Link between OSA and the "beer gut"
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Link between OSA and the "beer gut"
Ambient pressure. He was taking part in a study in which I was measuring several potentially important variables (genioglossus and diaphragm EMG, lung volume, gastric, esophageal and transidaphragmatic pressures, upper airway resistance) during "natural" apneic events.
Re: Link between OSA and the "beer gut"
In your present study, in Figure 2, the patient looks to be on about 15 cmH2O CPAP with PES about 22 cmH2O for a PMASK - PES pressure gradient of about 7 cmH2O. Was that with abdominal compression?split_city wrote:Ambient pressure. He was taking part in a study in which I was measuring several potentially important variables (genioglossus and diaphragm EMG, lung volume, gastric, esophageal and transidaphragmatic pressures, upper airway resistance) during "natural" apneic events.
I'm trying to understand why the "20 cmH2O patient" had such a high PES in the absence of CPAP and/or abdominal compression. It would seem to be from either an error in the calibration of PES transducer to NPSG or another factor present (like the guy had PEPI compression plus 3 Pizza Hut "Belly Busters" on the way into the sleep lab.
That said, looking at the results of your study may shed light on another thread
viewtopic.php?f=1&t=46945&st=0&sk=t&sd=a&start=255
where one of the "working hypotheses" is that overeating and creating gastric distension may be contributing to not only poor sleep architecture but perhaps alterations in obstructive component as well.
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Link between OSA and the "beer gut"
I'm fairly positive that data came during a period without abdominal compression. Pes at end-expiration is slightly subatmospheric when individuals are upright. However, in this case, patients were supine and on CPAP. Pes in this situation is influenced by a) CPAP and b) compression from mediastinal components. While peak Pes was ~22cmH20, end-expiratory Pes was ~19cmH20. Therefore, adjusted end-expiratory Pes is ~4cmH20. Therefore, compression from the mediastinum is contributing to the ~4cmH20. The mean Pes at end-expiration (without abdominal compression) for the group was 3.2+/-0.8cmH20. Pes with abdominal compression was 4.6+/-0.8cmH20. There was a trend for it being higher with abdominal compression (p=0.06), which supports the decrease in lung volume with abdominal compression.Muffy wrote:In your present study, in Figure 2, the patient looks to be on about 15 cmH2O CPAP with PES about 22 cmH2O for a PMASK - PES pressure gradient of about 7 cmH2O. Was that with abdominal compression?split_city wrote:Ambient pressure. He was taking part in a study in which I was measuring several potentially important variables (genioglossus and diaphragm EMG, lung volume, gastric, esophageal and transidaphragmatic pressures, upper airway resistance) during "natural" apneic events.
As I stated in the other thread, this patient was demonstrating increased respiratory drive as the patient was cycling through respiratory events. There was both an increase in inspiratory drive(increased genioglossus muscle activity) and expiratory drive (gastric pressure [Pga] swings during expiration). During "normal breathing", swings in Pes and Pga are opposite i.e. as Pes goes down during inspiration, Pga goes up. However, during increased expiratory drive (see figure below), contraction of the abdominal muscles during expiration increases Pga. The vertical line clearly shows that peak Pga occurs during expiration i.e. cranking up abdominal muscles. Furthermore, peak Pes appears to to increase with rising expiratory Pga swings. See breath designated by a *. As you can also see by the flow trace, it appears that expiration is also obstructed. (This patient had normal lung function). I believe that the increase in peak Pes is simply due to contraction of the abdominal muscles increasing airway pressure. I think it's also important to distinguish peak expiratory Pes versus end-expiratory Pes. End-expiratory Pes in the example below is predominantly <10cmH20.Muffy wrote:I'm trying to understand why the "20 cmH2O patient" had such a high PES in the absence of CPAP and/or abdominal compression. It would seem to be from either an error in the calibration of PES transducer to NPSG or another factor present (like the guy had PEPI compression plus 3 Pizza Hut "Belly Busters" on the way into the sleep lab.

