Okay. Let's take a quick peek at
why that added sensitivity offered by the proximal sensor line is important to the ASV algorithm. First let's review text from the ASV Fact Sheet (with an emphasis on the underlined parts):
Resmed Technology Fact Sheet wrote:To determine the degree of pressure support needed, the ASV
algorithm continuously calculates a target ventilation. Based on
respiratory rate and tidal volume, the target is 90% of the
patient’s recent average ventilation—that means that ventilation
can vary gradually and naturally over the course of the night.
The algorithm uses three factors to achieve synchronization
between pressure support and the patient’s breathing.
1. The patient’s own recent average respiratory rate—including
the ratio of inspiration to expiration and the length of any
expiratory pause.
2. The instantaneous direction, magnitude, and rate of change of
the patient’s airflow, which are measured at a series of set
points during each breath.
3. A backup respiratory rate of 15 breaths per minute.
To ensure ventilatory support is synchronized to the patient’s effort,
the VPAP Adapt SV relies on factors one and two. When a central
apnea/hypopnea occurs, support initially continues to reflect the
patient’s recent breathing pattern. However, as the apnea/hypopnea
persists, the device increasingly uses the backup respiratory rate.
From the above disclosure we know that the ASV algorithm relies heavily on measuring and comparing set points with respect to instantaneous direction, magnitude, and rate of change. Now that's what the ASV algorithm does by design. So please don't confuse that disclosure with the issue of whether SAG approves or disapproves of those algorithmic steps, or which Resmed employee SAG thinks released that information to the public.
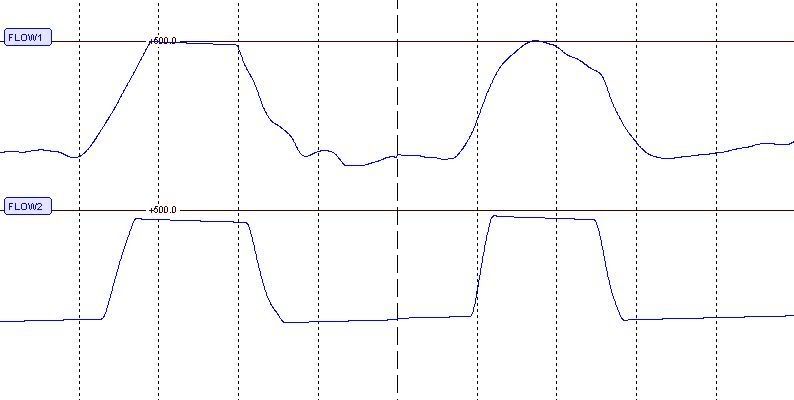
The ASV algorithm is comparing a series of reference points that look something like this:

Now here's a nice chart recently posted by SAG that shows significant degradation of a flow signal measured at the machine (flow2) compared with that same patient flow signal more accurately measured at the mask (flow1):
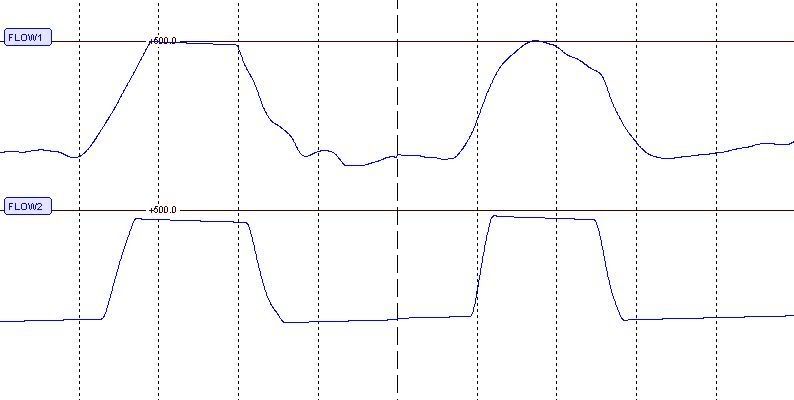
So the left two signal humps look similar because they are comprised largely of machine effort rather than human effort. But look at those right two humps. They differ quite a bit. The top hump in particular, flow1, is comprised from significant human inspiratory effort. That top hump much better reflects human inspiratory
instantaneous direction, magnitude, and rate of change that the ASV algorithm relies on for its comparative calculations.
It's
human inspiratory effort that the ASV tries to accurately baseline, compare, and correct on an as-needed basis. And if you're working with a series of flow-curve reference point comparisons (
minute volume) and your algorithm is design-bound to compare those points, then the top signal via a proximal sensor line is really what you want---because signal processing itself manages to retain many more of those crucial comparison reference points. Now if your algorithm endeavors to slide respiration rate (also known as patient-variable "F") back and forth,
preservation of those signal processing sample points becomes even more mathematically crucial.
So let's take yet another look at that
bottom-right signal hump labeled flow2.
It's flat. How is the ASV algorithm going to determine its top-most three crucial reference points with that signal source? Now sample at the mask with a proximal sensor line and you get that more-suitable top-right signal hump labeled flow1. With
that signal source the ASV algorithm can now more readily ascertain samples for its three top-most reference points (in order of appearance): 1) early mid-inspiration, 2)peak flow (top- and center-most reference point), as well as 3) late mid-inspiration. Some of the other reference points now sample and signal-process more accurately as well. You can see how this reference-point-driven ASV algorithm really needs that extra transient-signal sensitivity achieved via a proximal sensor line at the mask.
By contrast Respironics compares only peak flow (the top of each signal hump). And unlike Resmed, Respironics does not attempt to
adjust patient-variable "F" (Respironics only endeavors to back up respiration).That means
no need to compare instantaneous direction or rate of change of the flow curve itself. That also means
no need for a proximal sensor line in the Respironics case. As a side note, fixed or constant impedance can be algorithmically baselined without a proximal sensor line--very satisfactorily. Narrow-diameter proximal sensor lines are always about increasing sensitivity to
dynamics or transients embedded in a signal stream.
Thanks to SAG who originally provided us with the above Resmed text and two graphs.