Did you mean the image or the report? I don't trust the guys reading it and if you want the actual image I have to go back to the hospital because they missed putting those and my leg doppler on the chest CT disc.Sludge wrote:Want to put up your most recent chest x-ray?nmbugs wrote:I do have the CDs from all my studies and xrays.
Tidal Volume question
Re: Tidal Volume question
_________________
| Mask: Amara View Full Face CPAP Mask with Headgear |
| Additional Comments: SleepyHead Software and CMS50F pulse Ox |
Since my machine doesn't appear to be listed in the selection:
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Re: Tidal Volume question
The report will be fine.
Did you find any hemoglobin and/or Total CO2/HCO3- values?
Do you use a spacer with your MDIs?
How far OT from your original post are we?
Did you find any hemoglobin and/or Total CO2/HCO3- values?
Do you use a spacer with your MDIs?
How far OT from your original post are we?
You Kids Have Fun!!
Re: Tidal Volume question
Hemoglobin 12.9Sludge wrote:The report will be fine.
Did you find any hemoglobin and/or Total CO2/HCO3- values?
Do you use a spacer with your MDIs?
How far OT from your original post are we?
CO2 34 (prior to oxygen therapy it was usually 30-31, so should I be concerned with the increase?)
No HCO3 ever done.
My MPV is always slightly elevated at 9.8 which my hemo doc says that has something to do with my platelets always running a little on the low side but it seems according to the lab here the low values have changed from 150 to 100k so now I am usually in the normal range. I usually run anywhere from 100-130, this last test I was at 135 which is the highest I seem to ever go, thankfully I never go below 100 because that is a therapy I hope I never have to go through!!! It's been a long time since I have seen Dracula aka hemo doc because it's a 8 hour round trip and my platelets seem to be holding their own. Funny though when I lived in Baltimore my doctor said if they stayed in the low hundreds for a few years he would recommend a bone marrow biopsy but here they said it would have to be a lot lower. I have always wondered who is right on that one, frankly though that is a test I don't mind avoiding
I just started using a spacer back in Jan. I didn't know anything about them until I saw the pulm.
We are VERY off topic from the original post. I think I apologized to the boards for just that 20 posts ago
I will get the chest scanned and scan the CT too. In the CT the noticed a small "groundglass opacity" thing but because the biggest was 8mm the doctors have chosen to just watch it. There was also a 3mm nodule right lower lobe. Two subpleural densities medial right lower lobe 4mm and 2mm. 2.5mm subpleural density lateral left lower lobe. Also two or three small increased densities projected along the lumen or right lower lobe pulmonary artery.
I have a bunch of errands I have to do today so I will "scan" those when I get home (which will be late), I really need to get a scanner, the picture phone, converting to pdf, emailing it to myself, etc etc makes it too many dang steps.
Thanks again!
_________________
| Mask: Amara View Full Face CPAP Mask with Headgear |
| Additional Comments: SleepyHead Software and CMS50F pulse Ox |
Since my machine doesn't appear to be listed in the selection:
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Re: Tidal Volume question
Well, "IMHO" we're still doing a lot better than the Fort Hood Shooter and BMI Threads, where inevitably the Gun Nuts and Muscleheads show up.nmbugs wrote:We are VERY off topic from the original post. I think I apologized to the boards for just that 20 posts ago
However, we are about to snap right back on topic.
We can estimate pCO2 using Total CO2 (basically the equivalent of HCO3-) and the Henderson-Hasselbalch Equation. This gives a calculated pCO2 of ~60mmHg (assuming normal pH)! Consequently, a BiPAP approach might be a better plan that CPAP or APAP.
Indeed, you can find a lot of folks who believe asthma is a relative contraindication in asthma. However, if it is closely monitored, it may be helpful.:
http://err.ersjournals.com/content/19/115/39.full
That said, if they just threw you on APAP 6-13, I would not necessarily call that "closely monitored".
You have quite a bit of obstruction and air-trapping on PFT, but since they did not seem to jump on "emphysematous changes", "hyperlucency", "hyperinflation" or even "air-trapping" (although bafflement on that one), and since your diffusion appears to be normal, it would appear that the COPD is of the chronic bronchitis variety.
