BILEVEL PAP Therapy Pearls: Clearing the First Hurdle
-
BarryKrakowMD
- Posts: 65
- Joined: Wed Dec 05, 2007 12:48 am
- Contact:
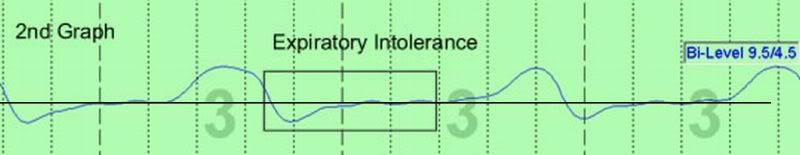
Expiratory Airflow Curves
As promised some weeks back, I've posted a comparison of two expiratory flow curves, one normal, smooth and rounded (1st Graph) and the other abnormal, choppy, and irregular (2nd Graph).
These sleep epochs are taken from the same patient who is in stage 2 NREM sleep in the 1st graph and stage 3 NREM sleep in the 2nd graph. These are real sleep epochs taken from a 30-second period from the polysomnogram.
I've just posted the epochs and some additional comments on my blog at http://www.sleepdynamictherapy.com, but if someone prefers to copy the graphs into this thread, feel free to do so.
The graphs will show you close-up one of the primary influences that spurred us to switch most of our SDB patients from CPAP to bilevel. I'm not expecting this to "settle" the bilevel debate. But, I hope it provides a specific insight about our thinking and clinical experience.
In particular, the presence of expiratory intolerance as seen in the lab on the night of titration correlated well with a patient's complaint of discomfort on expiration with CPAP. And, the cessation of this discomfort correlated well with the removal of expiratory intolerance with the use of bilevel.
These sleep epochs are taken from the same patient who is in stage 2 NREM sleep in the 1st graph and stage 3 NREM sleep in the 2nd graph. These are real sleep epochs taken from a 30-second period from the polysomnogram.
I've just posted the epochs and some additional comments on my blog at http://www.sleepdynamictherapy.com, but if someone prefers to copy the graphs into this thread, feel free to do so.
The graphs will show you close-up one of the primary influences that spurred us to switch most of our SDB patients from CPAP to bilevel. I'm not expecting this to "settle" the bilevel debate. But, I hope it provides a specific insight about our thinking and clinical experience.
In particular, the presence of expiratory intolerance as seen in the lab on the night of titration correlated well with a patient's complaint of discomfort on expiration with CPAP. And, the cessation of this discomfort correlated well with the removal of expiratory intolerance with the use of bilevel.
_________________
| Humidifier: HC150 Heated Humidifier With Hose, 2 Chambers and Stand |
| Additional Comments: Puritan Bennett Breeze Nasal Pillows; ResMed Mirage Quattro FFM; Respironics Premium Chinstrap; Breath Right Nasal Strips |
Barry Krakow, MD
Blogging at Fast Asleep (Sign up: https://fastasleep.substack.com/embed
Books & Videos at http://www.barrykrakowmd.com
Practice at http://www.barrykrakowmd.com
Blogging at Fast Asleep (Sign up: https://fastasleep.substack.com/embed
Books & Videos at http://www.barrykrakowmd.com
Practice at http://www.barrykrakowmd.com
-
Guest
Dr.Krakow,
Sad to know that up to date the manufacturers of cpap/apap/bipap still does not make the firmware algorithm dynamic enought for software upgrading from one algorithm function to another for better and correct treatment of SDB suffers. Is profits or opprotunity motives these manufactures to move forward for the benefits of SBD sufferes? A dynamic upgrdeable algoritms for the cpap is much needed so as much as expert systems in assistng the SDB sufferes for better predictable patency. Please comment.
Mckooi
Sad to know that up to date the manufacturers of cpap/apap/bipap still does not make the firmware algorithm dynamic enought for software upgrading from one algorithm function to another for better and correct treatment of SDB suffers. Is profits or opprotunity motives these manufactures to move forward for the benefits of SBD sufferes? A dynamic upgrdeable algoritms for the cpap is much needed so as much as expert systems in assistng the SDB sufferes for better predictable patency. Please comment.
