Why doesn't APAP respond to apneas?
Re: Why doesn't APAP respond to apneas?
Re further testing using my own machine. Last night I uped my epap from 11 to 12 - the machine remained quiet & I am now sure that adjusting my mask has to have been the solution for the long period of high leaks. S0, I am comfortable about changing my settings again.
If there is any benefit to me running my machine same as Bev's (i.e. when comparing the data does it look similar including the Encore pro report that IpapAv is 15). If yes I'll run it that way tonight.
Also, one reason I upped epap is to see what happens to the reported AIs & HIs - result ! - pretty much the same as the night before. Still around 4-5 randomly located AI apnea scores & machine responded with machine triggered breathing and PS boost.
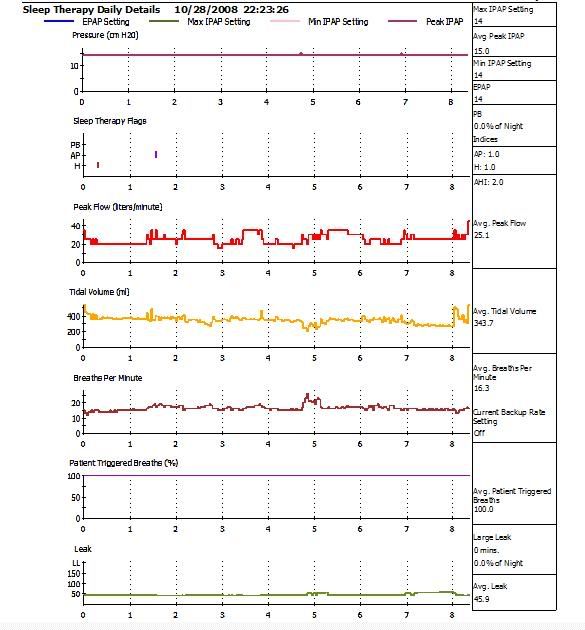
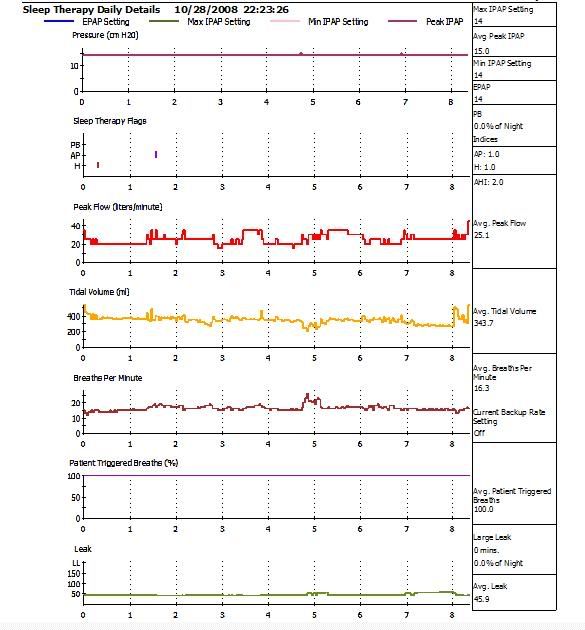
This chart shows night before (haven't yet loaded last nights to the web site).
http://www.internetage.ws/cpapdata/dsm- ... 8oct08.pdf
DSM
If there is any benefit to me running my machine same as Bev's (i.e. when comparing the data does it look similar including the Encore pro report that IpapAv is 15). If yes I'll run it that way tonight.
Also, one reason I upped epap is to see what happens to the reported AIs & HIs - result ! - pretty much the same as the night before. Still around 4-5 randomly located AI apnea scores & machine responded with machine triggered breathing and PS boost.
This chart shows night before (haven't yet loaded last nights to the web site).
http://www.internetage.ws/cpapdata/dsm- ... 8oct08.pdf
DSM
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)
Re: Why doesn't APAP respond to apneas?
If you ask me, that looks a lot better than your other reports I've seen. Zero HI but still a few Apnea Periods. Those AP's are central (based upon the machine cycling to backup mode). BPM is nice and slow, peak and tidal numbers are up there, I'd say you are a deep breather. IF Bev's IPAP working looked like yours I'd be okay with that. You gotta let me do the math on those numbers; BPM=14.2-2=12.2 (60/12.2=4.92/2=2.45) so if you set up a fixed backup mode, it would be BPM=12.2, IT=2.45 and Rise probably high at 5 or 6. But BPM=Auto appears to be handling that nicely.dsm wrote:Re further testing using my own machine. Last night I uped my epap from 11 to 12 - the machine remained quiet & I am now sure that adjusting my mask has to have been the solution for the long period of high leaks. S0, I am comfortable about changing my settings again.