BTW, what sleeping medication were you on that allowed the AHI to drop? With that degree of CO2 retention, almost any sleeping medication would be contraindicated as it would suppress breathing. It would seem that there may be very little sleep-disordered breathing present present, and this is all chronic respiratory failure, requiring BiPAP to increase your tidal volume.
See?
We're back!
Of course, doesn't mean you can't have both COPD and SDB, and be an "Overlapper", but "IMHO" those "AHI" events were actually period of hypoventilation (by definition of period of (greater) increased pCO2.
BTW, have any headaches? That tends to be a sign of increased pCO2.
You Kids Have Fun!!
Re: Tidal Volume question
I am working on getting all those reports up for you now. I found something interesting in one report, I didn't mention it before because I totally disregarding the echo my pulm did because my cardo said without "tissue doppler" it was worthless. Anyways I decided to google what the heck the chiari network in the right atrium was since nobody ever brought it up. Then I found this and about swallowed my tongue:Sludge wrote:Possibility?nmbugs wrote:I mentioned to him about the right to left cardiac shunts and he said that could be a possibility.
http://www.ncbi.nlm.nih.gov/pubmed/22893767Here, we evaluate the prevalence of right-to-left shunting (RLS) through transcranial Doppler ultrasound (TCD) in a large patient group with obstructive sleep apnea (OSA).
METHODS:
One hundred consecutive patients (mean age 59.5 y) with OSA underwent TCD with intravenous injection of agitated saline. The grading of right-to-left-shunts was in accordance with the Spencer PFO Grading Scale.
RESULTS:
RLS was detected in 72 of 100 patients (72%). Thirty-four out of these 72 patients (47%) had a shunt grade I or II; 15 (21%) had a shunt Grade III or IV; and 23 (32%) had a large shunt (Grade V or V+). In 47 of 72 patients (65%), a right-to-left shunt was detectable at rest without Valsalva maneuver.
Chiari's network was present in 29 of 1,436 patients (prevalence 2%). A frequently associated finding was a patent foramen ovale in 24 (83%) of the 29 patients with Chiari's network versus 44 (28%) of 160 control patients (p < 0.001). Intense right-to-left shunting occurred significantly more often in patients with Chiari's network than in control patients (16 [55%] of 29 patients vs. 19 [12%] of 160 control patients, p < 0.001). Another frequent association was an atrial septal aneurysm in 7 (24%) of 29 patients. The indication for transesophageal echocardiography was a suspected cardiac source of arterial embolism in 24 (83%) of 29 patients with a Chiari net, 13 of whom (54%) had recurrent embolic events. Chiari's network was significantly more common in patients with unexplained arterial embolism than in patients evaluated for other indications (24 [4.6%] of 522 patients vs. 5 [0.5%] of 914 patients, p < 0.001). Potential causes for arterial embolism were present in 9 of the 24 patients with a Chiari net and embolic events (atrial septal aneurysm in 7, cerebrovascular lesion in 2). In 15 (62%) of 24 patients only a patent foramen ovale could be identified. Three patients had deep venous thrombosis and pulmonary embolism at the time of arterial embolism; none had a thrombus detected within the network.
http://content.onlinejacc.org/article.a ... id=1166352
There is that right to left shunt thing you were talking about. Now the doc who read this echo he didn't note a shunt but the evaluation was limited due to poor subcostal window, whatever the heck that means!
Okay let me get to work on getting this docs uploaded and linked for you. Thanks again for everything. I have a bunch of questions for you on the bipap but I will ask them tomorrow.