Mckooi
-
BarryKrakowMD
- Posts: 65
- Joined: Wed Dec 05, 2007 12:48 am
- Contact:
Respiratory Physiology
If I'm understanding the question posed, the most important thing I can tell you is that were you to ask any medical student which basic science module was the most difficult to understand, the majority would answer, "Pulmonary Medicine." I still have vivid memories of going nuts in 1981 trying to understand what amounts to the physics and physiology of breathing.
Through the years, it has also been apparent to me at least, that pulmonologist are easily some of or perhaps the highest IQ docs in medicine today. My hats off to them, because it's a very difficult area of study. (Note:we have an IQ discussion going on in the Dr. Krakow's book topic, and I'll be clarifying some points about IQ, insomnia patients and doctors' bedside manners this weekend or next week in a new post there.)
Thus, my conclusion, conspiracy theories aside, is that it is just too difficult to produce the algorithm we need to auto-titrate patients, be it with CPAP or bilevel, although the new ASV devices suggest improvements continue to be made.
So, I do not think it's a "business thing," although it does take time for industry to improve technology and receive approval to sell it. As such, they have a vested interest in trying to improve things but not waiting until they have perfected the technology before they sell to the public.
My hunch and that of my colleagues is as above; it's just too difficult to figure out this algorithm at this point in time. Are we a year away or decade away? I don't know, but you better believe the sleep industry is working diligently on the R & D because the payoff will be huge if they can really figure out a great auto-titrating algorithm that's as good or better than a great sleep tech.
Through the years, it has also been apparent to me at least, that pulmonologist are easily some of or perhaps the highest IQ docs in medicine today. My hats off to them, because it's a very difficult area of study. (Note:we have an IQ discussion going on in the Dr. Krakow's book topic, and I'll be clarifying some points about IQ, insomnia patients and doctors' bedside manners this weekend or next week in a new post there.)
Thus, my conclusion, conspiracy theories aside, is that it is just too difficult to produce the algorithm we need to auto-titrate patients, be it with CPAP or bilevel, although the new ASV devices suggest improvements continue to be made.
So, I do not think it's a "business thing," although it does take time for industry to improve technology and receive approval to sell it. As such, they have a vested interest in trying to improve things but not waiting until they have perfected the technology before they sell to the public.
My hunch and that of my colleagues is as above; it's just too difficult to figure out this algorithm at this point in time. Are we a year away or decade away? I don't know, but you better believe the sleep industry is working diligently on the R & D because the payoff will be huge if they can really figure out a great auto-titrating algorithm that's as good or better than a great sleep tech.
_________________
| Humidifier: HC150 Heated Humidifier With Hose, 2 Chambers and Stand |
| Additional Comments: Puritan Bennett Breeze Nasal Pillows; ResMed Mirage Quattro FFM; Respironics Premium Chinstrap; Breath Right Nasal Strips |
Barry Krakow, MD
Blogging at Fast Asleep (Sign up: https://fastasleep.substack.com/embed
Books & Videos at http://www.barrykrakowmd.com
Practice at http://www.barrykrakowmd.com
Blogging at Fast Asleep (Sign up: https://fastasleep.substack.com/embed
Books & Videos at http://www.barrykrakowmd.com
Practice at http://www.barrykrakowmd.com
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
But In Proper Context...
Well those graphs certainly look interesting. But it is unclear to me as to where active expiration actually ends. Is this it?
(my guess at where threshold = 0 is. If that ain't it, then I need to go in a different direction.)
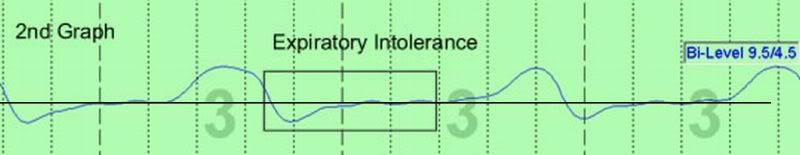
Right, looking at a single channel of anything rarely gives the whole picture of what's really happening. Can you print up the whole montage of that expiratory instability so we can see what everything else is doing?