Now, here's an example from the same subject during "normal" breathing without increased respiratory drive. Peak Pes is closer to ~11cmH20 while end-expiratory Pes is ~6-8cmH20. NOTE: The difference between peak and end-expiratory Pes is likely to be explained by iPEEP (see Steier et al 2009 http://www.ncbi.nlm.nih.gov/pubmed/1938 ... dinalpos=3)

I see no reason to discount such a hypothesis. I would need to look more into it when I have more timeMuffy wrote:That said, looking at the results of your study may shed light on another thread
viewtopic.php?f=1&t=46945&st=0&sk=t&sd=a&start=255
where one of the "working hypotheses" is that overeating and creating gastric distension may be contributing to not only poor sleep architecture but perhaps alterations in obstructive component as well.
Muffy
Re: Link between OSA and the "beer gut"
Actually, I don't see anything in the flow trace to indicate that expiration is obstructed. If anything, it shows quite the opposite.split_city wrote:See breath designated by a *. As you can also see by the flow trace, it appears that expiration is also obstructed.
However, if expiration is also obstructed, then this patient moves beyond the "OSA" category into the "Obstructed Airway" category (and "Let's Go Get A Tracheostomy").
Can you blow the first one up to 30 or 60 seconds?split_city wrote:Now, here's an example from the same subject during "normal" breathing without increased respiratory drive. Peak Pes is closer to ~11cmH20 while end-expiratory Pes is ~6-8cmH20.
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Link between OSA and the "beer gut"
Sure thing. The picture below shows a 60 sec segment which includes that breath indicated by a *. You will have to excuse what I said last night as it was very late. So expiration wasn't "completely" obstructed but can you please make a comment about his expiratory flow profile? I'm certainly no expert in spirometric procedures, but his expiration is of interest. During times of increased drive, he tended to get a brief period of increased flow (generally in the first second), before tapering off to lower flow rates for the rest of expiration. Again, look at the * breath. What's going on here? The expiratory Pga swing is massive, with peak Pga of ~28cmH20. Peak Pes for this expiration is ~20cmH20. However, end-expiratory Pes is ~5cmH20. Is this patient experiencing a lot of iPEEP?Muffy wrote:Actually, I don't see anything in the flow trace to indicate that expiration is obstructed. If anything, it shows quite the opposite.split_city wrote:See breath designated by a *. As you can also see by the flow trace, it appears that expiration is also obstructed.
However, if expiration is also obstructed, then this patient moves beyond the "OSA" category into the "Obstructed Airway" category (and "Let's Go Get A Tracheostomy").
Can you blow the first one up to 30 or 60 seconds?split_city wrote:Now, here's an example from the same subject during "normal" breathing without increased respiratory drive. Peak Pes is closer to ~11cmH20 while end-expiratory Pes is ~6-8cmH20.
Muffy
This patient had normal lung function with FEV1 and FVC both >80% predicted. He wasn't a smoker and not overly obese, with a BMI of ~33 (I think). However, this patient was a little odd compared to the rest of the patients in the group. There were certainly patients displaying expiratory swings in Pga but only during an apnea, and generally only towards the end of the apnea. This guy was showing these expiratory Pga swings (quite large ones at that) for a fair % of the night. I kept thinking maybe the Pes catheter was too low or even in the stomach. But he always showed the typical pressure swings i.e. Pga goes up while Pes went down during inspiration, during stable breathing. This certainly doesn't discount the possibility that the dipahragm moved up, resulting in the Pes catheter being below the diaphragm during unstable breathing.

Here's a figure taken from a paper by Carley et al 1989. It also shows an increase in peak Pes, up to ~20cmH20.

