Absolutely, Expiratory Intolerance is different than Expiratory Flow Limitation. I don't think I said otherwise, but sorry if I'm causing that confusion.
An FLE event whether on inspiration or expiration should mean the airway experiences resistance. Using the standard collapsible cyclinder/tube analogy, with UARS we expect to either see a slight narrowing of the tube diameter or if this is not visible, then dynamically, we expect there to be measurable resistance likely caused by some change in the tension in the airway dilator muscles, which prevents air from passing through the tube as smoothly as in a normal breathe. Again, you can develop this problem on inspiration or expiration.
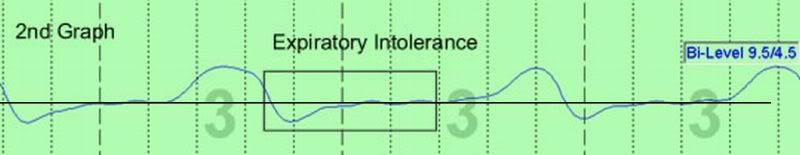
Expiratory intolerance suggests the the wall of the tube is fluttering or wobbly or doing something dynamically that appears to indicate (in our experience) that the patient is fighting the
incoming pressurized airflow while trying to breathe
out. Expiratory intolerance has been called expiratory instability by our group in the past, but after having done a more careful reading of older literature, I realized that the term "instability" has been used by many pulmonologists to describe the collapsibility of the airway, that is, an unstable airway is one that is prone to SDB events, etcs.
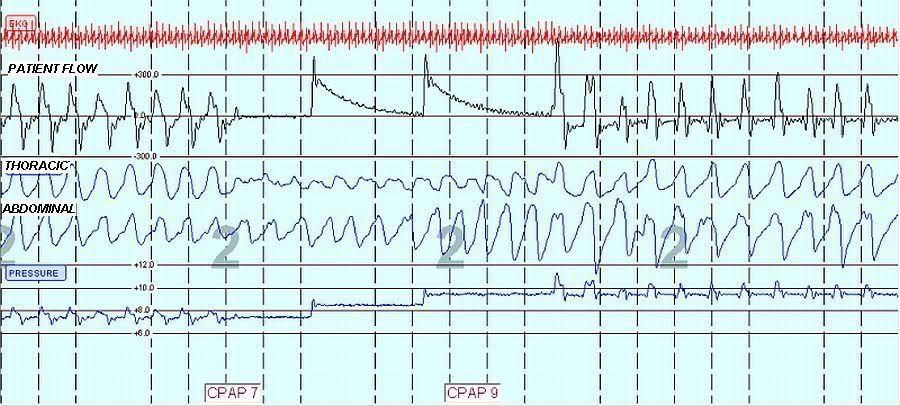
Any flow limitation event requires higher pressure, higher CPAP, IPAP, or EPAP, because you are trying to splint the airway open. but on expiration as CPAP pressure goes higher, it causes the wobbly airway, indicating the high pressure is making the airway intolerant to the process. In my clinical experience, although I concur that many variables influence the process, the single most constant variable that predicts this problem is anxiety in general or just a report of initial discomfort from the patient when using CPAP while awake during the initial desensization prior to the start of the titration. By the way,patients report the cessation of this discomfort when switched to bilevel, again while awake. Then, of course, during the titration and the night of sleep, you can still see the intolerance crop up from time to time on expiration, which is a cue to the sleep tech to drop CPAP pressure, switch to bilevel, or if on bilevel, drop EPAP.
Now, an incredibly key aspect of this phenomenon is whether or not you think the patient is going to adapt to the sensation of pressurized airflow during that first titration or whether it will take several weeks or months to do so, or will the patient always suffer too much anxiety to ever be able to use PAP therapy effectively. Thus, it is not at all uncommon to see a patient return for a full night bilevel titration a month or two later, and both IPAP and EPAP can be raised (as individually indicated to normalize the inspiratory or expiratory flow curve) to new pressures, and the patient reports having slept better that very morning compared to all their sleep experiences in the prior month of PAP use. Which really means that they had diminished their intolerance problem and were ready to test out higher pressures. In my opinion, this finding technically means that they needed higher pressure at the first titration, but it would have been impossible to have them use such pressure due to intolerance.