Also, what BiLevel is that, the 425?
Thank you for your time and expertise.
SAG
(my guess at where threshold = 0 is. If that ain't it, then I need to go in a different direction.)
Right, looking at a single channel of anything rarely gives the whole picture of what's really happening. Can you print up the whole montage of that expiratory instability so we can see what everything else is doing?
Also, what BiLevel is that, the 425?
Thank you for your time and expertise.
SAG

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
-
Guest
Re: Expiratory Airflow Curves
Dr, I wanted to ask if there's a real-world application to this look at two entirely different EPAP/IPAP ranges, at different sleep stages -- in the lab you had him/her at 5/3 while he was in Stage 2 sleep, and ended up with a normal airflow curve.BarryKrakowMD wrote:As promised some weeks back, I've posted a comparison of two expiratory flow curves, one normal, smooth and rounded (1st Graph) and the other abnormal, choppy, and irregular (2nd Graph).
These sleep epochs are taken from the same patient who is in stage 2 NREM sleep in the 1st graph and stage 3 NREM sleep in the 2nd graph.
When he was in Stage 3 though, you changed him to 9.5/4.5 and saw a jagged airflow curve, so we know that's not a good setting for him.
Is it possible that his breathing pattern/needs could change depending on the Stage of sleep he's in at that moment? So when he goes home and doesn't have a team of people watching him sleep and tinkering with his pressures in response to his then-current breathing, mightn't the 5/3 pressure setting that resulted in a nice smooth airflow curve in the lab during Stage 2 sleep not provide that same smooth result when he's in Stage 1, or 3, or REM, or if he rolls onto his back, or has had a cocktail before bed, etc?
I guess I'm trying to find the link between a nice normal airflow under specific situations in the lab, and the single set of pressure settings (ignoring Auto-BiPAP) that he'd use once he goes home. Would he go home with a 5/3 pressure setting, and would that be likely to provide a smooth airflow throughout most of his night's sleep stages?
I find your posts very interesting, and I do appreciate all your insights... Thanks for taking the time to participate here!
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
On Bumps &c
Although y'know, if the activity is of the low frequency type, the next thing to look for would be the effect of cardiac pulsation on the waveform. This may be more apparent as the patient approaches end-exhalation.BarryKrakowMD wrote:we can all probably imagine a number of possible explanations for these changes, such as general airflow turbulence or some subtle form of leak, but in our clinical experience the pattern in the 2nd Graph is what we term “Expiratory Intolerance” or “Expiratory Instability.” We believe this description is accurate, because this pattern often emerges during a time when the patient may go on to develop a full-blown iatrogenic central apnea, that is, in response to EPAP, the patient cannot tolerate pressurized airflow coming in as they attempt to breathe out. When this “tension” reaches a tipping point, the patient simply stops breathing.
But another important variable is the activity of the machine itself. As noted, there are going to be variations in pressure as it responds to changes in the system. With the "bumps" that are shown above being quite low frequency (~1 Hz), that would be the first thing I would look for.