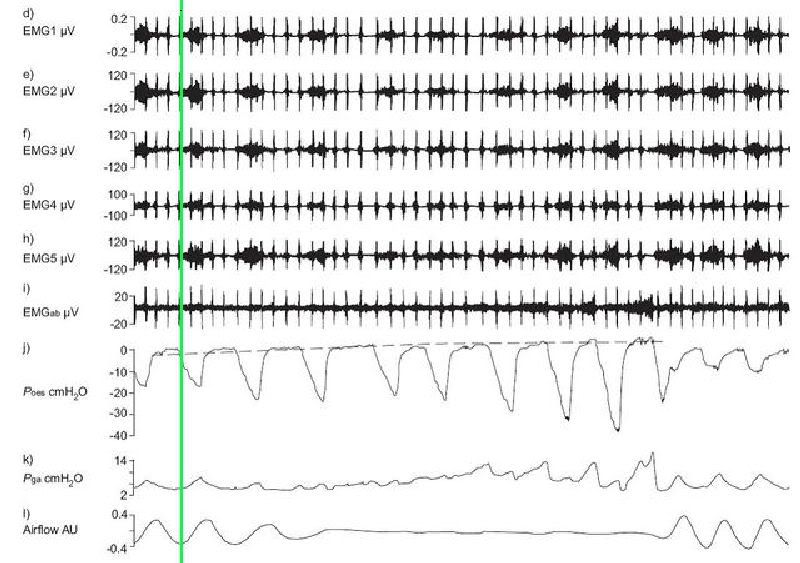
Here's another figure taken from Lou et al 2008 again showing an increase in peak Pes during an apnea. Peak Pes was noted to be less than my example. They also measured abdominal muscle activity (shown as EMGab). You can easily see an increase in muscle activity and Pga swings during expiration for the last three efforts during the apnea. I quote "The EMGab signal was silent at the beginning of an apnoea and became active during the expiratory phase, further supporting the concept that expiratory muscle contraction causes an increase in end expiratory Poes." I actually don't believe they mean end-expiratory Pes, but probably peak Pes.
Also "contraction of the abdominal muscles as evidenced by the rectus muscle EMG, is the cause of increasing end expiratory Poes."

Re: Link between OSA and the "beer gut"
This continues to support my point, that end-expiration in these highly dynamic patients is at the end of the plateau:split_city wrote:Here's another figure taken from Lou et al 2008 again showing an increase in peak Pes during an apnea. Peak Pes was noted to be less than my example.
you can't move it along any further than that because you'd end up with a negative baseline Pes, which is impossible.
Therefore, in this patient, your high baseline Pes is 20 cmH2O (and not 5 cmH2O), and is contaminated by the CPAP (although these examples are starting to run into each other. Is this patient, in fact, on CPAP?):

I imagine you're calling end-expiratory Pes at the red line, but assuming your signals are synched, I think it would be more appropriately called at the green lines:
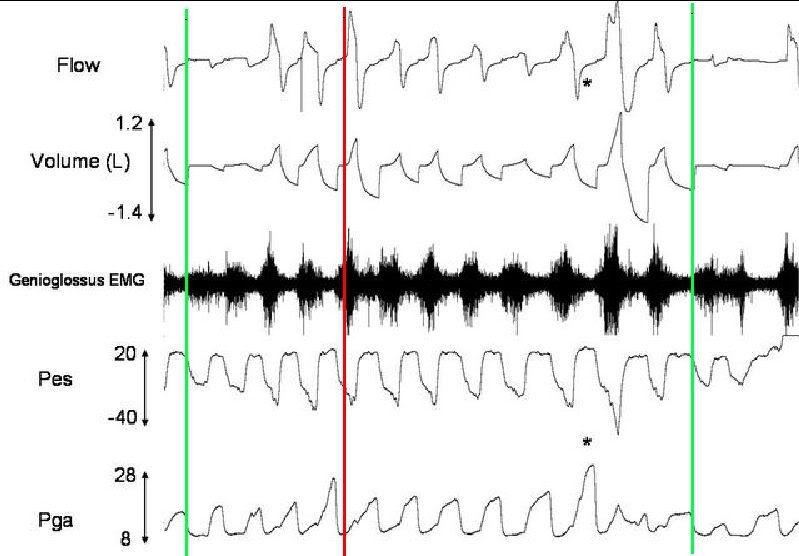
This would better coincide with the GN EMG, end of abdominal effort and VT. I think the baseline Pes is 20 cmH2O also because the tops remain flat even when expiratory flow significantly slows, both in some of the much less aggressive individual breaths and the inherent nature of the latter part of each breath. BTW, did you have inductance plethysmography belts on, and can you find a central apnea or some slow breathing where the breaths don't run into each other somewhere?