If there is any benefit to me running my machine same as Bev's (i.e. when comparing the data does it look similar including the Encore pro report that IpapAv is 15). If yes I'll run it that way tonight.
Also, one reason I upped epap is to see what happens to the reported AIs & HIs - result ! - pretty much the same as the night before. Still around 4-5 randomly located AI apnea scores & machine responded with machine triggered breathing and PS boost.
This chart shows night before (haven't yet loaded last nights to the web site).
http://www.internetage.ws/cpapdata/dsm- ... 8oct08.pdf
DSM
Doug: Did you notice that report still shows your EPAP=11? Did your upping of EPAP not take?
someday science will catch up to what I'm saying...
Re: Why doesn't APAP respond to apneas?
That chart is from the night before - I still haven't loaded last nights onto the web (can't do so until back home tonight). But I di look at it & it looked very similar in terms of random apnea scores but the tidal volume was a bit lower (which did surprise me).
Those apnea scores are I believe from turning over in the night. I often notice a PS boost after doing so if I happen to be a little more awake than normal.
We are coming into summer & so in recent days have changed bedding from winter to summer & that changeover period always seems to include days of more restless sleep while adjusting.
DSM
Tonight I'll go for 14 CMs epap/ipapMin/IpapMax & leave BPM=auto.
D
Those apnea scores are I believe from turning over in the night. I often notice a PS boost after doing so if I happen to be a little more awake than normal.
We are coming into summer & so in recent days have changed bedding from winter to summer & that changeover period always seems to include days of more restless sleep while adjusting.
DSM
Tonight I'll go for 14 CMs epap/ipapMin/IpapMax & leave BPM=auto.
D
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)
Re: Why doesn't APAP respond to apneas?
Bev: I would erase that SmartCard and run Setup on it next time you get a chance. This machine wasn't brand new was it? Someone could have programmed settings via SmartCard and those would have stuck until you manually changed a parameter via the keys.
Erasing and running Setup on that card would insure there is no carry over from another patient settings (from the SmartCard).
You would get an error if you tried to insert your M series SmartCard in the SV and vice versa, once you erase the card then you can interchange them and use in either machine.
Erasing and running Setup on that card would insure there is no carry over from another patient settings (from the SmartCard).
You would get an error if you tried to insert your M series SmartCard in the SV and vice versa, once you erase the card then you can interchange them and use in either machine.
someday science will catch up to what I'm saying...
Re: Why doesn't APAP respond to apneas?
This was a brand new machine when I got it. Original, sealed Respironics box. The card was new.
Bev
Y'all stop talking about my small lungs. There is a reason they used to call me Olive Oyle.
Bev
Y'all stop talking about my small lungs. There is a reason they used to call me Olive Oyle.
Diagnosed 9/4/07
Sleep Study Titrated to 19 cm H2O
Rotating between Activa and Softgel
11/2/07 RemStar M Series Auto with AFlex 14-17
10/17/08 BiPAP Auto SV 13/13-23, BPM Auto, AHI avg <1
Sleep Study Titrated to 19 cm H2O
Rotating between Activa and Softgel
11/2/07 RemStar M Series Auto with AFlex 14-17
10/17/08 BiPAP Auto SV 13/13-23, BPM Auto, AHI avg <1
Re: Why doesn't APAP respond to apneas?
Cute n slender is the descriptionOutaSync wrote:This was a brand new machine when I got it. Original, sealed Respironics box. The card was new.
Bev
Y'all stop talking about my small lungs. There is a reason they used to call me Olive Oyle.
DSM
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
On Hazards Of Dial-Wingin'
This thread now looks like something that Nostradamus would write. If you predict everything, then you're going to be right at least some of the time. Let's go back and try to answer some of the questions.
Zolpidem (Ambien) may be very helpful in some cases of SDB by promoting stable sleep, which in turn promotes stable airway.