Admittedly, I haven't seen too many PB machines in action, but the one I did see in head to head competition seemed to exhibit an interesting behavior. It also had "bumps" in the waveform (~1 Hz) in distinct contrast to the same test conditions in a competitor machine. While some of these anomalies could be attributed to cardiac pulsations, it is clear that not all of them were, as they did not quite match up with QRS:
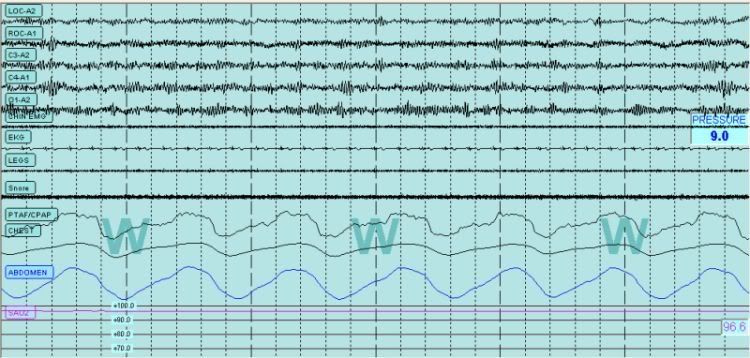
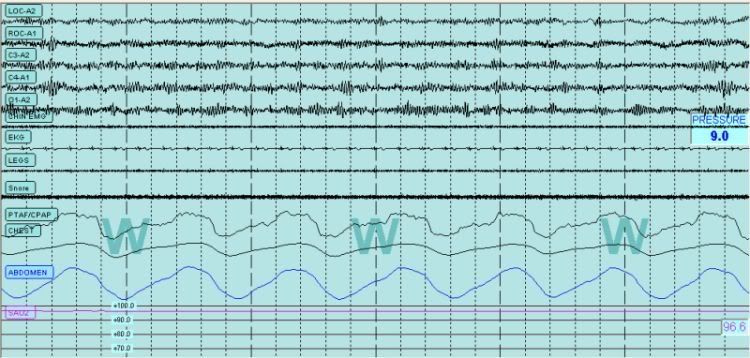
Respironics Synchrony

PB420E

Distinct PB420E Cardiac Pulsation Discord
(Cardiac Pulsations Are Affirmed in the Addominal Channel)
So, is this phenomenon a question of PB42x flow response vs expiratory instability (I would doubt "intolerance" per se, since the patient was sleeping)(and at this point, had logged in about 1000 nights of therapy)(on the PB420E, so any intolerance would have thought to be on the Synchrony).
Oh yeah, central apneas. Post for tomorrow.
SAG

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
Does EFL Really Matter?
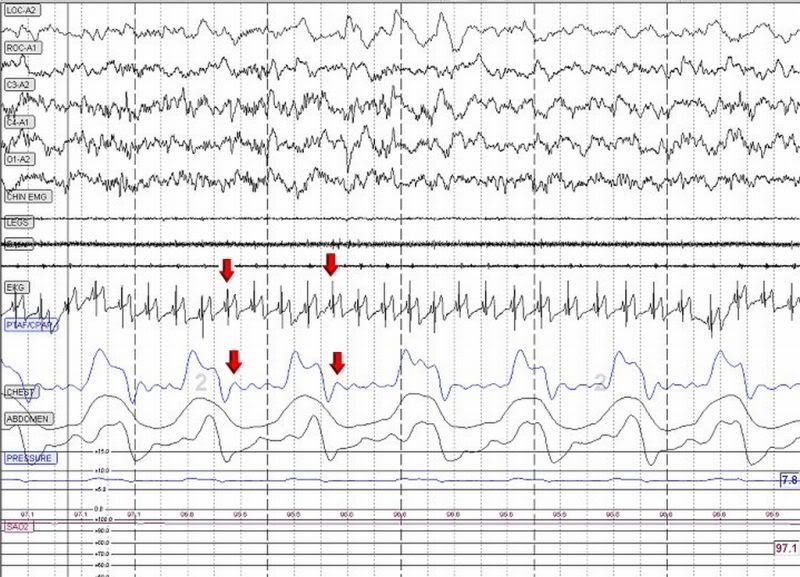
However, being that I have the attention span of Oh, hey! Look at this! In going back over this person's diagnostic NPSG (no pressure therapy) looking for expiratory phenomena (maybe not "expiratory intolerance" per se, but perhaps instability, flow limitation, artifact or whatever)(BTW, this person is a world renown mouth breather, and in the endless list of things I'm not, one is an ENT surgeon, but I've gotten the impression there there may be some nasal narrowing. While a tiny nose looks good, it tends to lack functionality):

And then mouth breathing lends to some pretty gnarly-looking pressure waveforms.