Another BTW, if the above patient was on CPAP (I'm thinking he was, cause you seem to have some central stuff there, so he probably needs an ASV anyway)(just kidding), which machine did you use? What you're calling end-expiratory Pes could have been a machine lag if it had a slug-response.
Since your set-up could slam the circuit closed wherever you wanted to, did you slam it shut at end-expiratory 0 CPAP? That would get you iPEEP and you wouldn't have to guess.split_city wrote:NOTE: The difference between peak and end-expiratory Pes is likely to be explained by iPEEP
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Link between OSA and the "beer gut"
That's not actually correct because end-expiratory Pes is negative when an individual is upright, at least in healthy-weight individuals. But for all intensive purposes, end-expiratory Pes is generally not subatmospheric when individuals are in the supine posture. See below table from a study by Steier et al 2009.Muffy wrote:This continues to support my point, that end-expiration in these highly dynamic patients is at the end of the plateau:split_city wrote:Here's another figure taken from Lou et al 2008 again showing an increase in peak Pes during an apnea. Peak Pes was noted to be less than my example.
you can't move it along any further than that because you'd end up with a negative baseline Pes, which is impossible.

No, the patient was not on CPAP. This guy was from my second study, not the abdominal compression study.Muffy wrote:Therefore, in this patient, your high baseline Pes is 20 cmH2O (and not 5 cmH2O), and is contaminated by the CPAP (although these examples are starting to run into each other. Is this patient, in fact, on CPAP?):
Nope, I wouldn't say that red line is where the breath starts. Here's where I think those three breath you identified start. I have also added mask pressure, epiglottic pressure (not the best trace as the catheter is slightly blocked) and a single diaphragm EMG channel. IMO, end-expiratory Pes is still below 10cmH20, and not the peak as you are suggesting.Muffy wrote:I imagine you're calling end-expiratory Pes at the red line, but assuming your signals are synched, I think it would be more appropriately called at the green lines:

Careful, as there is evidence from other studies to suggest that the GG is pre-activated before the onset of flow. Thus, you can't simply go by GG as a surrogate measurement for start of the breath.Muffy wrote:This would better coincide with the GN EMG
Ok, next figure. This clearly shows iPEEP in an obese patient in the supine posture. Peak Pes does not coincide with end-expiratory Pes. This also shows that Pes remains relatively flat during expiration (ignoring cardiac artefact). This is also from the Steier et al paper. This is the reference because you might like to read it if you haven't already: Neural Respiratory Drive in Obesity. Thorax 2009; 64: 719-725.Muffy wrote:...end of abdominal effort and VT. I think the baseline Pes is 20 cmH2O also because the tops remain flat even when expiratory flow significantly slows, both in some of the much less aggressive individual breaths and the inherent nature of the latter part of each breath.

Yes we did have bands on but that data was recorded on a separate system. Two hard to align, sorry. I will need to look for the centrals and/or slow breathing.Muffy wrote:BTW, did you have inductance plethysmography belts on, and can you find a central apnea or some slow breathing where the breaths don't run into each other somewhere?
As stated, patient was not on CPAP in this study.Muffy wrote:Another BTW, if the above patient was on CPAP (I'm thinking he was, cause you seem to have some central stuff there, so he probably needs an ASV anyway)(just kidding), which machine did you use? What you're calling end-expiratory Pes could have been a machine lag if it had a slug-response.