Recently, it has been suggested that zolpidem may also have a direct effect on increasing genioglossus activity:
Systemic vs. Central Administration of Common Hypnotics Reveals Opposing Effects on Genioglossus Muscle Activity in Rats Volume: 31 (3) p. 355-365; Eileen Park, MSc; Magdy Younes, MD; Hattie Liu, MSc; Xia Liu, PhD; Richard L Horner, PhD
Wontcha just love it when portable monitoring replaces NPSG?
Anyway, I'd really like to see a drug-free NPSG and MSLT one of these days.
BTW, there dial-wingers, there was desaturation to 73.00% on BiPAP 14/10, so I sure hope you guess right.
SAG
That area is clearly SWS, and has extremely long obstructive events in the diagnostic portion of the split and central events in the BiPAP titration, with both cases resulting in dangerously low levels of oxygen desaturation. In some of the events, Bev sleeps right through them, they are not terminated by arousal. This is highly unusual because (1)SWS should promote airway stability (and prevent obstructive events) and (2)the mechanism of event termination in adults is usually arousal (although again, M. Younes would probably debate this any day of the week).StillAnotherGuest wrote:Not necessarily. It can also mean stabilized sleep. For instance, SWS (the sleep kind, not the not the palabrating kind) is very airway-stabilizing.Snoredog wrote:the absence of events means stabilized breathing.
Which makes me wonder about that hypnogram (there was a hypnogram, wasn't there? Or is that the 'shrooms again?) where that initial block of SWS has horrific desats. That area really needs to be dissected.
Zolpidem (Ambien) may be very helpful in some cases of SDB by promoting stable sleep, which in turn promotes stable airway.
Recently, it has been suggested that zolpidem may also have a direct effect on increasing genioglossus activity:
Systemic vs. Central Administration of Common Hypnotics Reveals Opposing Effects on Genioglossus Muscle Activity in Rats Volume: 31 (3) p. 355-365; Eileen Park, MSc; Magdy Younes, MD; Hattie Liu, MSc; Xia Liu, PhD; Richard L Horner, PhD
In Bev's case, however, I believe that while arousal threshold is greatly increased, the other phenomena can not occur quickly enough to keep her out of significant trouble when under the influence of zolpidem. Without PAP support, CO2 doesn't increase fast enough to generate arousal before the O2 becomes dangerously low when obstructive apnea occurs. And with BiPAP support, the same thing occurs, but now the culprit is central apnea (BTW, based on where the oximetry probe was located, I don't believe there is any circulatory delay). In both cases, O2 saturation drops far more rapidly that CO2 increases.Lorazepam and zolpidem have an inhibitory effect on GG activity via local effects at the HMN (hypoglossal motor nucleus). Following systemic administration, however, this inhibitory effect can be outweighed both by a delay in arousal (allowing greater CO2-mediated respiratory stimulation in sleep) and excitatory influences on baseline GG activity via mechanisms operating outside the HMN.
Wontcha just love it when portable monitoring replaces NPSG?
Anyway, I'd really like to see a drug-free NPSG and MSLT one of these days.
BTW, there dial-wingers, there was desaturation to 73.00% on BiPAP 14/10, so I sure hope you guess right.
SAG

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
Re: Why doesn't APAP respond to apneas?
SAG, what would you do if you were me? So I can qualify and until I can get a new study? What kind of reports should I be running to take to the Dr.?
