ASV Titration Help Request
Re: ASV Titration Help Request
AVS and John,
I understand that the S9 does not actually treat Central apneas, but it does seem that it can prevent them to some extend. Since using my S9 my Centrals have gone down significantly with a corresponding decrease in my symptoms. The other day with the AHI of 0.7 I felt very good. I also look, usually daily and in detail at the Flow tracings that the S9 generates. It clearly indicates when CSR is present and when it isn't. And I have seem a great decrease in true CSR as well as a CSRish pattern (when the crescendo decrescendo isn't so pronounced as to actually produce a Central apnea). So my experience, and I think the data I have back up that the S9 has helped tremendously.
I'd describe it this way, that the S9 prevents CSR (which is intermittent in my case) from getting carried away and self- perpetuating. What I don't know is if this decrease in Centrals and CSR would have a significant positive impact on left ventricular ejection fraction--that the Adapt SV can achieve. In one of the papers that John linked, there was mention of improved left ventricular function with CPAP, so I should think this means that the S9 could have that same potential, at least for a specific individual (although I can't know if I am that lucky individual or not).
And I am trying different pressures to see if I can come up with something that seems to work. Please see my next post which is actually a draft I wrote prior to answering this. It is the best description of my experience that I can come up with right now. When the Adapt SV doesn't work for me, the negative symptoms are significant. I would really like to find a way for the Adapt SV (or failing that the BiPAP autoSV) work for me. But the bottom line if that I have to feel better and not worse. I find myself wondering if that 90% downward trending ventilation function has something to do with it (although my subjective sense is that I am being over-ventilated.) I just know that I've never felt as good on the Adapt SV as I have on the S9.
Please understand that I am not trying to be argumentative, rather I am trying to understand my condition as well as to communicate accurately about it. I truly appreciate the information and input.
I understand that the S9 does not actually treat Central apneas, but it does seem that it can prevent them to some extend. Since using my S9 my Centrals have gone down significantly with a corresponding decrease in my symptoms. The other day with the AHI of 0.7 I felt very good. I also look, usually daily and in detail at the Flow tracings that the S9 generates. It clearly indicates when CSR is present and when it isn't. And I have seem a great decrease in true CSR as well as a CSRish pattern (when the crescendo decrescendo isn't so pronounced as to actually produce a Central apnea). So my experience, and I think the data I have back up that the S9 has helped tremendously.
I'd describe it this way, that the S9 prevents CSR (which is intermittent in my case) from getting carried away and self- perpetuating. What I don't know is if this decrease in Centrals and CSR would have a significant positive impact on left ventricular ejection fraction--that the Adapt SV can achieve. In one of the papers that John linked, there was mention of improved left ventricular function with CPAP, so I should think this means that the S9 could have that same potential, at least for a specific individual (although I can't know if I am that lucky individual or not).
And I am trying different pressures to see if I can come up with something that seems to work. Please see my next post which is actually a draft I wrote prior to answering this. It is the best description of my experience that I can come up with right now. When the Adapt SV doesn't work for me, the negative symptoms are significant. I would really like to find a way for the Adapt SV (or failing that the BiPAP autoSV) work for me. But the bottom line if that I have to feel better and not worse. I find myself wondering if that 90% downward trending ventilation function has something to do with it (although my subjective sense is that I am being over-ventilated.) I just know that I've never felt as good on the Adapt SV as I have on the S9.
Please understand that I am not trying to be argumentative, rather I am trying to understand my condition as well as to communicate accurately about it. I truly appreciate the information and input.
Re: ASV Titration Help Request
I gave this a try recently, the only difference being that the Adapt limits EEP + PS to 20, so at the EEP of 8 it limited max PS to 12.guestASV wrote:On the Resmed unit... set your EEP @ 8, min PS @ 3; Max PS @ 15 and let it roll. You cannot self titrate on an ASV as every night will be different due the Cheyene Syocks Respirations. The reason you have these CSR is a CO2 imbalance.
I slept on my back for the whole night and it was a fairly rough night. I just don't do well trying to get to sleep on my back. But I can deal with that. I also wore my oximeter and glanced at it at various times as I tried to get to sleep as well as the times I woke up during the night. Often my O2 levels were reported at 97-98 with it seldom going lower than 95 for the entire night. The software reported my Basal SpO2 at 96.2 and that only 1.2% of the time did it go below 95%. So it seems I was very well oxygenated--and I wonder if that means over-oxygenated. The Adapt SV onscreen data was the following (although I don't know the significance) Average Pressure 9.6 VT 245-826, MV 4-19, Resp Rate 11-15, and leak rate was described as Very Good but showed 23/Lmin.
Does anyone know how the Average Pressure is calculated--if it is the average between adding the EEP and the average inspiration pressure divided by time throughout the night? (Which on an EEP of 8 with a minimum PS of 3 (so 11as min inspire.) would lead to an absolute minimum average pressure of 9.5. If that is the case then my data of 9.6 means I was very close to the minimum values all night long.
Subjectively the greatest difficulty is that I felt weird the next day. The symptoms that go with "weird" were an unusual stiffness at the upper neck and very base of my skull. I also have a slight sensation of a band around the top of my head (going around my head 360 degrees above the level of the temples.
But the primary symptom and most troubling symptom was an internal sense of "depletion." The depletion seemed to worsen as the day went on. By the evening I noticed an unusual breathing pattern where I seemed to take a quick breath in and quick breath out--sort of like panting but without the breath rate being elevated. And on the exhale it was sort of like my breathing was collapsing. I had a sense of being fairly exhausted. After doing some seated meditation in the evening I seemed to regain my internal balance. On waking and for awhile thereafter I also had a sense that I had been "over-breathed"--sort of a combination of over ventilated and having the muscles associated with breathing being over worked.
Now this "weird" sensation is exactly what I felt on my initial use of the Adapt SV when I had the EEP at 4, min PS 3 and max PS at around 15. Each day of use in that trial I seemed to go downhill until I was very, very depleted.
So normally I'd say that this trial with the higher pressure didn't work for me. But when I hooked myself to my EKG, it seemed that my HR was lower (which if true is very good for me). The next night I went back to my S9 and my AHI was 0.7 with CSA of 0.2, OSA 0.0 and HI of 0.4. My Flow graphs showed very little CSR. My pressure was also lower with median 5.4, 95th 6.3 max 7.4. And I felt very good all day.
There are so many variables to account for but maybe something good happened with the Adapt SV, once I got balanced out, which took a 2nd day/night.