_________________
| Mask: Amara View Full Face CPAP Mask with Headgear |
| Additional Comments: SleepyHead Software and CMS50F pulse Ox |
Since my machine doesn't appear to be listed in the selection:
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Re: Tidal Volume question
5-13 CT https://docs.google.com/file/d/0B-ELU_v ... YyUTQ/edit
12-13 ECHO non-doppler https://drive.google.com/file/d/0B-ELU_ ... BpYjQ/edit
12-13 CT https://drive.google.com/file/d/0B-ELU_ ... 1Lc3M/edit
1-14 Chest xray https://drive.google.com/file/d/0B-ELU_ ... h6R2M/edit
The one thing that keep irritating me, and maybe I am wrong in my thought and the doctors are right. They keep saying the size of my pulmonary artery could be just congenital large. Then when I ask well if it's congenital then why has it grown larger in just 6 months. Both said the same thing, well 29mm to 32mm isn't that much growth. I am thinking 3mm in 6 months while it is small considering it's an artery that can only expand so much, any enlarging should point to something. If it was a congenital defect it wouldn't have enlarged would it? My sleep doc thought was that was why the second radiologist measured the other artery to see if it was a congenital defect.
I wish my dang doctors would put their heads together and consult with one another, none of them know what the other is doing and it's getting so frustrating. I know NJ will be able to figure it out but I am still trying to figure out how I am going to pull off that trip. I wish they could just get it together here so I didn't have to spend all that money going out of state.
The link you posted about positive pressure, I found this interesting (and once again made me ): "We do not recommend the use of CPAP alone without pressure support in asthma as this mode is in effect external PEEP, which is mainly used for improving oxygenation. As CPAP has no pressure support it does not possess the added benefit of increased ventilation. Adding pressure support to CPAP increases tidal volume and helps to unload fatigued respiratory muscles [51, 52]. Therefore, we recommend the use of commercially available NPPV circuits or ICU ventilators with pressure support."
So "mainly used for improving oxygenation" would that mean being able to get off of oxygen eventually? That would be wonderful!!!!
The other question I have is the fatigued respiratory muscles, would that cause hypoventilation? The reason I ask is because when I use my portable oxygen concentrator it alarms on me all the time because apparently I am not taking deep enough breaths for the unit to know I am breathing in and send me that burst of oxygen. My home unit is continuous flow so I don't get those alarms unless I am wearing my new CMS50f and my oxy alarms is going off. I guess, maybe I am having apneas during the day, if that is possible? The resp tech who set me up on my machine was shocked that none of my doctors have sent me for resp therapy.
The medication I was on was seroquel and one doctor I spoke with (hospital doc not my personal doc) had a fit that I was given that for insomnia saying it was extremely dangerous off label use of that medication and that there have been a few (very rare) documented cases of that drug causing PAH in a few patients. I have to wonder if my CO2 had improved since I stopped taking that medicine, I know my AHIs have reduced...hmmm.
Many many thanks again!
Well I am going to try to get some sleep.
12-13 ECHO non-doppler https://drive.google.com/file/d/0B-ELU_ ... BpYjQ/edit
12-13 CT https://drive.google.com/file/d/0B-ELU_ ... 1Lc3M/edit
1-14 Chest xray https://drive.google.com/file/d/0B-ELU_ ... h6R2M/edit
The one thing that keep irritating me, and maybe I am wrong in my thought and the doctors are right. They keep saying the size of my pulmonary artery could be just congenital large. Then when I ask well if it's congenital then why has it grown larger in just 6 months. Both said the same thing, well 29mm to 32mm isn't that much growth. I am thinking 3mm in 6 months while it is small considering it's an artery that can only expand so much, any enlarging should point to something. If it was a congenital defect it wouldn't have enlarged would it? My sleep doc thought was that was why the second radiologist measured the other artery to see if it was a congenital defect.
I wish my dang doctors would put their heads together and consult with one another, none of them know what the other is doing and it's getting so frustrating. I know NJ will be able to figure it out but I am still trying to figure out how I am going to pull off that trip. I wish they could just get it together here so I didn't have to spend all that money going out of state.
The link you posted about positive pressure, I found this interesting (and once again made me ): "We do not recommend the use of CPAP alone without pressure support in asthma as this mode is in effect external PEEP, which is mainly used for improving oxygenation. As CPAP has no pressure support it does not possess the added benefit of increased ventilation. Adding pressure support to CPAP increases tidal volume and helps to unload fatigued respiratory muscles [51, 52]. Therefore, we recommend the use of commercially available NPPV circuits or ICU ventilators with pressure support."