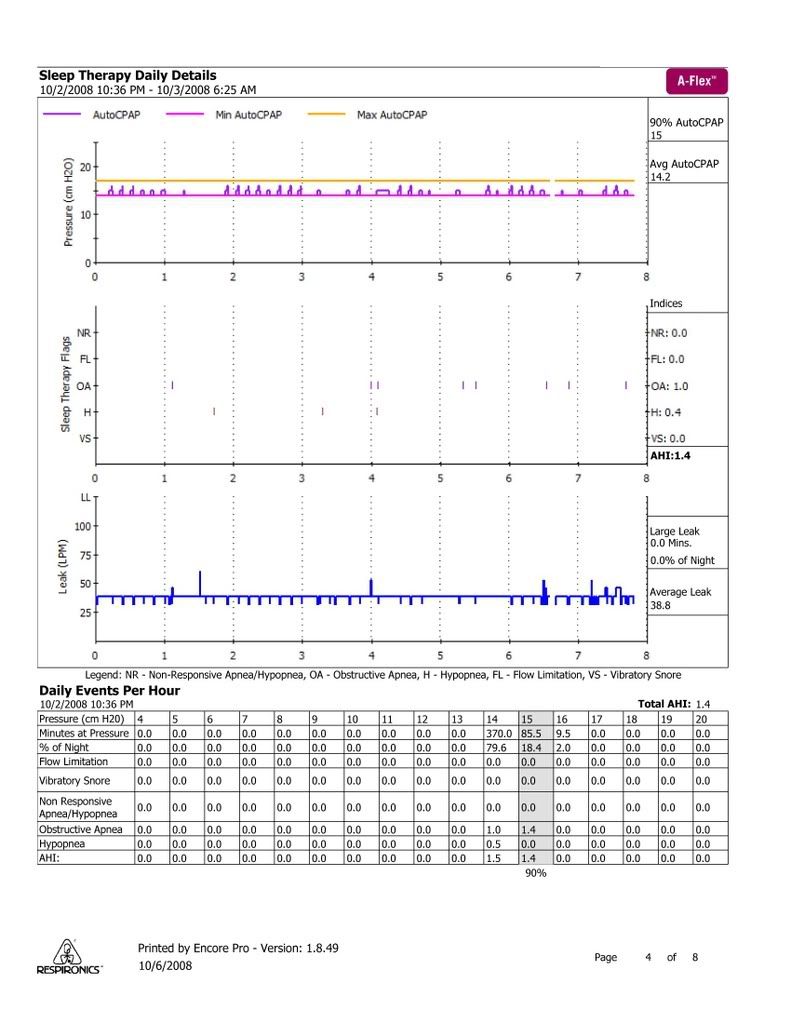
Last night's data:
Bev
Last night's data:
Bev
Diagnosed 9/4/07
Sleep Study Titrated to 19 cm H2O
Rotating between Activa and Softgel
11/2/07 RemStar M Series Auto with AFlex 14-17
10/17/08 BiPAP Auto SV 13/13-23, BPM Auto, AHI avg <1
Sleep Study Titrated to 19 cm H2O
Rotating between Activa and Softgel
11/2/07 RemStar M Series Auto with AFlex 14-17
10/17/08 BiPAP Auto SV 13/13-23, BPM Auto, AHI avg <1
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
Re: Why doesn't APAP respond to apneas?
Bring all the Encore Reports, which clearly show virtually complete control of SBD. The complaint is exactly as you describe, Persistent Excessive Daytime Sleepiness, R/O (at least) narcolepsy, idiopathic hypersomnolece and complex sleep apnea.
The AASM Standards For Practice is quite clear on the Indications For Polysomnography in this case:
PS - Add in the part where you think that the results were contaminated by the Lexapro and Ambien. Absolutely that there was no REM to analyze.
The AASM Standards For Practice is quite clear on the Indications For Polysomnography in this case:
SAGAASM Standards For Practice wrote:When clinical response is insufficient or when symptoms return despite a good initial response to treatment with CPAP. In these circumstances, testing should be devised with consideration that a concurrent sleep disorder may be present (e.g., OSA and narcolepsy)
PS - Add in the part where you think that the results were contaminated by the Lexapro and Ambien. Absolutely that there was no REM to analyze.

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
Re: Why doesn't APAP respond to apneas?
SAG, thanks for the preliminary analysis. Looking at the 14 cm CPAP results, I personally don't think rushing back to Bev's home-determined APAP 14 -17 setting lends any less risk of desaturation.
But I personally wouldn't go back to that same lab. Rather I'd select an institution that recognizes and properly manages complex sleep disordered breathing problems. They can properly rule that phenotype in or out. I don't think your current sleep doctor is in tune with what's really happening with your sleep physiology.
More later...
Bev, I personally think your best case for another sleep study might be garnered by also collecting data using a recording pulse oximeter--- to go along with your Encore charts. If your SpO2 readings are unacceptably low while AHI is acceptable (as some of us probably suspect) then you will have ample evidence for another sleep study.OutaSync wrote:SAG, what would you do if you were me? So I can qualify and until I can get a new study? What kind of reports should I be running to take to the Dr.?
But I personally wouldn't go back to that same lab. Rather I'd select an institution that recognizes and properly manages complex sleep disordered breathing problems. They can properly rule that phenotype in or out. I don't think your current sleep doctor is in tune with what's really happening with your sleep physiology.
More later...
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
Maybe So, Maybe Not...