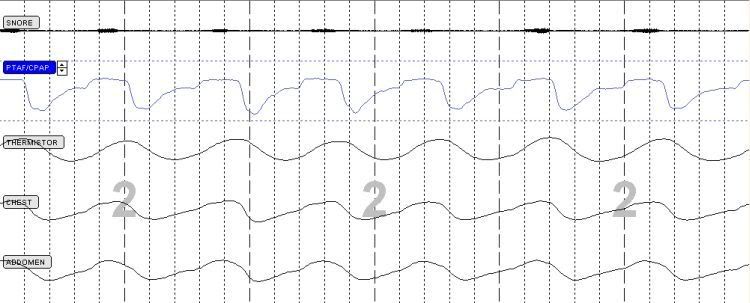
So anyway, here's a good shot of relatively normal breathing (PTAF waveform) as it moves rapidly from rounded to flattened (flow limitation) and on to hypopnea):

And an extended run of flow limitation (flattened PTAF tops with some concommitant snoring on inspiration above). See how the Thermistor does not accurately represent this:
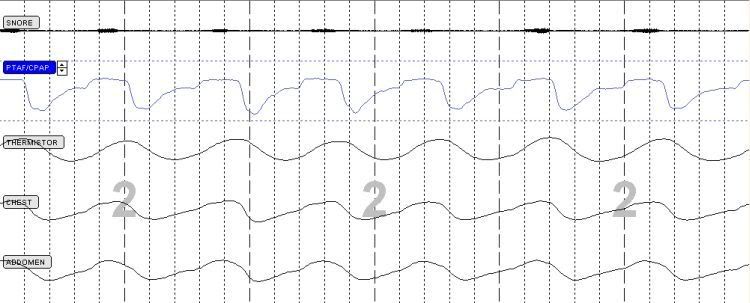
While the first question one must always ask is "What is it you're trying to fix?", close behind comes "Is what you're trying to fix really need fixing?" and "Can what you're trying to fix really be fixed?" If you've got severe nasal narrowing and use a nasal mask, chances are you're never going to correct flow limitations.
SAG

And then mouth breathing lends to some pretty gnarly-looking pressure waveforms.
So anyway, here's a good shot of relatively normal breathing (PTAF waveform) as it moves rapidly from rounded to flattened (flow limitation) and on to hypopnea):

And an extended run of flow limitation (flattened PTAF tops with some concommitant snoring on inspiration above). See how the Thermistor does not accurately represent this:
While the first question one must always ask is "What is it you're trying to fix?", close behind comes "Is what you're trying to fix really need fixing?" and "Can what you're trying to fix really be fixed?" If you've got severe nasal narrowing and use a nasal mask, chances are you're never going to correct flow limitations.
SAG

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
- rested gal
- Posts: 12880
- Joined: Thu Sep 09, 2004 10:14 pm
- Location: Tennessee
Re: Does EFL Really Matter?
My concern would also be, "Can what you're trying to fix even be fixed short of using a pressure of IPAP 25 / EPAP whatever?"StillAnotherGuest wrote:"Can what you're trying to fix really be fixed?"
If things are going reasonably well at reasonable pressures, and the person feels well rested every morning, why pursue rounding out every single last flow limitation, if to do that means increasing pressure to the point of mask seal difficulties, increased vent noise, aerophagia..... ?
ResMed S9 VPAP Auto (ASV)
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
A Single Page Does Not Define A Book...
Right. What we must ask is:
1. Are expiratory flow limitations (EFL) really present in any given patient? If so, are they effectively treated during CPAP titration with conventional criteria, rendering them academic?
2. Who is at risk for EFL? Generally, we've been tending to look at obese to morbidly obese (like split-city's study group)(Oh no, not the Mega Pes again!)
3. How can EFL be measured? I would submit that the highly filtered channel out of a CPAP machine would not be the way to go. Nor, I suppose, would a split_city montage on a routine basis, maybe something in between.
4. Can EFL emerge with the application of an expiratory adjunct (CFlex, AFlex, EPR or bilevel)?
5. Are they treatable (pressure responsive)? I think you better figure out what the cause of the "EFL" is. Machine artifact, obstructive airways disease or cardiac failure are examples of non-UA "EFL".
6. Are they clinically significant? If the EFLs are present and are not addressed by attacking events traditionally associated with inspiration (apneas, hypopneas and flow limitations), one must then ask if the EFLs are, in fact, causing a problem, such as desaturation, arousal, or change in intrathoracic pressure (and that change, if present, would be an increase in pressure).
If none of those entities exist, then this just amounts to "treating the waveform."