The last time I consistently used the Adapt SV it seemed like I progressively went downhill each day. It might be unorthodox but I am thinking to alternate between the Adapt SV and the S9 for a bit to see if I can ease into this.
- JohnBFisher
- Posts: 3821
- Joined: Wed Oct 14, 2009 6:33 am
Re: ASV Titration Help Request
ldj325, you are doing exactly what researchers have found works as well as a full blown titration - using a methodical trial and error approach. It is quite possible that just be keeping your airway open, it helps your body avoid the "run away" CSR issues. The S8 and S9 after that were built on lessons learned while creating the VPAP Adapt SV unit. My understanding is that the S9 is one of the best machines in that it is very easy to breathe with it. This decreased resistance would definitely help someone like you, who might "fall off the edge" when there is increased resistance to breathing. So, I speculate that between the improved airway and the easier breathing, you are attaining better consistent respiration.
And it is your methodical approach that makes a difference. You take careful notes, trying over and over - so you can provide consistent results (and not just an occasional aberration). This will allow you - in spite of limited funds - to find a solution that works best for you.
And as you've seen, though we can provide our own experience and thoughts, you will need to sort through your situation and discover what works for you.
But, you definitely have our best wishes as you continue your journey!
And it is your methodical approach that makes a difference. You take careful notes, trying over and over - so you can provide consistent results (and not just an occasional aberration). This will allow you - in spite of limited funds - to find a solution that works best for you.
And as you've seen, though we can provide our own experience and thoughts, you will need to sort through your situation and discover what works for you.
But, you definitely have our best wishes as you continue your journey!
_________________
| Mask: Quattro™ FX Full Face CPAP Mask with Headgear |
| Additional Comments: User of xPAP therapy for over 20 yrs. Resmed & Respironics ASV units with EEP=9cm-14cm H2O; PSmin=4cm H2O; PSmax=15cm H2O; Max=25cm H2O |
"I get up. I walk. I fall down. Meanwhile, I keep dancing” from Rabbi Hillel
"I wish to paint in such a manner as if I were photographing dreams." from Zdzisław Beksiński
"I wish to paint in such a manner as if I were photographing dreams." from Zdzisław Beksiński
Re: ASV Titration Help Request
John,
Thank you for your kind words. I know that a certain amount of trial and error is required. I wish I had more data on the Adapt SV to quide me, But that is just not the case with my original model. And until I can get some indication that that the Adapt SV can work for me, even if I had the money, I'd be hesitant to buy the Enhanced model. So trail and error is all I have. I have added oximeter information to my data to try to figure out what is happening, but I either have an oximeter that is not accurate enough or I just haven't had enough data to establish a trend yet. (i am often in the 94-95 % and occasionally drop down to 93% average. It may be that my body produces symptoms at 93% vs high 94s-95s. I just cant say yet.)
This is for everyone so please don't feel I am directing it at you specifically as I know you are busy. And I'm sure everyone has been busy with the end of Summer, start of school and digging out from the holiday.
I've had a number of questions that have gone unanswered. If anyone who is knowledgeable with the Adapt SV would feel more comfortable in answering via PM the please do so. I have wanted to keep this public for the benefit of others, but I don't want to limit the information coming to me. (And I've seen that several comments have come in from quest posters which seems to indicate some anonymity is desired.) I am still trying to figure out why my symptomatic response to the Adapt SV is so poor. I've tried low pressures (EEP 4.0), then a higher pressure (EEP 8.0) and then a middle pressure (EEP 6. while side sleeping only. I have given up on any idea or sleeping on my back for now and all future attempts will be on side sleeping only.
I've never received any answer to my early question of the S9 data indicating a median pressure of 5.6, meaning 1/2 the time I'm below that pressure with a lot of time around 4.8--5.2 if the Adapt SV is just too much pressure I suppose leading the pressure induced Centrals.
Alternatively I've looked at the whole downtrending of 90% of the prior 3 minutes minute ventilation average. Could it be that this drives my CO2 too high and results in the negative symptoms I experience? Does anyone know if this downtrending process continues to occur even in the absence of CSA or CSR. Per my S9 data I'm not having a lot of CSR these days.
Per this reference that I think you or SWS sent me: http://www.sleepcenters.us/adaptive-ser ... hen-brown/ "At its core, the Adapt SV is a highly evolved bilevel device. The IPAP is variable and responds rapidly within 2 or 3 breaths to significant changes in patient tidal volume. When patient tidal volume increases, the device IPAP decreases. When patient tidal volume decreases, the device IPAP increases. Thus the marked fluctuations in patient tidal volume that characterize complex sleep apnea are attenuated and usually the tidal volume is stabilized by the device.
A longer-term correction is effected by the trailing 3-minute memory of minute ventilation and pattern of breathing. After a 3-minute initial collection period, the Adapt SV then sets a minute-ventilation target that is 90% of the previous minute volume. Hence there is a weak downward force on total minute-ventilation that nudges the PCO2 upward 2 or 3 millimeters of mercury, decreasing or eliminating the frequent CO2 dips below the apnea threshold that drives the central events. Because of this 90% target, the manufacturer cautions that the device should not be used in patients who have a condition that might result in hypoventilation."
In the meantime I will keep hunting to see if I can find a "sweet spot" with the Adapt SV.
Thank you for your kind words. I know that a certain amount of trial and error is required. I wish I had more data on the Adapt SV to quide me, But that is just not the case with my original model. And until I can get some indication that that the Adapt SV can work for me, even if I had the money, I'd be hesitant to buy the Enhanced model. So trail and error is all I have. I have added oximeter information to my data to try to figure out what is happening, but I either have an oximeter that is not accurate enough or I just haven't had enough data to establish a trend yet. (i am often in the 94-95 % and occasionally drop down to 93% average. It may be that my body produces symptoms at 93% vs high 94s-95s. I just cant say yet.)
This is for everyone so please don't feel I am directing it at you specifically as I know you are busy. And I'm sure everyone has been busy with the end of Summer, start of school and digging out from the holiday.
I've had a number of questions that have gone unanswered. If anyone who is knowledgeable with the Adapt SV would feel more comfortable in answering via PM the please do so. I have wanted to keep this public for the benefit of others, but I don't want to limit the information coming to me. (And I've seen that several comments have come in from quest posters which seems to indicate some anonymity is desired.) I am still trying to figure out why my symptomatic response to the Adapt SV is so poor. I've tried low pressures (EEP 4.0), then a higher pressure (EEP 8.0) and then a middle pressure (EEP 6. while side sleeping only. I have given up on any idea or sleeping on my back for now and all future attempts will be on side sleeping only.