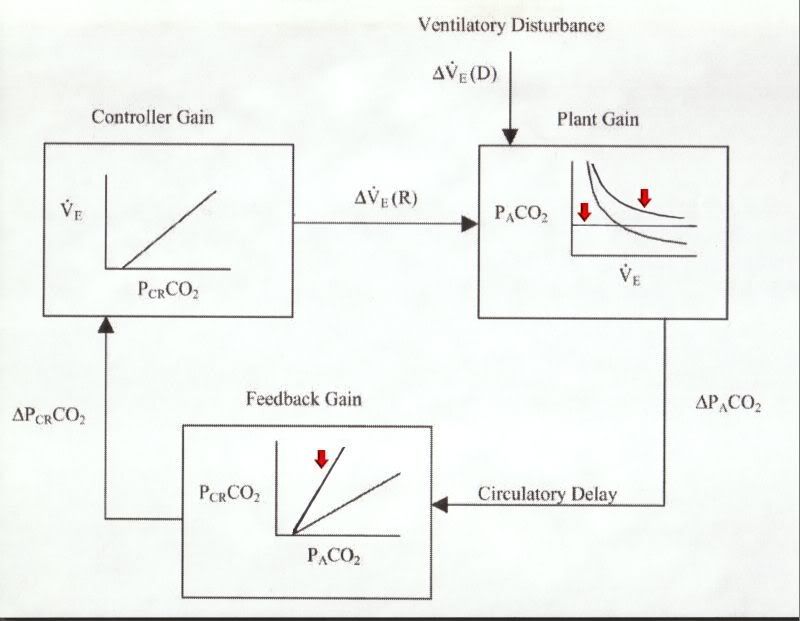
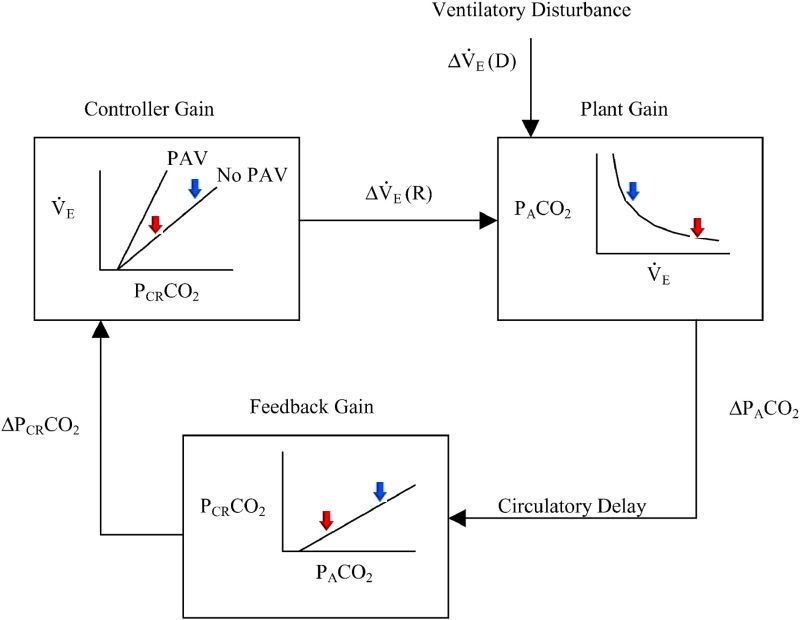
Does expiratory intolerance precede central apneas? Absolutely. It is one of the most common findings in a sleep lab. It may be more generally perceived as pressure that is too high, because all sleep techs report the finding of "pressure was raised, central apneas developed, so pressures was dropped." But, if you consider the distinctive feelings of inspiration and expiration, it is certainly easier to adapt to a feeling of high air pressure coming in when you breathe in than it is to adapt to high pressure when you breathe out, so the more common antecedent to a central apnea would be predicted to be during expiration. Are some of these centrals related to loop gain and changes in CO2? While the answer is probably yes in some cases, this type of central might also be primarily mechanical forces at work: you don't like the feeling of pressurized air, so you "check" your breathing (as you might when sticking your head out the window of a rapidly moving vehicle).
Last, for now, many pulmonologists are quick to state that patients are "passive" to the experience of PAP therapy while asleep, that is, they believe the patient does not experience emotional responses to it. I strongly disagree and always counter with our common experiences in REM sleep, namely dreaming and the enormous emotional responses we have to our dreams. I remain convinced, at this point, that anxious patients tend to bring their anxiety with them into the sleep state, and expiratory intolerance manifests when a threshold of discomfort is crossed between level of pressurized air and level of comfort in breathing out against that pressurized air. Remarkably, I encounter at least 25% of our patients who "think" they are
not anxious, but who really suffer significant anxiety, yet because their TFI System (thoughts, feelings, images) is so out of balance, they do not know how to recognize or measure anxiety (see posts on the topic "Dr. Krakow's book" regarding emotional processing or hey, buy the book
Sound Sleep, Sound Mind at
http://www.sleeptreatment.com.
P.S. I find 120 sec epochs much less clarifying that 30 second epochs, especially if you are trying to spot the subtle bumpiness of intolerance.
P.S.S. Don't think it's cardiac oscillations linked to intolerance, but I will try to find another epoch in coming weeks to verify and demonstrate.