Sludge wrote:nmbugs wrote:Sludge wrote:nmbugs wrote:Also hemoglobin at what time?
At the time they did the diffusion.
Sorry, I am confused. In diffusion you mean prior to the PFT. Do they typically do blood at the same time?
I meant prior to diffusion part of the test, which was the one where you held a deep breath for about 10 seconds before you exhaled. The maneuver should have been repeated several times. One needs to correct for abnormal hemoglobin. Also, one needs to be OFF oxygen for at least 15 minutes, so never mind, it's all messed up anyway.
My heart cath that was done here the doctor was in and out in 5 min. National Jewish has everything broken down from prep to med time to procedure time then recovery. They have my cath lasting 2 hours.
The cath lab report could be looked at to see what was done, but it could have been all they did was a Right Heart Cath, but even that takes longer than 5 minutes. Maybe you had a little Happy Juice on board. At any rate, sounds like NJ is doing R&L.
Spirometry:
FVC Pre: 2.23 Post 2.57
FEV1 Pre: 1.14 Post 1.27
FEV1/FVC% Pre: 51 Post: 49
FEF25-75% Pre: 0.37 Post: 0.36
PEF Pre: 3.50 Post: 3.79
FIVC Pre: 1.69 Post: 2.09
Diffusion:
DLCO 23.7
DL adj 22.1
DLCO/VA 5.76
DL/VA Adj 5.37
VA 4.12
IVC 2.28
BHT 12.95
This looks like unresponsive asthma (you got the bronchodilator and didn't improve an iota). What kind(s) of drugs are you/have you been on? Did you try all these:
http://www.mkh-medicine.com/presentatio ... o/001.ppt
The wheezing could have driven up the diffusion.
α1-antitrypsin deficiency?
Are you a BOOP? That's almost like winning Lotto.
Meta:
http://www.cmaj.ca/content/182/1/45.full
They did test for α1-antitrypsin mutation and that was negative.
This has been the frustrating thing. My first pulm was like this is just all asthma and I told him, I have had asthma since I was 18 and this is not asthma. He put me on a crap load of expensive COPD meds which did nothing but make my lungs feel like they were on fire! Yes I still have asthma attacks and when I have them my rescue inhaler medicine helps. I still have asthma attacks while on oxygen (which he tried to say oxygen helps asthma, which I haven't noticed any damn difference in number of occurrences- which really are not that many). My shortness of breath happens when I move about or just sitting and off of oxygen for an extended period of time. It just takes a little walking without oxygen to make it drop. Asthma medicine doesn't help that SOB (I tried that before I got on oxygen where I was using my inhaler like 15 times a day!) but if I sit down the SOB gets better within a few minutes. My saturations will start to go back up but will still stay in mid 80s (again without oxygen). I never had an asthma attack where sitting for 3-5 minutes stopped the SOB (not wheezing btw you should have heard my quack pulm explain why with "this asthma" I wasn't wheezing, I about fell out of my chair!) Anyway that's why my PCP put me on oxygen in the first place, because it wasn't my asthma.
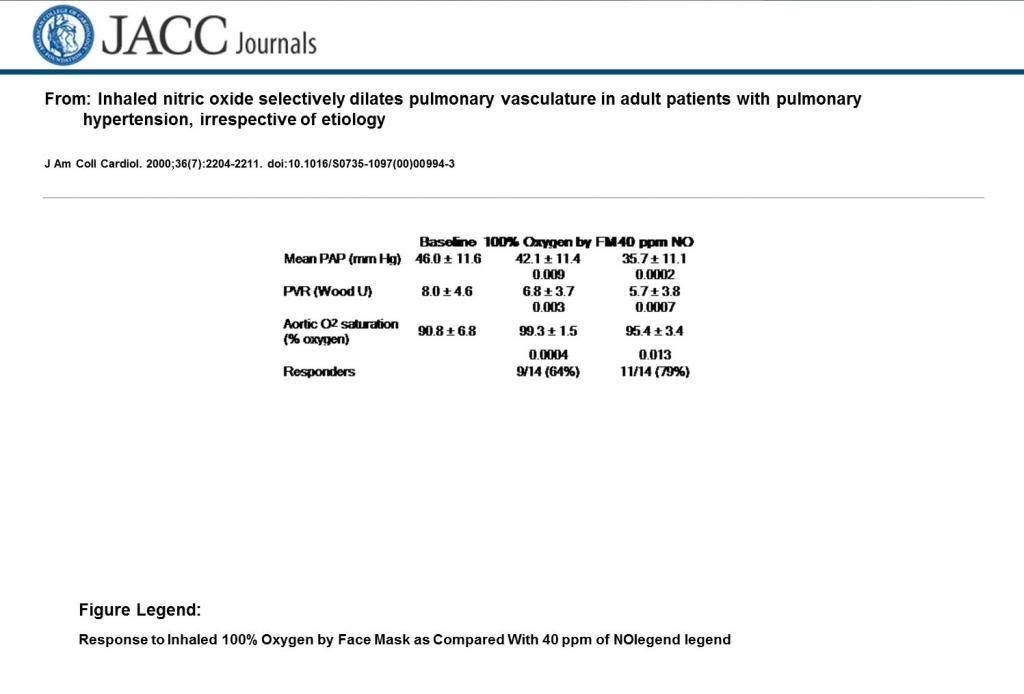
I did find this interesting from that article: "64% of patients were responders (≥20% decrease in mean PA pressure or ≥20% decrease in PVR) to 100% oxygen". So I wonder what my Mean pulm pressure would have been had he left the damn oxygen off? Grrrr, this makes me so mad. If NJ gets a different result I am going to fight the doc and hospital over their charges. Neither my insurance or me should be responsible for that payment. Oh and the reason the 5 minutes sticks in my mind is because the nurses were congratulating the doc for such a "record" cath. This of course didn't account for the prep time and med, that took about 30 min. After they put me on the table and he numbed my leg from that time to the time he pulled out the cath it was 5 min!
As for BOOP, nobody has ever done a biopsy and nothing has shown up on xrays that are suggestive of it, or at least nobody has suggested it.
I really appreciate all your help. I have learned so much more about these tests and my lungs just in these last few days from info you posted. I am always scared to be proactive in my health because then I feel like a hypochondriac or afraid the docs will think I am. However it seems if you are not knowledgeable in tests and what they mean you just might end up, well to put it nicely, messed up. Like my new pulm said "your pulmonary artery can only stretch so far"! I just hope this last screw up didn't take a lot of time off my life , trying to stay positive and not think like that but I have my bad days and today is one of those days.
Anyways I hope you have a wonderful weekend, sorry for being a bummer.