a BiPAP S/T machine above, rather than an ASV platform. But Brian's home experiment that night resulted in his machine initiating his breaths 65.4% of the time---rather than his intact spontaneous drive being allowed to initiate those breaths. Compare that number with the red numbers I have above. So that home experiment set a new record. With that home experiment, Brian went from initiating most of his breaths during sleep to having the machine initiate roughly two-thirds of his breaths. Note the machine's backup rate was not changed. Rather, Brian's respiratory drive changed in response to those new machine settings.
I don't think using a machine that way on a short-term basis is harmful. But I still question whether there are long-term risks---known or unknown---associated with unnecessarily preempting most of Brian's spontaneous breaths each night---year after year. That's the basis of the question about risk that I suggested Brian ask his doctor. And it's also the basis of why I would want to explore the other treatment modalities such as ASV: toward allowing spontaneous drive to initiate most of Brian's breaths rather than machine trigger.
Bear in mind there are patients, unlike Brian, who do not have an intact spontaneous drive. Those patients must rely on machine timing for initiation of all or most of their breaths. When a patient with an intact spontaneous drive must have two-thirds of their breaths initiated by machine timing, then the therapy platform or settings are likely not suitable IMO...
And I suspect that's why Brian's doctor is now arranging an ASV trial.
I think that statement is wrong. Machine-induced central apneas are examples. And above we can see that PAP therapy is capable of introducing an iatrogenic effect that can inhibit respiratory drive at a given rate. We can infer, with those 20/13 settings, that the BiPAP S/T: 1) inhibited the rate at which Brian initiated his breaths, then 2) mechanically interceded with initiation of those now-delayed and now-missing breaths, and additionally 3) performed significant Work of Breathing reduction and mechanical ventilation via that large and constant PS change.Mary Z wrote:... but no therapy inhibits your own drive to breathe.