I've never received any answer to my early question of the S9 data indicating a median pressure of 5.6, meaning 1/2 the time I'm below that pressure with a lot of time around 4.8--5.2 if the Adapt SV is just too much pressure I suppose leading the pressure induced Centrals.
Alternatively I've looked at the whole downtrending of 90% of the prior 3 minutes minute ventilation average. Could it be that this drives my CO2 too high and results in the negative symptoms I experience? Does anyone know if this downtrending process continues to occur even in the absence of CSA or CSR. Per my S9 data I'm not having a lot of CSR these days.
Per this reference that I think you or SWS sent me: http://www.sleepcenters.us/adaptive-ser ... hen-brown/ "At its core, the Adapt SV is a highly evolved bilevel device. The IPAP is variable and responds rapidly within 2 or 3 breaths to significant changes in patient tidal volume. When patient tidal volume increases, the device IPAP decreases. When patient tidal volume decreases, the device IPAP increases. Thus the marked fluctuations in patient tidal volume that characterize complex sleep apnea are attenuated and usually the tidal volume is stabilized by the device.
A longer-term correction is effected by the trailing 3-minute memory of minute ventilation and pattern of breathing. After a 3-minute initial collection period, the Adapt SV then sets a minute-ventilation target that is 90% of the previous minute volume. Hence there is a weak downward force on total minute-ventilation that nudges the PCO2 upward 2 or 3 millimeters of mercury, decreasing or eliminating the frequent CO2 dips below the apnea threshold that drives the central events. Because of this 90% target, the manufacturer cautions that the device should not be used in patients who have a condition that might result in hypoventilation."
In the meantime I will keep hunting to see if I can find a "sweet spot" with the Adapt SV.
Re: ASV Titration Help Request
Hello again, ldj325... I'd like to go back to the top of your thread and work my way down with comments. But before I do, let's visit this important post:
Also, I have some layperson speculation about generalized thoracic/neck "fluid loading" here:
viewtopic.php?f=1&t=47180&p=425332&hili ... ng#p425332
I'll also point out that the Remed Adapt SV requires an extended period of time in which the algorithm adapts to or "reads" the patient before settling into a more comfortable routine. You might try your Respironics BiPAP AutoSV set up essentially the same way as your Resmed---for a side-by-side comparison---to see if the Respironics algorithm just so happens to suit you better. The Respironics algorithm does not have that initial algorithmic adaptation phase that some patients just so happen to find uncomfortable.
More later...
And I'd like to pull these excerpts from your above post for further discussion:ldj325 wrote:(This member posts from this thread have brought up a number of things. I can't address them all at once, but I have not forgotten the comments about the thyroid issue and the sleep surface or the suggestion about the ASV trial pressure.)
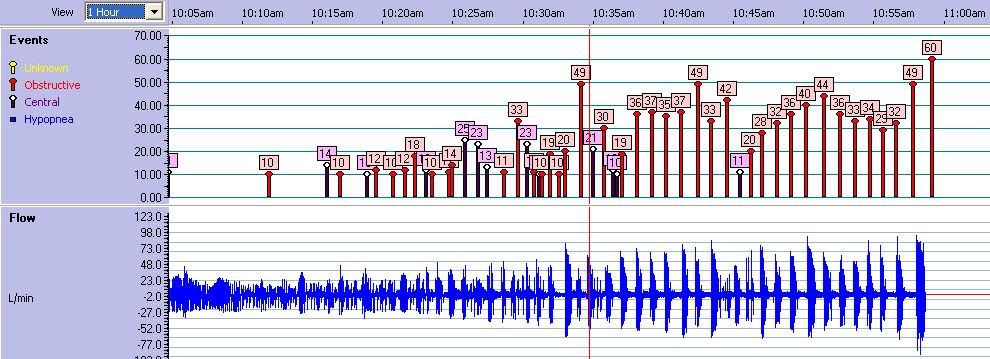
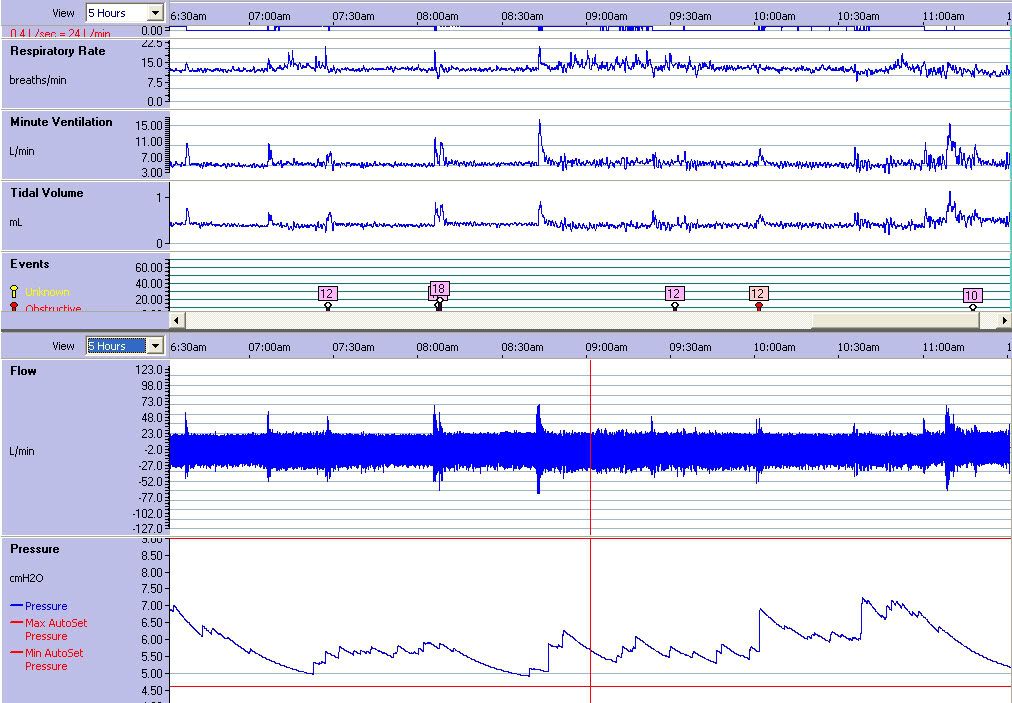
Upddate on my Average stats: Update Averages 5/21-9/6/2010 AHI 2.3, CA 1.6, OA 0.2, HI 0.4 Pressure Median 5.6, 95th 7.1, Max 8.2
As is evident by the OA of 0.2 my issue has predominantly been Central apneas. Then on 9/3 I had a long meditation session and the last 40 minutes it looks like I dropped off to sleep. Recently the S9 has shown that I haven't done well when in seated meditation which is why I tried on the back.
