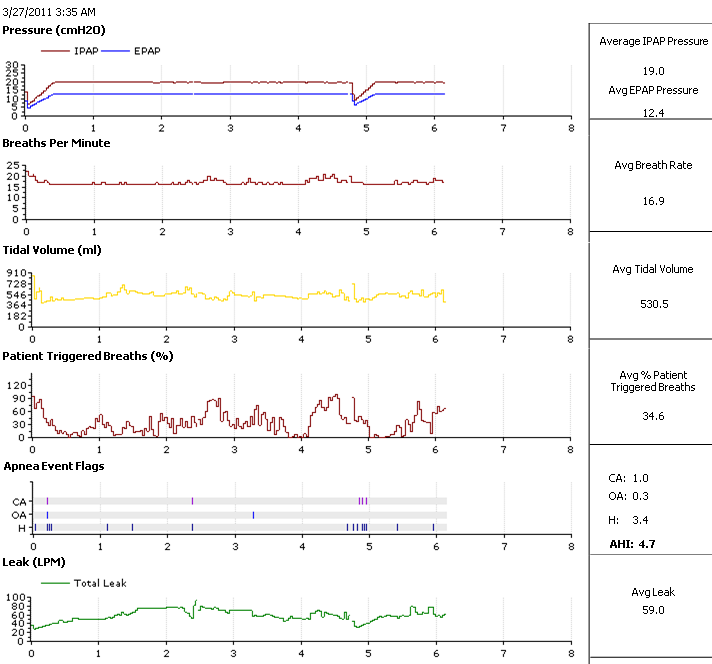
For years, APAP manufacturers have been working with/around 10cm as a statistical barrier beyond which central apneas become progressively machine-induced in the SDB patient population.Mr Bill wrote:That is a very pertinent reference. Since I am at 4700 feet, that is an ~2 psi difference from that at sea level which is equivalent to about 55 inches or 139cm of water. Most therapy does not go over 30cm H2O. But induced centrals happen even over that range. On the other hand...
http://www.madsci.com/manu/gas_gas.htmEmphasis added by me.Chemical Control of Respiration
Special chemical receptors near the aorta and carotid arteries, called the aortic bodies and carotid bodies, are sensitive to an increase in carbon dioxide or acid concentration, or to a decrease in the pressure of oxygen (PaO2). When these receptors sense acidity or low oxygen, they stimulate the brain respiratory center to increase the speed and depth of breathing.
The area of the brain stem that controls respiration is directly responsive to increases in acid concentration in the cerebrospinal fluid, producing increased respirations. When acid buildup occurs, such as in diabetic ketoacidosis, strong stimulation of respiration results. The deep rapid breathing mixes alveolar air with increased amounts of low-CO2 air, leading to a decrease in the carbon dioxide in the blood as it passes by the alveolus. The reduction in CO2 raises the pH back towards normal.
When there is a rise in serum CO2, such as with the increased metabolism of exercise, ventilation is stimulated until the CO2 returns to normal levels.
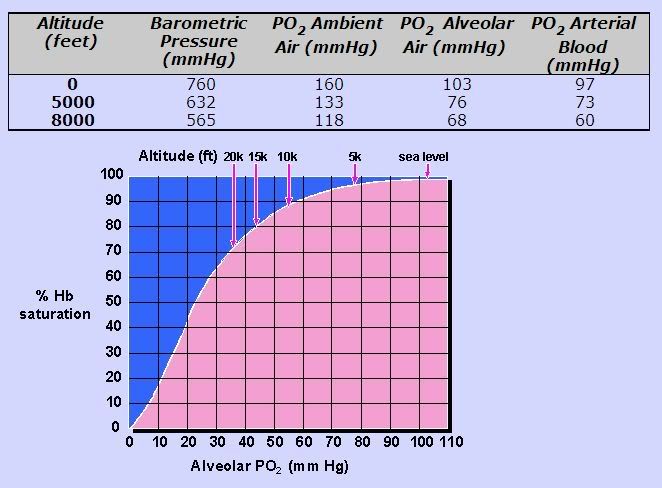
Lack of oxygen also acts as a respiratory stimulant, although a weak one. In healthy individuals at normal altitudes, oxygen levels play no role in regulation of ventilation. As arterial oxygen pressure falls, there is not much stimulation of respiration until the level is below 60 mm Hg. Patients suffering from severe chronic bronchitis and emphysema may come to rely on the “hypoxic drive” to stimulate respirations, as they become habituated to high levels of carbon dioxide.
http://encyclopedia.thefreedictionary.c ... +breathinghttp://encyclopedia.thefreedictionary.com/Bohr+effectHyperventilating causes a drop in CO2 below normal levels, lowering blood and oxygen supply to vital organs due to CO2-induced vasoconstriction and suppressed Bohr effect. Voluntary hyperventilation can cause tissue oxygen levels to go to dangerously low levels leading to, for example, fainting due to brain hypoxia.
I did not realize the Bohr Effect means that CO2 is needed in the blood for oxygen to be properly released to tissue! So, removing too much carbon dioxide from the lungs might induce lowering respiratory drive. So, if we over ventilate somebody, its like we are inducing hyperventilation, the body decides a pause in breathing is needed because CO2 levels in the blood are too low.
Maybe its that adding ~25 cm H2O pressure when you are at an elevation with 139 cm H2O less total pressure, is relatively more hyperventilating than doing so at sea level. Ach! I need to go to bed and sleep.
Thank you for the interesting response. It really got me thinking and I'll be thinking about it all day tomorrow in the environmental lab where I work.
Mr. Bill, although you're sleeping at a moderate 4700 ft, you might find white papers describing the pathophysiology and epidemiology of High Altitude Periodic Breathing (HAPB) interesting:
http://scholar.google.com/scholar?hl=en ... =&as_vis=0
And here's general discussion of HAPB on the web at-large:
http://www.google.com/search?hl=en&q=%2 ... a=N&tab=sw
I also happen to suspect a "threshold confluence" of: 1) moderate altitude, and 2) PAP machine pressure might contribute to CompSAS in some cases.Mr Bill wrote: Maybe its that adding ~25 cm H2O pressure when you are at an elevation with 139 cm H2O less total pressure, is relatively more hyperventilating than doing so at sea level.
And here's a great altitude-comparison graph previously posted by one of our sleep professionals, StillAnotherGuest/Muffy/NotMuffy/deltadave:
viewtopic.php?f=1&t=41034&p=360468&hilit=hapb#p360468