Muffy wrote:I think there's 2 cruxi to the problem:
What is the site and phenomena that creates the obstruction (we obviously agree that there is a fairly hefty obstruction); and
what in turn, causes that.
Instead of looking at iPEEP, I believe it would have been far more helpful to track end expiratory lung volume (EELV), as suggested by your reference 7 (the Boston crowd)(the article link won't post, there's something in it that generates that "Internal Server Error" message on the board)
Arrggghh, EELV has been a major component of my thesis. So do you mean it would have been useful to track EELV during these times of high end-expiratory Pes? Just in relation to the Boston crowd, which actually relates to a lot of my work, they actually measured
change in EELV as measured by magnetometers, not absolute EELV.
Back to SAG. Silly question, but how was the test performed in the supine posture? Was it done by plethysmography? Or does the N2 represent nitrogen washout? We have previously measured FRC using helium dilution during wakefulness but we found it fiddly, with quite variable results within individuals. I couldn't imagine doing it during sleep. Plus, don't you need relatively large tidal volumes to ensure gas mixing and to allow mixing in smaller airways which might be closed at lower tidal volumes?
Muffy wrote:as well as the poster SAG, who went through the trouble of testing himself over 2 years ago to demonstrate how simple it would be to perform that test:
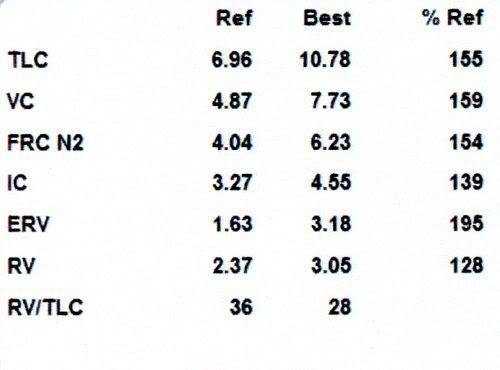
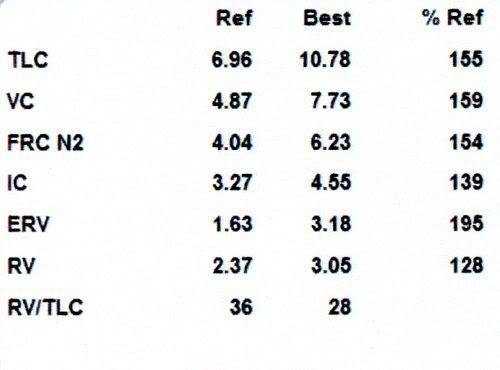
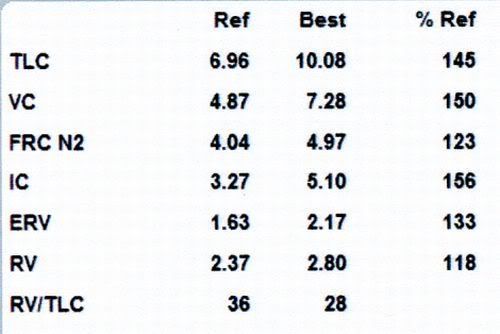
A Comparison of Postural PFTs in a Normal Population
Lung Volumes - Sitting
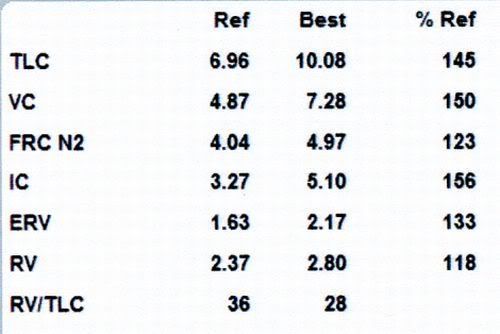
 Lung Volumes - Supine
Lung Volumes - Supine
 viewtopic.php?f=1&t=25185&p=222003&hili ... es#p222003
viewtopic.php?f=1&t=25185&p=222003&hili ... es#p222003
Muffy wrote:as well as revealing valuable information on much ERV would drop when moving from sitting to supine.
But FRC changes very little in the obese following the same change in posture, despite increased mass loading. This formed the basis of my second study + manuscript which is in the process of being reviewed. We have been interested as to why lung volume doesn't decrease in the obese. We thought of a few possibilities and I would love to hear your thoughts.
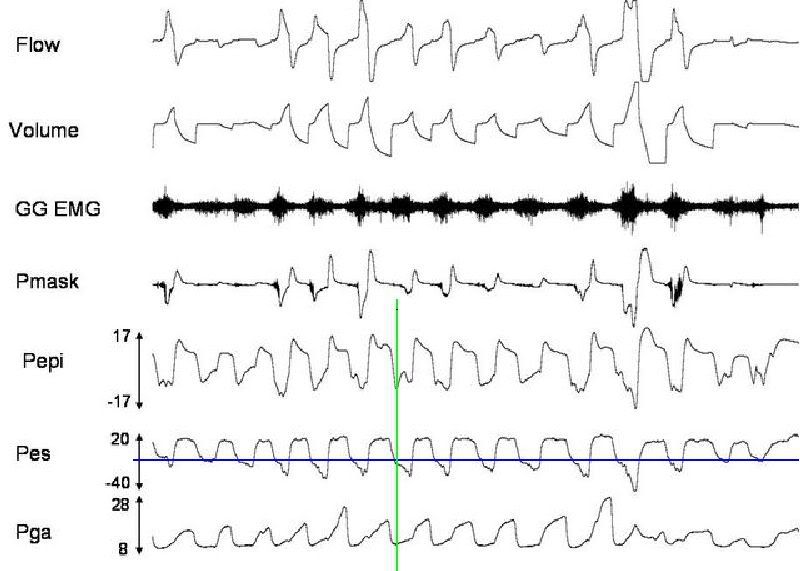
1) This was our major hypothesis. Similar to increased genioglossus activity during wakefulness, we speculated that there would be increased expiratory (tonic) diaphragm muscle activity in obese OSA patients when supine, which prevents/limits the cranial displacement of the diaphragm, and thus preventing/limiting the decrease in EELV
2) EELV in obese individuals is already close to RV i.e. ERV is low. Given that RV changes very little when moving to the supine position, EELV doesn't have much room to fall
3) Something discussed amongst us recently. Given the findings by Steier, it appears that iPEEP increases in the obese when they move to the supine position, which may also limit the decrease in EELV
We found no evidence to suggest that tonic diaphragm activity is higher in obese OSA patients during wake compared to age-matched, healthy-weight controls, thus ruling out point number 1.