And I got this data which is what caused me to come unglued with frustration, especially since for many years meditation has been a place of renewal for me.
(Click on graphs to expand)
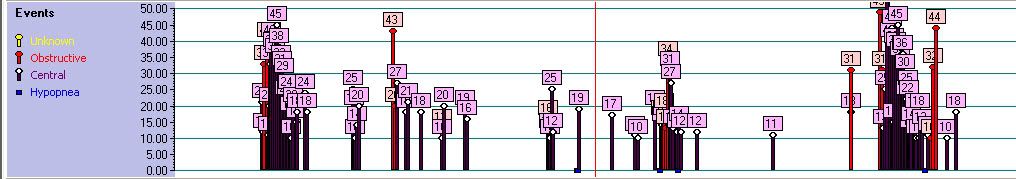
I have never before seen me have anything more than a smattering of OA. The few times I've slept on my back it typically looked like this:
It has taken me awhile to figure out why I would go from predominantly CA to such a run of OA. From the first week on the S9 I'd seen that I didn't do well on my back. So I have trained myself to sleep on my sides only, except in rare instances. So my average stats are largely based on sleeping on my sides. And with side sleeping I have consistently cut my autoset range down from 4-20 initially gradually to my current range of 4.4-9.
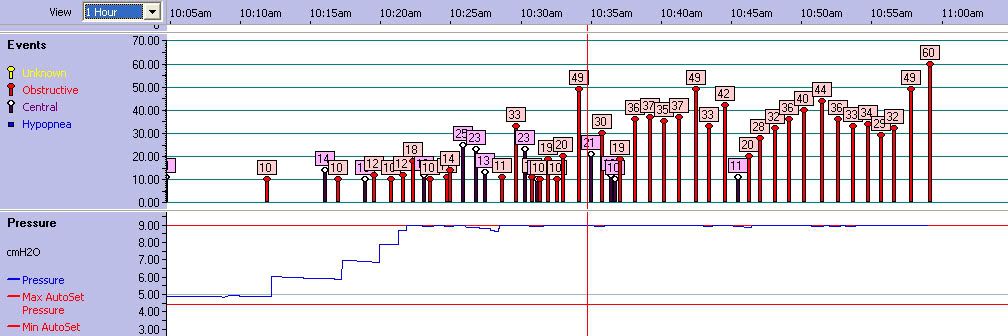
What I didn't realize this past Saturday is that I've never tried being on my back with the more narrow range. Which resulted in this:
So it looks to me like the S9 topped out in pressure but it wasn't enough to prevent the OA while on my back. At least knowing this makes it not seem so crazy to me. Does this line of reasoning seem plausible to you more experienced members?
Now that leads me to question if I'm like 2 people in terms of needed therapy. One is side sleeping where it seems like the 4.4-9 range on the S9 works pretty well. I know that the 4.4 is low, but I've looked extensively at my detailed pressure tracings at times when there are no events and I seem to be resting well. And I've seen that I spend a lot of time in the upper 4s and low 5s. This seems supported by the Median Pressure Average of 5.6. I also tried raising the lower end to 5.0 and I got aerophagia and didn't seem to do well. Similarly after my titration study I narrowed my range to 7-9 (since I was titrated for 8.0) but again I did not do well.
And with the Adapt SV even starting at 4.0 with a a minimum pressure support of 3 it provided a minimum on inspiration of 7.0--and again I seemed to be getting too much air. I am thinking that this is the case for side sleeping. And if that is the case then it doesn't seem like the Adapt SV can work for me--unless my my understanding of how the Adapt works or my reasoning is faulty. Can someone knowledgeable comment on this?
On the other hand, when sleeping on my back it seems that I need greater pressure and in that instance the Adapt SV was set too low in terms of EEP. This then brings into question the comment by the sleep tech after my titration study (which was primarily done on my back) who said they did not get me effectively titrated for the BiPAP autoSV (Respironics Omni-lab) as I kept going from the OA into CA.
Is there any ASV machine that could go low enough and not over aspirate me while on my side and still go higher for when I'm on my back?
I think that's an entirely reasonable hypothesis. We might also wonder what causes your night-to-night variability regarding closure severity or required pressure. Sleep position is one possibility as you noted. I'm under the impression---as the rank layperson that I am---that pulmonary edema can conceivably contribute. Supposedly "cardiac asthma" occurs as bronchospasms that are secondary to pulmonary congestion/edema. I'm thinking that one possibility is that "cardiac asthma" type obstructions can register on your S9 as ordinary apnea obstructions. I don't think the S9 would have the ability to differentiate those two types of airway obstructions: bronchial occlusion versus upper airway occlusion.So it looks to me like the S9 topped out in pressure but it wasn't enough to prevent the OA while on my back. At least knowing this makes it not seem so crazy to me. Does this line of reasoning seem plausible to you more experienced members?
Also, I have some layperson speculation about generalized thoracic/neck "fluid loading" here:
viewtopic.php?f=1&t=47180&p=425332&hili ... ng#p425332
Well, you can see from this search link that aerophagia is a big challenge for many people here: search.php?keywords=aerophagia. Different aerophagia countermeasures seem to work for different people. Some people double their pillows, for instance, so that their chin tucks forward---thereby positioning their LES to maintain better closure. Others require chin pointed up and back as they sleep, similar to the CPR chin position. Unfortunately, both of your ASV models require that exhale pressure be high enough to adequately address your obstructive apneas. You should not use fluctuating IPAP to address your obstructive apneas according to either ASV manufacturer protocol. The ASV's fluctuating IPAP is essentially supposed to be reserved for central undershoot, including central apneas and central hypopneas. Obstructive hypopneas can optionally be addressed with either exhale pressure or a minimum/base IPAP.Now that leads me to question if I'm like 2 people in terms of needed therapy. One is side sleeping where it seems like the 4.4-9 range on the S9 works pretty well. I know that the 4.4 is low, but I've looked extensively at my detailed pressure tracings at times when there are no events and I seem to be resting well. And I've seen that I spend a lot of time in the upper 4s and low 5s. This seems supported by the Median Pressure Average of 5.6. I also tried raising the lower end to 5.0 and I got aerophagia and didn't seem to do well. Similarly after my titration study I narrowed my range to 7-9 (since I was titrated for 8.0) but again I did not do well.