Probably not, but it won't hurt, and might help. She never really used 17 cmH2O so it's somewhat academic, there seems to be occassional breakthroughs that might be the REM-related OSA, there's the positional thing, and once you take all the "bidets" off the graph, whenever you are left with a "table" (I guess if it would make more sense to have a constant "furniture" theme and call them "chairs", but who can't but smile when they think of "bidet". Just don't sit on the bidet and then sit on the table. Or now that I think of it, if you're going to sit on the table, perhaps one should use the bidet first) those are the areas where beneficial activity may be taking place.-SWS wrote:I personally don't think rushing back to Bev's home-determined APAP 14 -17 setting lends any less risk of desaturation
SAG

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
Re: Why doesn't APAP respond to apneas?
So we have another example of bad Encore Pro reporting math. Again, we have EPAP, IPAPmin, and IPAPmax all set at 14 cmH2O (straight CPAP). And yet Encore Pro reports an average IPAPpeak of 15 cmH2O. Then we have exactly two scored events by the way of tick marks. For more than 8 hours of sleep we see one scored Apnea, one scored Hypopnea, and Enore Pro's magic math arrives at an AHI of 2.0. One of those two reporting areas is clearly wrong. Is it any wonder that medical professionals think home monitoring has some serious problems?
And this machine is the model that's targeted for very serious cases of chronic heart failure (CHF/CSR). Does anyone find this crappy clinician software as highly annoying as I do?
---------------------------------------------------------------------------------------------------
SAG, you speculated about latent or non-existent arousals in response to OA or CA. I personally suspect that part of the theoretical analysis might very well be correct. Let's assume that it's correct for this particular line of inquiry: At this point of our theoretical analysis we have choreographed: 1) an apnea with 2) a latent or remiss arousal/awakening mechanism, and 3) consequential desaturation.
We still have a couple paradoxes on our hands, though:
1) Excessive RDI- If arousals are not occurring as a timely response to help mitigate apneic desaturations, then why might they be occurring in such large numbers for complex SDB patients? What might the stimuli-related mechanism be in complex SDB pathophysiology to cause an excessive RDI that seems to not resolve A or H---and at the same time will not be satisfactorily mitigated with PAP?
2) Minimal AHI in cases of slight CompSA/CSDB- Is this actually a paradox regarding complex SDB? Or is AHI scoring simply too time-permissive or coarse regarding perhaps extremely short, sudden disruptions to both eupneic breathing and sleep drive?
Again, I believe minimal compSA/CSDB AHI can sometimes be attributed to a non-linear pressure relationship regarding nothing more than minimization of the frank A and H part of CompSA/CSDB pathophysiology---with that pressure-related "saddle-point" not necessarily having successfully mitigated the excessive RDI/RERA component of compSA/CSDB.
I think that may be what's happening in Bev's case as she sits around 14 cmH2O with a great AHI and yet highly deteriorated overall sleep---deteriorated presumably because of an unresolved RDI/RERA component that is both excessive and typical of CompSA/CSDB.
And this machine is the model that's targeted for very serious cases of chronic heart failure (CHF/CSR). Does anyone find this crappy clinician software as highly annoying as I do?
---------------------------------------------------------------------------------------------------
SAG, you speculated about latent or non-existent arousals in response to OA or CA. I personally suspect that part of the theoretical analysis might very well be correct. Let's assume that it's correct for this particular line of inquiry: At this point of our theoretical analysis we have choreographed: 1) an apnea with 2) a latent or remiss arousal/awakening mechanism, and 3) consequential desaturation.
We still have a couple paradoxes on our hands, though:
1) Excessive RDI- If arousals are not occurring as a timely response to help mitigate apneic desaturations, then why might they be occurring in such large numbers for complex SDB patients? What might the stimuli-related mechanism be in complex SDB pathophysiology to cause an excessive RDI that seems to not resolve A or H---and at the same time will not be satisfactorily mitigated with PAP?
2) Minimal AHI in cases of slight CompSA/CSDB- Is this actually a paradox regarding complex SDB? Or is AHI scoring simply too time-permissive or coarse regarding perhaps extremely short, sudden disruptions to both eupneic breathing and sleep drive?
Again, I believe minimal compSA/CSDB AHI can sometimes be attributed to a non-linear pressure relationship regarding nothing more than minimization of the frank A and H part of CompSA/CSDB pathophysiology---with that pressure-related "saddle-point" not necessarily having successfully mitigated the excessive RDI/RERA component of compSA/CSDB.