So "mainly used for improving oxygenation" would that mean being able to get off of oxygen eventually? That would be wonderful!!!!
The other question I have is the fatigued respiratory muscles, would that cause hypoventilation? The reason I ask is because when I use my portable oxygen concentrator it alarms on me all the time because apparently I am not taking deep enough breaths for the unit to know I am breathing in and send me that burst of oxygen. My home unit is continuous flow so I don't get those alarms unless I am wearing my new CMS50f and my oxy alarms is going off. I guess, maybe I am having apneas during the day, if that is possible? The resp tech who set me up on my machine was shocked that none of my doctors have sent me for resp therapy.
The medication I was on was seroquel and one doctor I spoke with (hospital doc not my personal doc) had a fit that I was given that for insomnia saying it was extremely dangerous off label use of that medication and that there have been a few (very rare) documented cases of that drug causing PAH in a few patients. I have to wonder if my CO2 had improved since I stopped taking that medicine, I know my AHIs have reduced...hmmm.
Many many thanks again!
Well I am going to try to get some sleep.
_________________
| Mask: Amara View Full Face CPAP Mask with Headgear |
| Additional Comments: SleepyHead Software and CMS50F pulse Ox |
Since my machine doesn't appear to be listed in the selection:
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Re: Tidal Volume question
Former smoker?
How many packs per day did you smoke? For how many years?
How many packs per day did you smoke? For how many years?
You Kids Have Fun!!
Re: Tidal Volume question
Yes. 1/2 - 3/4 a pack. How many years? That's a hard one. I would smoke for 2 years get pregnant and quit for 5 years then get under some sort of severe stress and start smoking again. I quit 3 years ago and have NO intention to ever touch another one.Sludge wrote:Former smoker?
How many packs per day did you smoke? For how many years?
The other thing is, my doctors always dismiss this because testing for it was so poor in 1983. When I was 13, I was really sick and in the hospital for a long time. Breathing problems of all kinds, lungs, sinuses etc. What it eventually came down to was I had a ton of nasal and sinus polyps. They also treated me for histoplasmosis but back then the only histo test was like a skin allergy type test which docs today say wasn't reliable. I grew up in central Fl and spent a lot of time in swampy areas with my dad, so who knows. Interesting though when my doctor tested me for everything but normal blood work he ran an IgG kit (something once again my other doctors say was worthless) and guess what was high in that test? My doctor was sure I had birds, even implied I was lying and I must have birds...lol. I was like look birds are one animal I would never have for fear of histo! But after that nothing else was ever said about it.
I also forgot, you asked about headaches. No, the only time I get headaches now is my migraines or if my oxygen line has a break, gets twisted and kinked or a dog/kid/husband trips on my hose and yanks it out of my unit. I don't notice it's gone til the headache hits (if sitting down) or until I get up, move around and can't breathe. I need to pay better attention to my body and when I am sitting and start having problems not dismiss it and keep going (which seems to happen a lot when I can't find a cause until I eventually find the crack in the hose).
_________________
| Mask: Amara View Full Face CPAP Mask with Headgear |
| Additional Comments: SleepyHead Software and CMS50F pulse Ox |
Since my machine doesn't appear to be listed in the selection:
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Re: Tidal Volume question
To answer your question on number of years total, it looks like 8-10 yrs. It makes me sick that I ever picked it up again after stopping the first time and going 11 years without a smoke! I hope that isn't the cause of all this now, I am sure it didn't help whatever is happening. All the docs know that history but really didn't say anything except ask if I will smoke again.
Oh and my doctor has order blood gases test. She said to leave my oxygen on for the tests. I was going to get the paperwork and test today but have a horrible migraine so I will have to try to do it tomorrow. I will let you know those results as soon as I get them back. Will that test indicate anything about the RLS? The reason I ask is because my pulm said that the cardio should have done blood gases during the cath to diagnosis RLS.
Thanks again!
