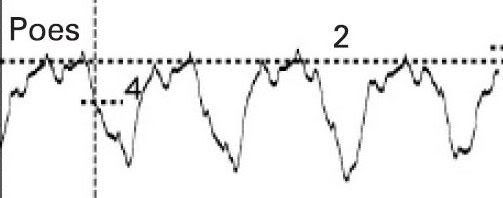
I wouldn't say breath 2 clearly had no iPEEP. Going by their definition, there still is a delay between end-expiration to start inspiratory flow. But based on what is said below, there is a question on its accuracy, which is the same with the other two breaths.Muffy wrote:Are you now totally berserk? The supine example continues to show poor support for this concept and borderline accuracy at best.Split_City wrote:Their vertical line doesn't represent that. The difference between this figure and the Steier seated one is the that start flow doesn't coincide with end-expiration/start inspiratory effort (rise in Pdi). Thus there is iPEEP.
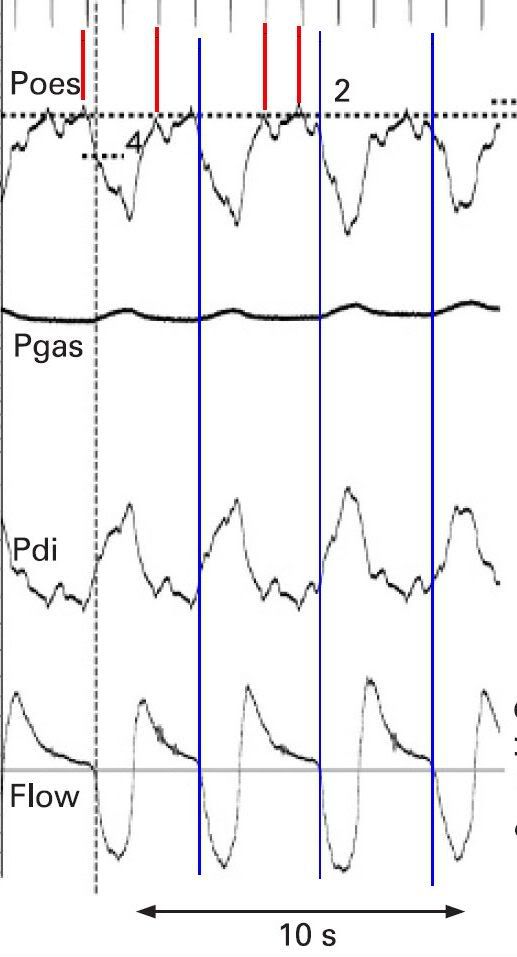
Clearly, breaths 2, 3 and 4 (blue lines) do not exhibit any iPEEP characteristics, so even if breath 1 had iPEEP characteristics, it can be best qualified as an outlier:
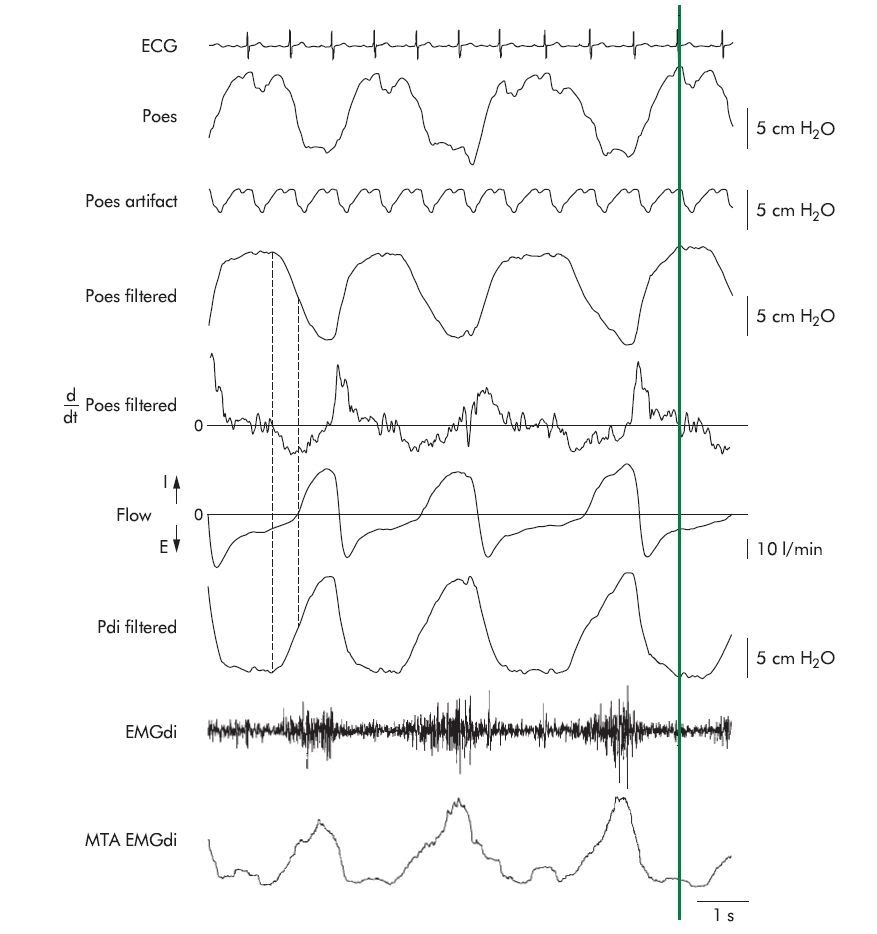
Yep, all very good points. Dr. Fergal O’Donoghue, who did his PhD with us a few years back, measured iPEEP in COPD patients "Effect of CPAP on intrinsic PEEP, inspiratory effort, and lung volume in severe stable COPD. Thoax 2002." In contrast to Steier (well, it looks like it anyway), he filtered out EKG from Pes and Pdi:Muffy wrote:
Muffy wrote:One of my earlier points pertained to performing some verification of signals (biocalibrations or the like) to insure that all signals were accurate in time relative to each other. As an aside, Pankow did this:
but I can see no evidence of that being done in Steier (good news and bad news on that later).Pankow wrote:Time synchronicity of pressure and flow measurements was assessed by placing the flow sensor, the Pao sensor, and the CMT into the tube of a bass-reflex loudspeaker. Over the range of 5–10 Hz, there was a constant time delay (Dt) of airflow in relation to pressures of 0.03 s.
However, in a review of channel synchronicity, the electrical signals seen at the top most likely represent EKG artifact. The red lines on top trace EKG down to the Pes where it can now be seen that there is a huge amount of pulse artifact contaminating the waveform, all of which needs to be subtracted from peak Pes. Consequently, that iPEEP calculation measurement would be more in the neighborhood of about 2. And given the very steep descent of Pes at that point, moving that vertical line just a tiny bit to the left (which looks quite justifiable) would give iPEEP = 0.
Muffy
"We found that, despite optimal balloon placement, there was still
substantial cardiac artefact on Poes and Pga tracings. This
made it difficult to identify reliably the exact point of
inflection in Poes (start of inspiratory effort). Therefore, at
each CPAP pressure the mean cardiac component of the Poes
and Pga records (artefact) was calculated over a period of 2–3
minutes by ensemble averaging the recurrent pressure
fluctuations centred on the R wave of the ECG. The cardiac
artefact was found not to vary substantially within the tidal
volume range. The mean artefact was then subtracted from
the Poes and Pga traces at each cardiac cycle."

Maybe that email to Steier is still worth while . Actually, since I have a litle bit of time on my hands before getting ready to sing some Xmas carols, I might just send off an email