I'll also point out that the Remed Adapt SV requires an extended period of time in which the algorithm adapts to or "reads" the patient before settling into a more comfortable routine. You might try your Respironics BiPAP AutoSV set up essentially the same way as your Resmed---for a side-by-side comparison---to see if the Respironics algorithm just so happens to suit you better. The Respironics algorithm does not have that initial algorithmic adaptation phase that some patients just so happen to find uncomfortable.
I suppose it's possible that a BiLevel IPAP of 7cm is too much for you, but that would be rare. It's also possible that the Adapt SV algorithm somehow isn't quite right for your particular breathing pattern. Another reason to at least try your Respironics ASV machine is that you can run it with min PS at 0cm. That would be servo-ventilation applied on top of CPAP as base therapy (instead of required BiLevel as base therapy---as in the Resmed ASV case). And If it just so happens to turn out that your Respironics machine works surprisingly well for you, whereas the Resmed did not by comparison, then you will know not to keep the Resmed.And with the Adapt SV even starting at 4.0 with a a minimum pressure support of 3 it provided a minimum on inspiration of 7.0--and again I seemed to be getting too much air. I am thinking that this is the case for side sleeping. And if that is the case then it doesn't seem like the Adapt SV can work for me--unless my my understanding of how the Adapt works or my reasoning is faulty. Can someone knowledgeable comment on this?
More later...
Re: ASV Titration Help Request
-SWS,
Thanks for the detailed reply. There is a lot to digest, I especially liked some of the links especially the Circulation Overview of OSA and CSA in heart disease (excellent summary for anyone interested). I scanned it but will need to print that out and reread to fully digest it.
Fortunately I have never before seen anything like that run of OSA, even on my first sleep study where I spent a lot of time on my back (although not much sleeping) or my titration study. The titration study was also largely on my back, but I was hooked up to CPAP so I'm thinking that controlled a lot of the apnea. Although the tech did make that comment that they couldn't get me titrated with ASV due to a combination of limited time and the fact that as my centrals were handled I went into OSA.
Whatever the case, as a pragmatic approach I haven't slept or napped on my back since. One episode of 21 minutes of apnea in 47 minutes convinced me t0 let that "dream" go. Fortunately recently I have hit upon a good pressure with my alternating pressure mattress that has allowed me to side sleep exclusively without getting excessive pressure point pain. I still get some and I suspect it is causing some arousals but it is manageable.
As for pulmonary edema, my cardiologists have listened to my lungs several times and haven't heard obvious edema. As I understand it there can still be interstitial edema that might be a factor--and it's just currently relatively mild state. As for the rest of me I only have very mild ankle edema. Still something has caused my primarily CSA (as I'm primarily side sleeping) and the OSA when I'm on my back. Your comments here in one of the links was very interesting because of the intermittent aspect that I haven't considered before:"In summary: If left-heart insufficiency causes intermittent pulmonary edema, then intermittent central SDB can occur; if left-heart insufficiency leads to intermittent tissue edema in the upper thoracic/neck area, then obstructive SDB can, at least in theory, be intermittently exacerbated."
I imagine the whole thing about the fluid loading could relate to what I eat or drink, and especially salt which I am very sensitive to. Unfortunately it is too far back for me to remember specifics about how much fluid I might have been retaining. But in the future I'll try to pay more attention
I read a bit on cardiac asthma and it doesn't sound like my symptoms.
The aerophagia hasn't been as bad as on my original trial with only mildly elevated pressure IPAP 5.0. Last night with the EEP at 7.6 I had some, but it was manageable.
Regarding this statement: "I'll also point out is that the Remed Adapt SV requires an extended period of time in which the algorithm adapts to or "reads" the patient before settling into a more comfortable routine." Does "the extended period of time" mean later in the same night or does it refer to a multi-night learning period. If it is multi-night then I've probably not given it enough time. Also when I first got the machine I erased all previous data (except total hours of usage which can't be erased). I am hoping that the Adapt has started fresh with me and is not carrying over some learning from the prior owner. Do you (or anyone who might be reading) know about this?
The great difficulty for me is that I have never had a good night on the Adapt SV and most were I felt quite poor. I have been experimenting with EEP pressure to see if I could find one where I could tolerate it well. I did very poorly in my side-sleeping at EEP 4.0 and back sleeping at 8.0 (which was my titrated CPAP back sleeping pressure). So more recently, thinking that side sleeping would possibly require less pressure I tried 6.8 (not great subjectively but the oximeter averaged 95% for the night) then 7.4 (subjectively better) and recently 7.6. At 7.6 I felt the best for most of the time. But I awoke and found my CMS 50F pulse oximeter reading SpO2 of 74% (whereas always before the Adapt SV has seemingly boosted night average SpO2). At the same time I looked at my onscreen data and saw that my RR was 26. That's more than twice my normal resting rate. And in the morning my EKG seemed to indicate a somewhat elevaton over my norm, And while there has been a progressive improvement,I still experience a overall negative and nowhere near as good as I feel on the S9 (where my recent AHI has been 1.0 with very little evidence of CSR.
My subjective sense as I am going to sleep is that the RR that the Adapt wants to maintain is too fast for me. And I've watched the screen sometimes and it often wants to keep me around RR 18. I've been able a few times to sort of trick the Adapt so that the RR comes down to about 15, which feels better to me. But I have to be looking at the screen to do this.
I am a little suspicious of the CMS 50F for me due to the fact that it can't keep pace of my true pulse rate. Still obviously there was something going on because of the arousal and the decreased O2 reading and the very elevated RR. I have decided to replace the CMS 50F (which I think for most folks is a great bang for the buck oximeter) with the SPO7500 in the hopes that the later will be more sensitive to HR changes and hopefully more sensitive to O2 desaturations as well.
My evaluation period is coming to an end fairly soon with the Adapt SV, so my focus is on figuring out if the Adapt can work for me or not. But maybe I can give the Respironics a try this weekend just to experience the difference.
Best regards.
Thanks for the detailed reply. There is a lot to digest, I especially liked some of the links especially the Circulation Overview of OSA and CSA in heart disease (excellent summary for anyone interested). I scanned it but will need to print that out and reread to fully digest it.