Oh and my doctor has order blood gases test. She said to leave my oxygen on for the tests. I was going to get the paperwork and test today but have a horrible migraine so I will have to try to do it tomorrow. I will let you know those results as soon as I get them back. Will that test indicate anything about the RLS? The reason I ask is because my pulm said that the cardio should have done blood gases during the cath to diagnosis RLS.
Thanks again!
_________________
| Mask: Amara View Full Face CPAP Mask with Headgear |
| Additional Comments: SleepyHead Software and CMS50F pulse Ox |
Since my machine doesn't appear to be listed in the selection:
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Re: Tidal Volume question
I think if it shows a low pO2 that is unexplainable, then the R>L Shunt door remains open.nmbugs wrote:Will that test indicate anything about the RLS?
To look for PFO (quick, cheap and easy), you really to do
- Transcranial Doppler (TCD); or
- Transesophageal Echocardiogram (TEE)
You Kids Have Fun!!
Re: Tidal Volume question
What time of day are these migraines? Are they really "migraines"?nmbugs wrote:...the only time I get headaches now is my migraines...
However, an interesting bit of trivia that can be used to feed this Syllogistic Diagnostic Approach:
http://www.americanheadachesociety.org/ ... chwedt.pdf
You Kids Have Fun!!
Re: Tidal Volume question
It's funny you ask that question. Back in 1994 I had jaw surgery, mandibular osteotomy, for TMJ that was triggering daily horrid migraines. After that surgery I went without a migraine until 5 years ago. About a year ago I kept telling my doctor these migraines are different. They don't respond to my migraine meds, even when I do into a dark quiet room my head is still pounding and the only way to get any pain off my eyes is to apply pressure to them (with my fingers I literally apply pressure to the eyeballs, usually it is always the left that needs that kind of pressure though). One in particular was so bad I went to the ER because it wasn't like my typical migraines. I am not keeping a headache journal (I know BAD on me, will start one) so I don't remember now what the difference was that made me go to the ER, which I typically don't do for migraines.Sludge wrote:What time of day are these migraines? Are they really "migraines"?nmbugs wrote:...the only time I get headaches now is my migraines...
However, an interesting bit of trivia that can be used to feed this Syllogistic Diagnostic Approach:
http://www.americanheadachesociety.org/ ... chwedt.pdf
Like I said I don't keep a journal and my memory SUCKS so I will start one now and keep better track. I can tell you for sure the one that hit yesterday hit soon after I got up and the one I got Sat I was just sitting down crocheting a hat. Back to yesterday I was just sitting at my computer checking emails. I had not eaten breakfast yet or taken a shower, it's spring break so I was having a lazy day. Nothing worked on the migraine. I didn't have any maxalt on hand but that hasn't been working all the great anyways so I took fioricet. Five fioricets later my migraine was "liveable" and my eye pain was way better, well at least I wasn't having to try any press it into my brain .
Now here is a question. When I went to a knew neurologist about 5 years ago for my fibro and migraines so he did a MRI. He said the MRI showed a TIA. When trying to get my records I found out he read the reports himself and the state closed him down for failure to keep proper patient records so no report. The best I can do is get the CD of the MRI but not sure if that does me any good since I don't have anyone right now who can read it. Since my neuro lost his license my PCP has taken over my pain management treatment (ie has kept me on the same meds he had me on). So was it really a TIA? I don't know. Besides his failure to keep patient records he seemed to know what he was doing
_________________
| Mask: Amara View Full Face CPAP Mask with Headgear |
| Additional Comments: SleepyHead Software and CMS50F pulse Ox |
Since my machine doesn't appear to be listed in the selection:
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Re: Tidal Volume question
Stupid question time. One thing that has the doctors stumped (I lie, everything has this docs .....), is my edema. My edema is severe, even on water pills but only in one leg. My right leg from the knee down is double sometimes triple the other leg. Any of these problems you have brought up would cause edema on one side of the body only? It feels like I am retaining fluid in my stomach but nobody seems to be concerned about that. Towards the late afternoon I get this strange sensation in the center/ towards left side of my chest. It feels like tingling/burning. It doesn't hurt but it feels really weird and I swear at those times I am filled with fluid. My pulm dismissed it as heartburn but it sure as heck doesn't feel like that, I don't have an acid rising up and tums doesn't make it stop, so I don't know. My right leg always hurts so bad too. I think it's from the constant fluid buildup. I am taking potassium and the pain isn't cramps either. Maybe it's just my fibro making the water retention hurt so badly. It has been 3 months since my leg was normal size. In the beginning it would swell for a few days and go away then come back but this last round it hasn't gone away, well except after my cath when I was able to spend a day in bed but as soon as I started moving around again it blew right back up.
