BrianinTN wrote:So if y'all were me, how would you do things right now?
----
And yes, I realize no one would ever say to a patient "Don't do your prescribed therapy!" -- which is why I'm asking this as what you would do rather than what you would counsel me to do. .
ok, I'll go out in a limb and say what I'd do... considering this (especially the part I put in bold red:)
BrianinTN wrote:Given my travel schedule plus the fact that they haven't even scheduled my ASV titration study, I'm at least two (and probably more like four) weeks away from even the possibility of being on the ASV at home. Given that I generally feel OK (but not great) after a night of no machine, but feel pretty awful day and night while on the BiPAP, would you all keep using it in the interim or take a chill pill until we get to the ASV data?
Sooooo...if it were me -- yeah, I'd probably put the machine aside for the time being. Only because of the bold red words. I'd wait for the ASV titration.
If unsure whether the doctor's office has actually contacted the sleep lab yet about scheduling an ASV titration, I'd start calling the doctor's office every other day, to ask if the sleep lab has given them a date.
After I found out the contact had been made, I'd call the sleep lab to confirm that it is, indeed, scheduled as an
ASV titration...not a "regular" sleep study titration. And while I had them on the phone, I'd mention that if they have a cancellation on a night when the tech that handles ASV titrations is coming in, to please call me.
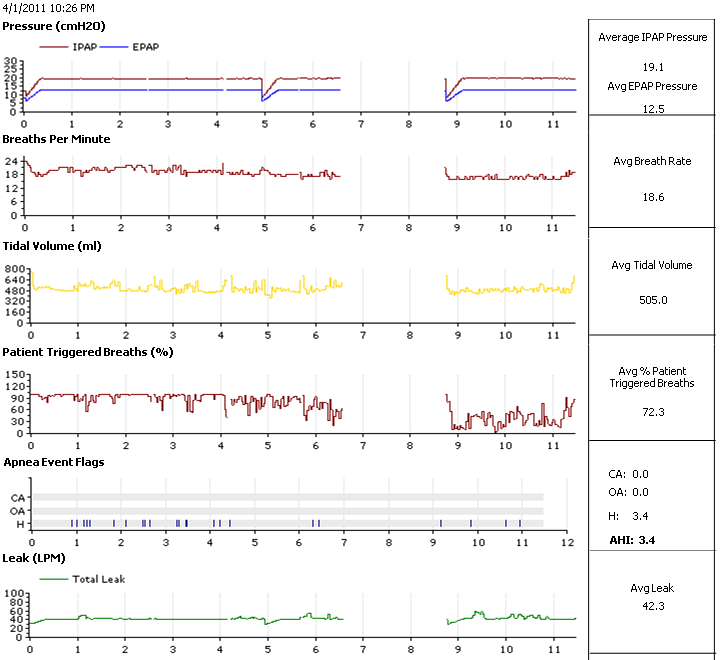
Actually, I'd first beg the doctor to let me try using an ASV at home while waiting. To have the DME loan me an ASV machine while waiting. Doctor probably won't go along with that idea...he'll say the settings
have to be done through a PSG study, yadda, yadda. Meaning, he doesn't have a clue how to tell the DME what settings to put in an ASV for temporary use. Certainly, the settings
should be arrived at via a PSG titration, but I'd
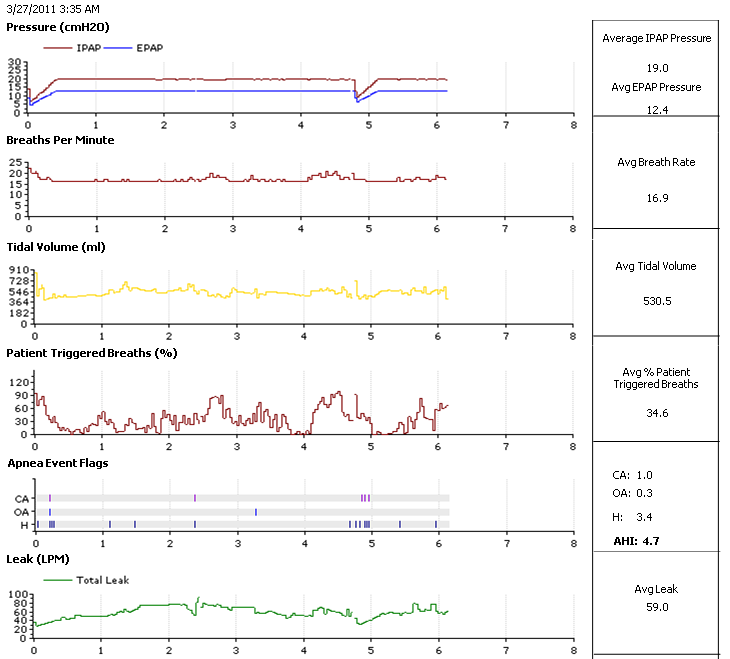
still plead to be allowed to use an ASV at home while waiting. Since you've already been prescribed stratospheric pressures on the S/T anyway...
To make it easier for the doctor to consider your plea... during the begging suggest some settings for the ASV. Phrased perhaps: "
While waiting for the titration...just to help me breathe at night until the titration takes place ...would it be reasonable to temporarily use an ASV at home with settings like IPAP ___, EPAP____, etc.___ just during the wait?"
See if you can nudge -SWS out on the limb (there's room for him right here beside me! ) for a suggestion of ASV settings -- "i
f it were him, in your situation."