Fortunately I have never before seen anything like that run of OSA, even on my first sleep study where I spent a lot of time on my back (although not much sleeping) or my titration study. The titration study was also largely on my back, but I was hooked up to CPAP so I'm thinking that controlled a lot of the apnea. Although the tech did make that comment that they couldn't get me titrated with ASV due to a combination of limited time and the fact that as my centrals were handled I went into OSA.
Whatever the case, as a pragmatic approach I haven't slept or napped on my back since. One episode of 21 minutes of apnea in 47 minutes convinced me t0 let that "dream" go. Fortunately recently I have hit upon a good pressure with my alternating pressure mattress that has allowed me to side sleep exclusively without getting excessive pressure point pain. I still get some and I suspect it is causing some arousals but it is manageable.
As for pulmonary edema, my cardiologists have listened to my lungs several times and haven't heard obvious edema. As I understand it there can still be interstitial edema that might be a factor--and it's just currently relatively mild state. As for the rest of me I only have very mild ankle edema. Still something has caused my primarily CSA (as I'm primarily side sleeping) and the OSA when I'm on my back. Your comments here in one of the links was very interesting because of the intermittent aspect that I haven't considered before:"In summary: If left-heart insufficiency causes intermittent pulmonary edema, then intermittent central SDB can occur; if left-heart insufficiency leads to intermittent tissue edema in the upper thoracic/neck area, then obstructive SDB can, at least in theory, be intermittently exacerbated."
I imagine the whole thing about the fluid loading could relate to what I eat or drink, and especially salt which I am very sensitive to. Unfortunately it is too far back for me to remember specifics about how much fluid I might have been retaining. But in the future I'll try to pay more attention
I read a bit on cardiac asthma and it doesn't sound like my symptoms.
The aerophagia hasn't been as bad as on my original trial with only mildly elevated pressure IPAP 5.0. Last night with the EEP at 7.6 I had some, but it was manageable.
Regarding this statement: "I'll also point out is that the Remed Adapt SV requires an extended period of time in which the algorithm adapts to or "reads" the patient before settling into a more comfortable routine." Does "the extended period of time" mean later in the same night or does it refer to a multi-night learning period. If it is multi-night then I've probably not given it enough time. Also when I first got the machine I erased all previous data (except total hours of usage which can't be erased). I am hoping that the Adapt has started fresh with me and is not carrying over some learning from the prior owner. Do you (or anyone who might be reading) know about this?
The great difficulty for me is that I have never had a good night on the Adapt SV and most were I felt quite poor. I have been experimenting with EEP pressure to see if I could find one where I could tolerate it well. I did very poorly in my side-sleeping at EEP 4.0 and back sleeping at 8.0 (which was my titrated CPAP back sleeping pressure). So more recently, thinking that side sleeping would possibly require less pressure I tried 6.8 (not great subjectively but the oximeter averaged 95% for the night) then 7.4 (subjectively better) and recently 7.6. At 7.6 I felt the best for most of the time. But I awoke and found my CMS 50F pulse oximeter reading SpO2 of 74% (whereas always before the Adapt SV has seemingly boosted night average SpO2). At the same time I looked at my onscreen data and saw that my RR was 26. That's more than twice my normal resting rate. And in the morning my EKG seemed to indicate a somewhat elevaton over my norm, And while there has been a progressive improvement,I still experience a overall negative and nowhere near as good as I feel on the S9 (where my recent AHI has been 1.0 with very little evidence of CSR.
My subjective sense as I am going to sleep is that the RR that the Adapt wants to maintain is too fast for me. And I've watched the screen sometimes and it often wants to keep me around RR 18. I've been able a few times to sort of trick the Adapt so that the RR comes down to about 15, which feels better to me. But I have to be looking at the screen to do this.
I am a little suspicious of the CMS 50F for me due to the fact that it can't keep pace of my true pulse rate. Still obviously there was something going on because of the arousal and the decreased O2 reading and the very elevated RR. I have decided to replace the CMS 50F (which I think for most folks is a great bang for the buck oximeter) with the SPO7500 in the hopes that the later will be more sensitive to HR changes and hopefully more sensitive to O2 desaturations as well.
My evaluation period is coming to an end fairly soon with the Adapt SV, so my focus is on figuring out if the Adapt can work for me or not. But maybe I can give the Respironics a try this weekend just to experience the difference.
Best regards.
Re: ASV Titration Help Request
Hello again, ldj325.
It occurs to me that while your thread's purpose is to solicit ASV titration opinions, we have yet to see your ASV charts. Consider posting those as well when you get some time.
It occurs to me that while your thread's purpose is to solicit ASV titration opinions, we have yet to see your ASV charts. Consider posting those as well when you get some time.
Re: ASV Titration Help Request
SWS,-SWS wrote:Hello again, ldj325.
It occurs to me that while your thread's purpose is to solicit ASV titration opinions, we have yet to see your ASV charts. Consider posting those as well when you get some time.
What are the ASV charts?
Re: ASV Titration Help Request
The same kind of graphs that you have posted for the S9. Here's a 2006 example from another Adapt SV user that Muffy posted a while back:ldj325 wrote: What are the ASV charts?
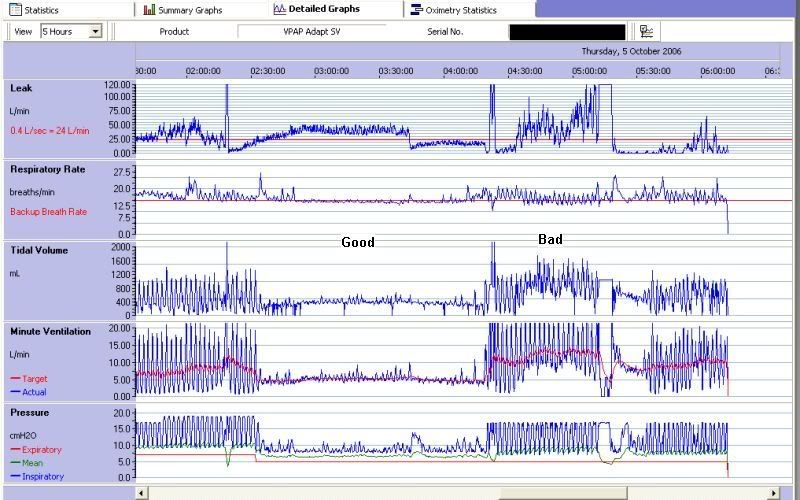
Re: ASV Titration Help Request
In this excerpt. I am assuming that the selections marked "Good" and "Bad" apply to all 5 graphs (vertically). The "volume" or "gain" is radically different between the Good/Bad sections. What is the significance of the extreme left portion of the graphs prior to "Good." The "volume" seems to be more like the "Bad" section--but is it an example of "normal" before the respiratory disturbance of the "Bad" section? Or is it just the tail end of the previous "Bad" section?-SWS wrote:The same kind of graphs that you have posted for the S9. Here's a 2006 example from another Adapt SV user that Muffy posted a while back:ldj325 wrote: What are the ASV charts?