Looks like you are getting confused. Lets get the record straight. This 20cmH20 peak Pes guy was not part of the abdominal compression study. I hope we have cleared that up! Maybe the discussion of this guy should have been left to my other thread so that we could leave this thread for discussion of the abdominal compression study.Muffy wrote:Since your set-up could slam the circuit closed wherever you wanted to, did you slam it shut at end-expiratory 0 CPAP? That would get you iPEEP and you wouldn't have to guess.split_city wrote:NOTE: The difference between peak and end-expiratory Pes is likely to be explained by iPEEP
Muffy
Re: Link between OSA and the "beer gut"
Was that patient upright at the time?split_city wrote:That's not actually correct because end-expiratory Pes is negative when an individual is upright, at least in healthy-weight individuals.
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Re: Link between OSA and the "beer gut"
Muffy wrote:I imagine you're calling end-expiratory Pes at the red line, but assuming your signals are synched, I think it would be more appropriately called at the green lines:
AYFKM? That's exactly where I put my lines. How do you go from the upper graph where it's obviously 20 cmH2O to yours, erase the 20, and arbitrarily say it's 7?split_city wrote:Nope, I wouldn't say that red line is where the breath starts. Here's where I think those three breath you identified start. I have also added mask pressure, epiglottic pressure (not the best trace as the catheter is slightly blocked) and a single diaphragm EMG channel. IMO, end-expiratory Pes is still below 10cmH20, and not the peak as you are suggesting.
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Re: Link between OSA and the "beer gut"
Best. Thread. Ever.
This is one of those threads that I will need to go over and over until my knowledge catches up. I enjoy it much more than the constant kvetching about Evil DMEs. (And I confess, I enjoy DME kvetching too -- it's sorta fun, and makes me feel morally superior to the people on whom I depend for equipment.)
You guys rock. Thanks for providing this level of info, even if I have to sort of pick it up by induction at the moment.
This is one of those threads that I will need to go over and over until my knowledge catches up. I enjoy it much more than the constant kvetching about Evil DMEs. (And I confess, I enjoy DME kvetching too -- it's sorta fun, and makes me feel morally superior to the people on whom I depend for equipment.)
You guys rock. Thanks for providing this level of info, even if I have to sort of pick it up by induction at the moment.
_________________
| Mask: Forma Full Face CPAP Mask with Headgear |
| Additional Comments: First four-hour compliance: Nov 20, 2009 |
-Tom Williams
Re: Link between OSA and the "beer gut"
Muffy wrote:This would better coincide with the GN EMG
I can't stand it! Then you turn around and plop the start of inspiration exactly where I said it should be!split_city wrote:Careful, as there is evidence from other studies to suggest that the GG is pre-activated before the onset of flow. Thus, you can't simply go by GG as a surrogate measurement for start of the breath.
split_city wrote: Here's where I think those three breath you identified start. I have also added mask pressure, epiglottic pressure (not the best trace as the catheter is slightly blocked) and a single diaphragm EMG channel. IMO, end-expiratory Pes is still below 10cmH20, and not the peak as you are suggesting.

Lord, give me strength.
Muffy
________________________________
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Machine: Dell Dimension 8100
Mask: 3M N-95 (during flu season)
Humidifier: Avoided, tends to make me moldy
Software: XP Pro
Additional Comments: You can't find a solution when you don't know the problem
Re: Re:
Does this mean that men are faster to lay down additional VAT (visceral adipose tissue) than women who first add to SAT (subcutanous...)? If so, interesting. Even post-menopausal women are still producing 40-60% of the 3 estrogens compared to pre-menopause production; it's progesterone that falls to ziltch in women (starting at age 35 in Amer & Canadian women, only ones in the study). This book excerpt says that the estrogens and progesterone protect women from sleep apnea: http://books.google.com/books?id=_PhU7g ... 22&f=false. Page 57+ of A Woman's Guide to Sleep Disorders By Meir H. Kryger. Would be interesting to know if the women who have sleep apnea also have reduced levels of these hormones.split_city wrote:...Obese males tend to have greater intra-abdominal pressures versus BMI-matched obese females, again illustrating the difference in fat distribution.