_________________
| Mask: Amara View Full Face CPAP Mask with Headgear |
| Additional Comments: SleepyHead Software and CMS50F pulse Ox |
Since my machine doesn't appear to be listed in the selection:
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Re: Tidal Volume question
I'm thinking it's time you found a new hobby.
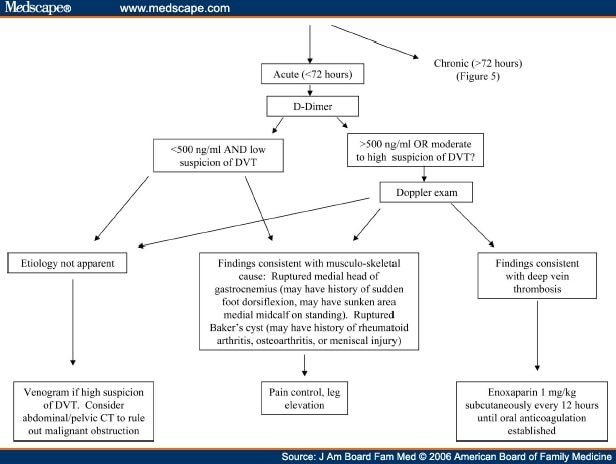
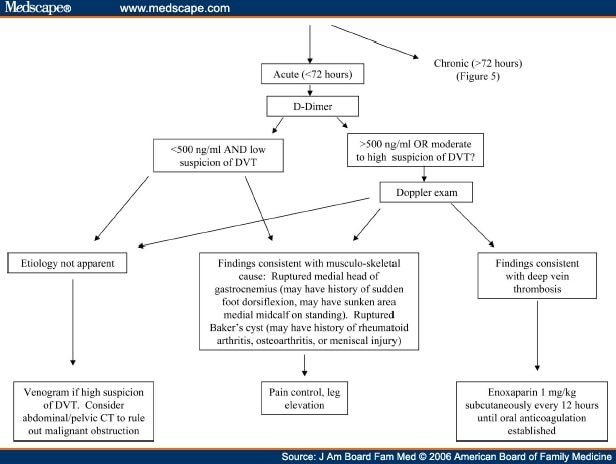
Figure 4: Unilateral Edema.
http://www.medscape.com/viewarticle/524606_1
BTW, how'd the blood gas turn out?
Figure 4: Unilateral Edema.
http://www.medscape.com/viewarticle/524606_1
BTW, how'd the blood gas turn out?
You Kids Have Fun!!
Re: Tidal Volume question
Tell me about it, I want my photography back! I miss taking pics of spiders and other creepy thingsSludge wrote:I'm thinking it's time you found a new hobby.
Figure 4: Unilateral Edema.
http://www.medscape.com/viewarticle/524606_1
BTW, how'd the blood gas turn out?
https://www.flickr.com/photos/8506937@N ... 1918136237 Just in case you don't like spiders I linked you to a cute insect
I haven't gone for my blood gases yet. Yesterday was just a horrid day all around. If I am able to get some sleep I hope to go today. It's a bad night with my leg. My doc did a sono of my ab/pelvic but not CT and nothing was found, this was about 4-5 months ago.
_________________
| Mask: Amara View Full Face CPAP Mask with Headgear |
| Additional Comments: SleepyHead Software and CMS50F pulse Ox |
Since my machine doesn't appear to be listed in the selection:
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals
Resmed Aircurve 10 ASV w/ humidifier and climate line tubing w/ 2L O2. Just restarted therapy after stopping bipap for 1 yr due to complications w/ increased centrals