Re: ASV Titration Help Request
-SWS,
Are these graphs from the Adapt SV Original (the one I have) or the Adapt SV Enhanced?
I had a problem with getting my computer to recognize to the Adapt SV via cable download. I was under the impression that the Adapt data had minimal usefulness so I didn't pursue getting the data to download. But I understand some of the usefulness of the data you've posted, especially RR when combined with accurate SpO2 and HR data. I don't know how to interpret the the graphs of minute ventilation or tidal volume, but I can see how they might be useful. Do you know if the Adapt SV reports a Flow graph. I believe I understand those and it seems easy enough to spot apneas by examining them.
Do you have any good tutorial references on how to interpret those MV and TV? I will try to get the Adapt SV downloads but it may take through the weekend.
Next week the SPO7500 should be delivered to me so I hope to add accurate SpO2 and HR. Those 2 in combination with RR of the Adapt seems to me (my guess) where appropriate to indicate a type of arousal event.
Now for some good news. I have had my first night where I have awoken feeling good after a night on the Adapt SV. For the second night in a row I have had the EEP at 7.6. The first night I awoke feeling the best I ever had on the Adapt, but still feeling a bit depleted, "over-breathed" and not nearly as good as the typical night on the S9. Last night I again had the EEP at 7.6 and this time I used the PadaCheek mask liner for the first time. This resulted in a slightly better seal. The leak data for the night was 19L/min (as opposed to approx 26L/min the night before). That leak rate still seems high (I usually have 0.0 leak rate with the S9) but subjectively I was less troubled by the leaks. My onscreen data showed: Avg Pressure 9.2, VT 147-736, MV 4-9, and RR 11-16.
For the first time I did not have that overwhelming sense of being "over-breathed" and my lungs felt good--a bit like the feeling of being in mountain air. I immediately checked my EKG and found it overall trending a bit downward with less variability in rhythm. As I sat a wrote this I did begin to experience a bit of the sense of being "over-breathed." I realized for the first time that there is also a mild sense of heart fatigue like when I over-exercise. But on rechecking the EKG it still showed a relatively low resting HR average (for me) of 85 (vs 110 when things are worst).
Are these graphs from the Adapt SV Original (the one I have) or the Adapt SV Enhanced?
I had a problem with getting my computer to recognize to the Adapt SV via cable download. I was under the impression that the Adapt data had minimal usefulness so I didn't pursue getting the data to download. But I understand some of the usefulness of the data you've posted, especially RR when combined with accurate SpO2 and HR data. I don't know how to interpret the the graphs of minute ventilation or tidal volume, but I can see how they might be useful. Do you know if the Adapt SV reports a Flow graph. I believe I understand those and it seems easy enough to spot apneas by examining them.
Do you have any good tutorial references on how to interpret those MV and TV? I will try to get the Adapt SV downloads but it may take through the weekend.
Next week the SPO7500 should be delivered to me so I hope to add accurate SpO2 and HR. Those 2 in combination with RR of the Adapt seems to me (my guess) where appropriate to indicate a type of arousal event.
Now for some good news. I have had my first night where I have awoken feeling good after a night on the Adapt SV. For the second night in a row I have had the EEP at 7.6. The first night I awoke feeling the best I ever had on the Adapt, but still feeling a bit depleted, "over-breathed" and not nearly as good as the typical night on the S9. Last night I again had the EEP at 7.6 and this time I used the PadaCheek mask liner for the first time. This resulted in a slightly better seal. The leak data for the night was 19L/min (as opposed to approx 26L/min the night before). That leak rate still seems high (I usually have 0.0 leak rate with the S9) but subjectively I was less troubled by the leaks. My onscreen data showed: Avg Pressure 9.2, VT 147-736, MV 4-9, and RR 11-16.
For the first time I did not have that overwhelming sense of being "over-breathed" and my lungs felt good--a bit like the feeling of being in mountain air. I immediately checked my EKG and found it overall trending a bit downward with less variability in rhythm. As I sat a wrote this I did begin to experience a bit of the sense of being "over-breathed." I realized for the first time that there is also a mild sense of heart fatigue like when I over-exercise. But on rechecking the EKG it still showed a relatively low resting HR average (for me) of 85 (vs 110 when things are worst).
Re: ASV Titration Help Request
The annotations aren't mine, ldj325. But I agree that the center portion marked good shows stable respiration from top-to-bottom on those graphs. The far left and far right sections display erratic/unstable patient parameters by the way of RR, tidal volumes, and minute ventilation...ldj325 wrote: In this excerpt. I am assuming that the selections marked "Good" and "Bad" apply to all 5 graphs (vertically). The "volume" or "gain" is radically different between the Good/Bad sections. What is the significance of the extreme left portion of the graphs prior to "Good." The "volume" seems to be more like the "Bad" section--but is it an example of "normal" before the respiratory disturbance of the "Bad" section? Or is it just the tail end of the previous "Bad" section?
Re: ASV Titration Help Request
Since the graphs are dated October 2006, they would be for the original model.ldj325 wrote: Are these graphs from the Adapt SV Original (the one I have) or the Adapt SV Enhanced?
A detailed flow graph is not available for your ASV, ldj325. But you can see how those three patient parameters I mentioned above can be compared against your own more stable baseline to heuristically assess issues like erratic breathing, hypoventilation, hyperventilation, etc.ldj325 wrote:I had a problem with getting my computer to recognize to the Adapt SV via cable download. I was under the impression that the Adapt data had minimal usefulness so I didn't pursue getting the data to download. But I understand some of the usefulness of the data you've posted, especially RR when combined with accurate SpO2 and HR data. I don't know how to interpret the the graphs of minute ventilation or tidal volume, but I can see how they might be useful. Do you know if the Adapt SV reports a Flow graph. I believe I understand those and it seems easy enough to spot apneas by examining them.
Unfortunately I don't have tutorial type references.... But we have had a few Adapt SV discussion threads on this message board that might be worth searching. Again, heuristic data comparison against your own stable baseline would be useful at the VERY least IMHO.Do you have any good tutorial references on how to interpret those MV and TV? I will try to get the Adapt SV downloads but it may take through the weekend.