I think that may be what's happening in Bev's case as she sits around 14 cmH2O with a great AHI and yet highly deteriorated overall sleep---deteriorated presumably because of an unresolved RDI/RERA component that is both excessive and typical of CompSA/CSDB.
Re: Maybe So, Maybe Not...
Bev, SAG's wondering above if slightly higher CPAP pressure than 14 cm just might be of benefit as you wait for your next PSG. I had wondered the same a few pages back, as did Snoredog, and MUCH earlier in the thread ozij (she talked about raising that bottom APAP pressure). So the line of conjecture is whether you might gain benefit by adjusting your pressure to not the highest peaks (where the algorithm lowered its pressure based on no measured gains)---but rather at those slightly lower "chair seats". Looks to be about 15 cmH2O CPAP.StillAnotherGuest wrote:...there seems to be occassional breakthroughs that might be the REM-related OSA, there's the positional thing, and once you take all the "bidets" off the graph, whenever you are left with a "table" (I guess if it would make more sense to have a constant "furniture" theme and call them "chairs", but who can't but smile when they think of "bidet". Just don't sit on the bidet and then sit on the table. Or now that I think of it, if you're going to sit on the table, perhaps one should use the bidet first) those are the areas where beneficial activity may be taking place.
Also, here's the place I would consider arranging a sleep study if I were in this particular situation of apparently suffering deteriorated sleep with excessive unresolved RDI (and having shown central emergence on my BiLevel titration):
http://www.bidmc.org/CentersandDepartme ... Staff.aspx
That's Harvard medical school's teaching hospital. And the team members above that I might try to arrange my sleep study with would be any of these authors:
http://www.ncbi.nlm.nih.gov/pubmed/16217173
I'd take a night and day for the initial PSG/MSLT sleep study, and then enjoy the other days and nights as a nice out-of-town vacation experience. There's plenty to do in that area as a tourist! Bring your autoSV should they want to titrate either BiLevel S/T or SV modality during a split-night study. Just a suggestion.
Also, Bev, give yourself time to see whether Lyrica does anything for you as you baseline. If you decide to baseline BiLevel or retest SV pending baselined results, I think you would be wise to record SpO2 as well.
Re: Why doesn't APAP respond to apneas?
Those are some great links with a lot of information. I'll have to delve in when I get home.
I'll run on up to that Harvard center as soon as I win the lottery. Right now, I have to get enough information together to convince my insurance company that I need to have another sleep test. I would have to have a referral, and since my current sleep doctor thinks I'm "fine" and "doing well", I doubt I'll get one from him. But he has partners, who are more experienced, so if I could make my case, with facts and figures from the same sleep studies that the doctor reviewed, maybe I could get somewhere.
So, do you think I should continue the week with CPAP 14, or do some changing now?
Bev
I'll run on up to that Harvard center as soon as I win the lottery. Right now, I have to get enough information together to convince my insurance company that I need to have another sleep test. I would have to have a referral, and since my current sleep doctor thinks I'm "fine" and "doing well", I doubt I'll get one from him. But he has partners, who are more experienced, so if I could make my case, with facts and figures from the same sleep studies that the doctor reviewed, maybe I could get somewhere.
So, do you think I should continue the week with CPAP 14, or do some changing now?
Bev
Diagnosed 9/4/07
Sleep Study Titrated to 19 cm H2O
Rotating between Activa and Softgel
11/2/07 RemStar M Series Auto with AFlex 14-17
10/17/08 BiPAP Auto SV 13/13-23, BPM Auto, AHI avg <1
Sleep Study Titrated to 19 cm H2O
Rotating between Activa and Softgel
11/2/07 RemStar M Series Auto with AFlex 14-17
10/17/08 BiPAP Auto SV 13/13-23, BPM Auto, AHI avg <1
Re: Why doesn't APAP respond to apneas?
If it were me I'd run another night at 14 cm. Then I'd switch to 15 cm for a while and see if symptoms improve.
If moving on to baselining with BiLevel I'd try to get my hands on an overnight recording pulse oximeter somehow. Buy, borrow, or even get it R/X'ed by any doc, including your general practitioner.
If moving on to baselining with BiLevel I'd try to get my hands on an overnight recording pulse oximeter somehow. Buy, borrow, or even get it R/X'ed by any doc, including your general practitioner.











