BarryKrakowMD wrote:My experience also tells me why the comment about ENT is generally untrue, unless we're talking about some superstar ENT surgeon who has developed techniques that are as yet unpublished. The ENT track record in predicting changes in RDI (apneas + hypopneas + flow limitations) following surgery are abysmal. In fact, ENT predictions on baseline diagnostic RDIs are frequently inaccurate as well. We can all agree I think that part of the problem lies in the absurd way in which SDB events are measured. Nonetheless, a purported ENT model, let's say using a "collapsible tube" analogy is highly flawed when it comes to predicting SDB events with precision, because the airway is so much more complex and dynamic.
I showed this comment to one of the ENT surgeons, whom we affectionally call "Luca" (because of the strong resemblance to the character Luca Brasi in "The Godfather") and he seemed to take exception to it. He became quite agitated, his singular giant eyebrow became furrowed and his eyes narrowed as he said, "
Meet Krakow.
Eat Krakow". Don't worry, tho, we hit him with the tranquilizer gun, and I'm sure he'll be fine when he wakes up.
Let us not dismiss these thoughts:
SAG wrote:A visit to a good ENT guy will go a long way in helping to identify structure that could result in fixed flow limitation. There are also objective testing methods of assessing nasal airflow. And the analysis of flow volume loops in the PFT lab may be helpful in "looking" at areas that cannot be seen directly.
with this generalization:
BarryKrakowMD wrote:My experience also tells me why the comment about ENT is generally untrue, unless we're talking about some superstar ENT surgeon who has developed techniques that are as yet unpublished. The ENT track record in predicting changes in RDI (apneas + hypopneas + flow limitations) following surgery are abysmal. In fact, ENT predictions on baseline diagnostic RDIs are frequently inaccurate as well. We can all agree I think that part of the problem lies in the absurd way in which SDB events are measured. Nonetheless, a purported ENT model, let's say using a "collapsible tube" analogy is highly flawed when it comes to predicting SDB events with precision, because the airway is so much more complex and dynamic.
There are a number of different anatomical structures that contribute to airway patency, some of which may be treated with pressure approach, some of which may not (fixed obstructions). If your measuring methodology is composed of nasal pressure transducer during diagnostic testing, the effect of nasal airway narrowing (if present) will be included in the waveform. If you're using nasal interface during pressure titration, nasal narrowing now becomes a significant contributor to that waveform. And you're not going to change that waveform, that patency a heckuva lot by increasing or decreasing pressure. Further, the contributions of these "upper" upper airway structures can be assessed by a good ENT guy, or in your own garage using rhinomanometry. Once identified, a different treatment approach should be considered. It may be as simple as using a ResMed Mirage Quattro FFM and Breathe Right Nasal Strips, or perhaps surgical intervention may help.
BarryKrakowMD wrote:Regardless, I still have trouble with what I understand to be SAG's points, because they either are exquisitely reductionistic or they are being communicated in reductionistic ways.
I must go head-to-head with this assessment, and resort to the "I-know-you-are-but-what-am-I?" debating strategy.
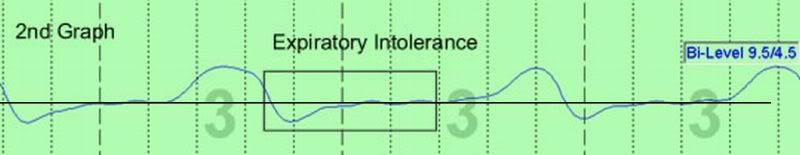
I respectfully submit that basing treatment approach on this singular event
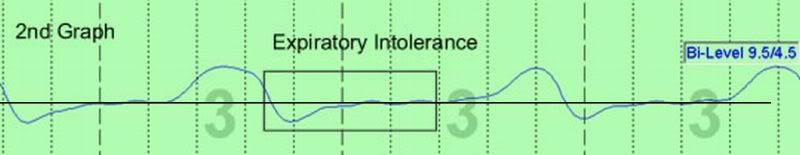
is "reductionalistic". It not only fails to take into account the numerous previously mentioned forces, but is highly susceptible to artifact. And again, looking at those other channels will be able to give us a much better idea of the contribution of these other factors.
SAG