That's GREAT news!Now for some good news. I have had my first night where I have awoken feeling good after a night on the Adapt SV. For the second night in a row I have had the EEP at 7.6. The first night I awoke feeling the best I ever had on the Adapt, but still feeling a bit depleted, "over-breathed" and not nearly as good as the typical night on the S9. Last night I again had the EEP at 7.6 and this time I used the PadaCheek mask liner for the first time. This resulted in a slightly better seal. The leak data for the night was 19L/min (as opposed to approx 26L/min the night before). That leak rate still seems high (I usually have 0.0 leak rate with the S9) but subjectively I was less troubled by the leaks. My onscreen data showed: Avg Pressure 9.2, VT 147-736, MV 4-9, and RR 11-16.
For the first time I did not have that overwhelming sense of being "over-breathed" and my lungs felt good--a bit like the feeling of being in mountain air. I immediately checked my EKG and found it overall trending a bit downward with less variability in rhythm. As I sat a wrote this I did begin to experience a bit of the sense of being "over-breathed." I realized for the first time that there is also a mild sense of heart fatigue like when I over-exercise. But on rechecking the EKG it still showed a relatively low resting HR average (for me) of 85 (vs 110 when things are worst).
________________________________________________________________________________________________________________________
SUGGESTION: UNLOCK THE RESPIRATORY RATE & VOLUME GRAPHS ON YOUR S9 SO THAT YOU CAN COMPARE THOSE SAME RESPIRATORY PARAMETERS AGAINST YOUR ADAPT SV DATA SET: viewtopic.php?f=1&t=54652&st=0&sk=t&sd= ... me#p510488
You will then be able to compare respiratory-data apples with respiratory-data apples...
P.S. Hats off to gvz for the above simple but GREAT data-display mod!
Re: ASV Titration Help Request
I agree about the great job gvz has done. I've been a beta tester for his program and have been using it for weeks. I've also been looking at oximetery/pulse data from the CMS 50F. I have been comparing the graphs for awhile now on the S9. I have come to term some things as "respiratory events" where there is obviously an increased activation of the respiratory system--which sometimes relates to AHI events and sometimes not. Sometimes the pulse rate correlates with these "events" and again sometimes not. (The questionable accuracy of the CMS 50F tracking of my pulse is a major confounding factor with this.)-SWS wrote: ________________________________________________________________________________________________________________________
SUGGESTION: UNLOCK THE RESPIRATORY RATE & VOLUME GRAPHS ON YOUR S9 SO THAT YOU CAN COMPARE THOSE SAME RESPIRATORY PARAMETERS AGAINST YOUR ADAPT SV DATA SET: viewtopic.php?f=1&t=54652&st=0&sk=t&sd= ... me#p510488
You will then be able to compare respiratory-data apples with respiratory-data apples...
P.S. Hats off to gvz for the above simple but GREAT data-display mod!
Perhaps I need to develop my own personal (heuristic) Respiratory Event Index for the Adapt data and let that be enough, rather than to be concerned with true AHI. If I had this sort of index with the below S9 data, it would be higher that AHI, but still is some sort of measure. So in the examples below there are 6 AHI events (so AHI 1.0) vs what I would term Respiratory Events which are at least 10-13 (for a personal, heuristic "RE index" of 1.5 to 2.0.
I hope to get the Adapt SV data into the computer today--unless I have to rebuild my computer (which is a real task) to get the Adapt recognized.
Re: ASV Titration Help Request
The S9 calculates static pressure with which to "stent" airway obstructions while the Adapt SV calculates dynamic inspiratory Pressure Support with which to "ventilate" centrally-dysregulated breathing. So the obstructive SDB target-pressure calculations performed by the S9 algorithm are entirely irrelevant to the central SDB target-pressure calculations performed by the Adapt SV for the sake of IPAP delivery.ldj325 wrote: I've never received any answer to my early question of the S9 data indicating a median pressure of 5.6, meaning 1/2 the time I'm below that pressure with a lot of time around 4.8--5.2 if the Adapt SV is just too much pressure I suppose leading the pressure induced Centrals.
That means you can't apply S9 obstructive calculations to the ASV's fluctuating IPAP---that latter targeting central undershoot instead of obstructions. IF you knew the S9's calculations were valid and unskewed for your obstructions, then those pressure calculations could be transferred to the ASV's EEP setting/value, which also functions to "stent" your obstructive component. But if S9 were under-delivering pressure for the sake of avoiding exacerbation of S9-detected central apneas, then even those calculations would be suboptimal if not entirely useless.
My understanding is that the above contraindication/concern pertaining to 90% targeting would be ONLY if a patient happened to have a hypoventilatory etiology in the first place. I don't think hypoventilation is linked to your heart issue, whereas periodic breathing most definitely is. That's not to say you can't have a separate and concomitant etiology entailing hypoventilation, of course.ldj325 wrote:Alternatively I've looked at the whole downtrending of 90% of the prior 3 minutes minute ventilation average. Could it be that this drives my CO2 too high and results in the negative symptoms I experience? Does anyone know if this downtrending process continues to occur even in the absence of CSA or CSR. Per my S9 data I'm not having a lot of CSR these days.
Per this reference that I think you or SWS sent me: http://www.sleepcenters.us/adaptive-ser ... hen-brown/ "At its core, the Adapt SV is a highly evolved bilevel device. The IPAP is variable and responds rapidly within 2 or 3 breaths to significant changes in patient tidal volume. When patient tidal volume increases, the device IPAP decreases. When patient tidal volume decreases, the device IPAP increases. Thus the marked fluctuations in patient tidal volume that characterize complex sleep apnea are attenuated and usually the tidal volume is stabilized by the device.
A longer-term correction is effected by the trailing 3-minute memory of minute ventilation and pattern of breathing. After a 3-minute initial collection period, the Adapt SV then sets a minute-ventilation target that is 90% of the previous minute volume. Hence there is a weak downward force on total minute-ventilation that nudges the PCO2 upward 2 or 3 millimeters of mercury, decreasing or eliminating the frequent CO2 dips below the apnea threshold that drives the central events. Because of this 90% target, the manufacturer cautions that the device should not be used in patients who have a condition that might result in hypoventilation."
This post is mainly a bump to find out how that "sweet spot" search is progressing.ldj325 wrote:In the meantime I will keep hunting to see if I can find a "sweet spot" with the Adapt SV.