PS If you aren't aware, statins with their potential muscle damage contribute to sleep apnea in some individuals. As you are testing men who have been the targets for statin mfgs, it might be worth gathering that data and determining if muscle weakness from statins might also be contributory...http://www.spacedoc.net/sleep_apnea_statins worth reading as it might impact your research. Read the user posts at that website too; apparently it's more common than the medical field is aware of if these users represent more than a few %s.
ResMed S9 range 9.8-17, RespCare Hybrid FFM
Never, never, never, never say never.
Never, never, never, never say never.
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Link between OSA and the "beer gut"
No they weren't. I was just pointing out that your statement that "negative baseline Pes, which is impossible" maybe confusing to others, unless you mention posture. But lets move on from that shall we?Muffy wrote:Was that patient upright at the time?split_city wrote:That's not actually correct because end-expiratory Pes is negative when an individual is upright, at least in healthy-weight individuals.
Muffy
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Link between OSA and the "beer gut"
Muffy, it's not obvious. I went back to the original sleep file and carefully picked where I thought inspiration started based on flow, mask pressure, epiglottic pressure and diaphragm EMG activity. I haven't put in an arbitrary 7cmH20 because that's the Pes value where the lines are. The scale is quite broad as shown by an earlier snapshot. The Pes where the line is do not coincide with peak Pes.Muffy wrote:Muffy wrote:I imagine you're calling end-expiratory Pes at the red line, but assuming your signals are synched, I think it would be more appropriately called at the green lines:
AYFKM? That's exactly where I put my lines. How do you go from the upper graph where it's obviously 20 cmH2O to yours, erase the 20, and arbitrarily say it's 7?split_city wrote:Nope, I wouldn't say that red line is where the breath starts. Here's where I think those three breath you identified start. I have also added mask pressure, epiglottic pressure (not the best trace as the catheter is slightly blocked) and a single diaphragm EMG channel. IMO, end-expiratory Pes is still below 10cmH20, and not the peak as you are suggesting.
Muffy
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Link between OSA and the "beer gut"
Right I think I know where some confusion lies. Going back to the Steier paper, they have defined their end-expiratory pressure as the peak value. End-expiration does not also equal start of next inspiration, and I think that's where my wires were getting crossed. I originally have been saying that peak Pes doesn't equal end-expiratory Pes, when in fact I should have been saying peak/end-expiratory Pes doesn't equal start of next breath. My apologies. The Pes at start inspiration, in the examples I gave, do not equal peak/end-expiratory Pes values. Do you agree or are you saying that peak/end expiratory Pes is the same as start inspiration values for the next breath?
So yes, end-expiratory Pes is around 20cmH20 but start inspiration values are around 7cmH20. My apologies again! Are you happy with that? But I am a bit confused as to why you didn't pick me up on it when I said "Nope, I wouldn't say that red line is where the breath starts."
. I clearly said where I thought the breaths started, not end-expiratory pressures. But hang on, you said these:
So yes, end-expiratory Pes is around 20cmH20 but start inspiration values are around 7cmH20. My apologies again! Are you happy with that? But I am a bit confused as to why you didn't pick me up on it when I said "Nope, I wouldn't say that red line is where the breath starts."
. I clearly said where I thought the breaths started, not end-expiratory pressures. But hang on, you said these:
Muffy wrote:I imagine you're calling end-expiratory Pes at the red line, but assuming your signals are synched, I think it would be more appropriately called at the green lines:
That's in reference to where those green and red lines are. So you also have said end-expiratory Pes and start of inspiration in reference to the same figure. Are you implying end-expiratory Pes values are the same as start inspiratory values for the next breath? Your first green line is to the right of the peak Pes, so I assume that you're stating end-expiration = start inspiration of next breath??Muffy wrote: "Then you turn around and plop the start of inspiration exactly where I said it should be!"