Muffy wrote:It becomes extremely noteworthy when one realizes that the poster SAG is also "incredibly fit" (for his age, anyway), so doing a supine PFT on somebody morbidly obese gives information that absolutely must be considered.
hhhmmm, very large volumes! 6L FRC??
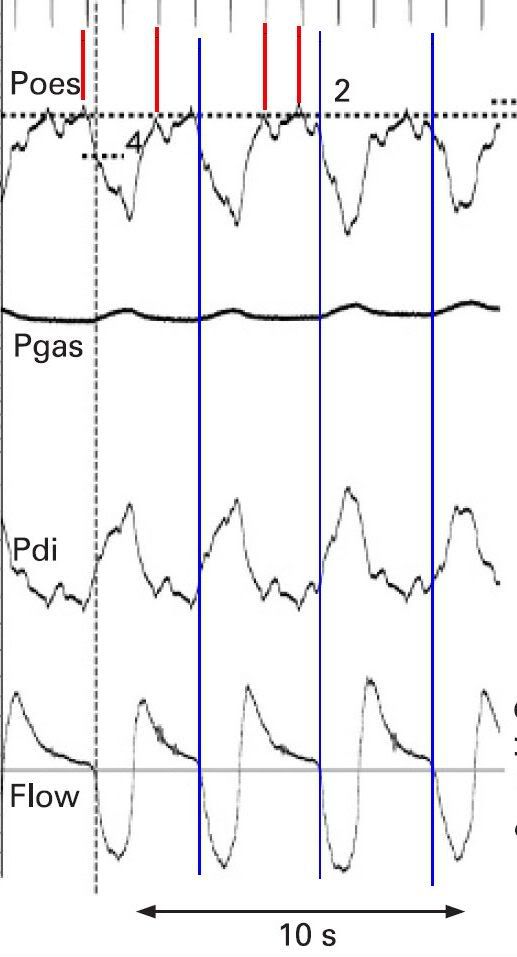
Muffy wrote:Your new image offers further support that tracking iPEEP is either inaccurate or irrelevant:
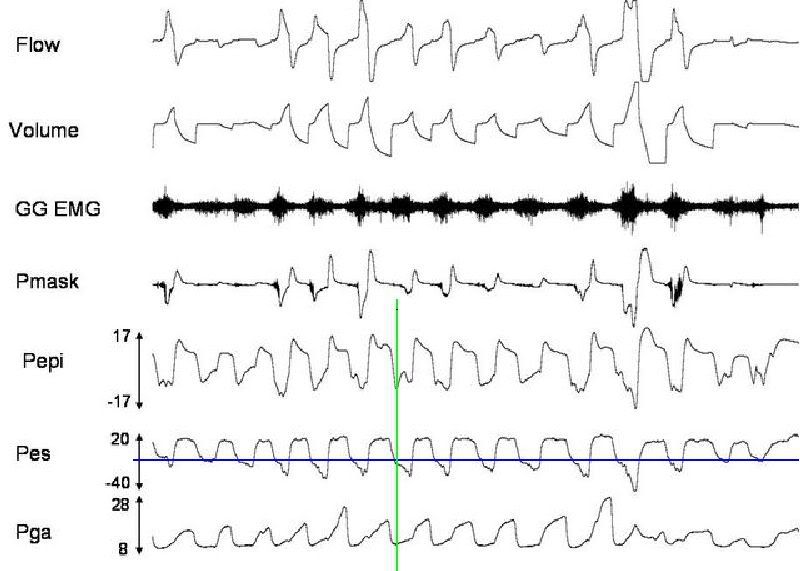
The calculation of iPEEP is based on looking for that stupid blip. As the blue line notes, sometimes you got a blip, sometime you don't. So in answer to your question, yes, I believe there is upper airway obstruction present, the blip represents airway opening, and the flatness of
Pes after opening flow is a reflection of the flow limitation (literally).
Muffy
Yeah it's a bit confusing to me. So iPEEP is the pressure difference between end-expiratory Pes and the onset of flow. But I guess there isn't any flow to begin with because he is initially obstructed. So should iPEEP represent the pressure difference between end-expiratory Pes and when (expiratory) flow reaches zero? Please correct me if I'm wrong!
It's obviously hard to tell on your side but I reckon that my additional line represents the time when expiratory flow reaches zero and when he should be generating airflow, if it weren't for upper airway obstruction. Not much of a difference from your line but it does make a difference in regards to what Pes is.

But it would certainly be interesting to know what's obstructing his airway during expiration. Time to stick a camera down his airway I reckon.