OK, but asthma is a disease of exhalation, and these numbers:nmbugs wrote:Let me see if I can explain why my SOB doesn't feel like asthma....
First I don't wheeze and second the SOB starts to happen upon exhale not inhale. Because I cannot exhale all the air in my lungs I cannot inhale. Again there is no wheezing and the pain in my chest is on exhale then not being able to empty my lungs out I cannot take enough air in.
Code: Select all
Spirometry:
Pre: Post:
FVC 2.23 2.57
FEV1 1.14 1.27
FEV1/FVC% 51 49
FEF25-75% 0.37 0.36
PEF 3.50 3.79
However, we can call that "unresponsive obstruction".
BTW, is your FVC normal? What is your age and height:
http://www.cdc.gov/niosh/topics/spirome ... lator.html
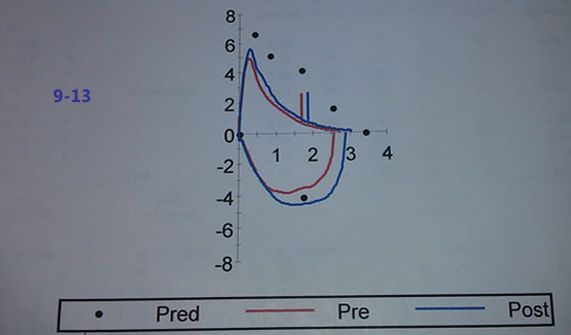
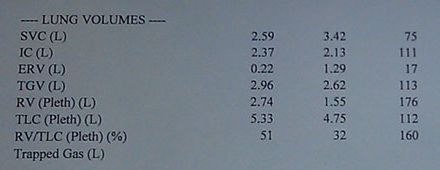
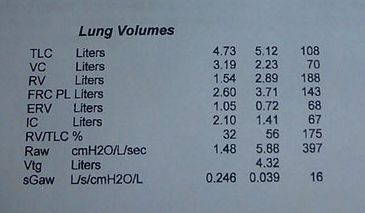
Can you upload the PFT results (you can upload the document to Dropbox, GoogleDocs, etc.) to look at the Flow-Volume Loops and Volumes (RV) to see if there are any clues there?