And all this relates to sleep. If this is a comfort issue that relates to Wake, or Wake/1 transition, one still treats the the patient's subjective assessment, not the waveform.
Speaking of which
What are you trying to fix?
And GFL when Level IV 2 channel "PSG" comes along.
SAG
1. Are expiratory flow limitations (EFL) really present in any given patient? If so, are they effectively treated during CPAP titration with conventional criteria, rendering them academic?
2. Who is at risk for EFL? Generally, we've been tending to look at obese to morbidly obese (like split-city's study group)(Oh no, not the Mega Pes again!)
3. How can EFL be measured? I would submit that the highly filtered channel out of a CPAP machine would not be the way to go. Nor, I suppose, would a split_city montage on a routine basis, maybe something in between.
4. Can EFL emerge with the application of an expiratory adjunct (CFlex, AFlex, EPR or bilevel)?
5. Are they treatable (pressure responsive)? I think you better figure out what the cause of the "EFL" is. Machine artifact, obstructive airways disease or cardiac failure are examples of non-UA "EFL".
6. Are they clinically significant? If the EFLs are present and are not addressed by attacking events traditionally associated with inspiration (apneas, hypopneas and flow limitations), one must then ask if the EFLs are, in fact, causing a problem, such as desaturation, arousal, or change in intrathoracic pressure (and that change, if present, would be an increase in pressure).
If none of those entities exist, then this just amounts to "treating the waveform."
And all this relates to sleep. If this is a comfort issue that relates to Wake, or Wake/1 transition, one still treats the the patient's subjective assessment, not the waveform.
Speaking of which
Here's an Epoch of Li'l PerkyNose during Wake (defined by all the alpha) with theoretically normal UA tone and on 9 cmH2O CPAP, clearly showing a pattern of flow limitation:rested gal wrote:My concern would also be, "Can what you're trying to fix even be fixed short of using a pressure of IPAP 25 / EPAP whatever?"StillAnotherGuest wrote:"Can what you're trying to fix really be fixed?"
If things are going reasonably well at reasonable pressures, and the person feels well rested every morning, why pursue rounding out every single last flow limitation, if to do that means increasing pressure to the point of mask seal difficulties, increased vent noise, aerophagia..... ?
What are you trying to fix?
And GFL when Level IV 2 channel "PSG" comes along.
SAG

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
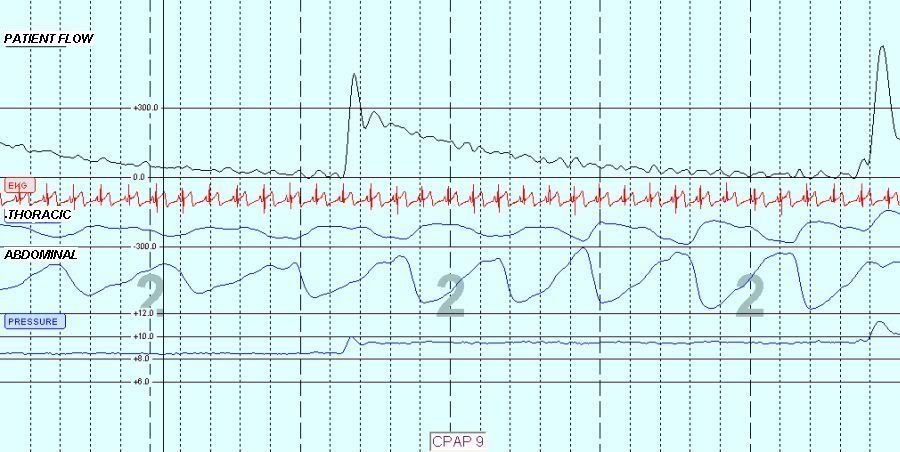
What Be Them Things Anyway?
OK, here's a great shot of "bumps" on the PB420E in Auto Mode. 30 second window. The patient flow was a separate transducer and not a machine output, so the acquisition rate and filters could be independently controlled. EKG is brought up close to the Patient Flow Rate to see if that's the cause of the artifact. This is an apnea, so there is no patient flow.
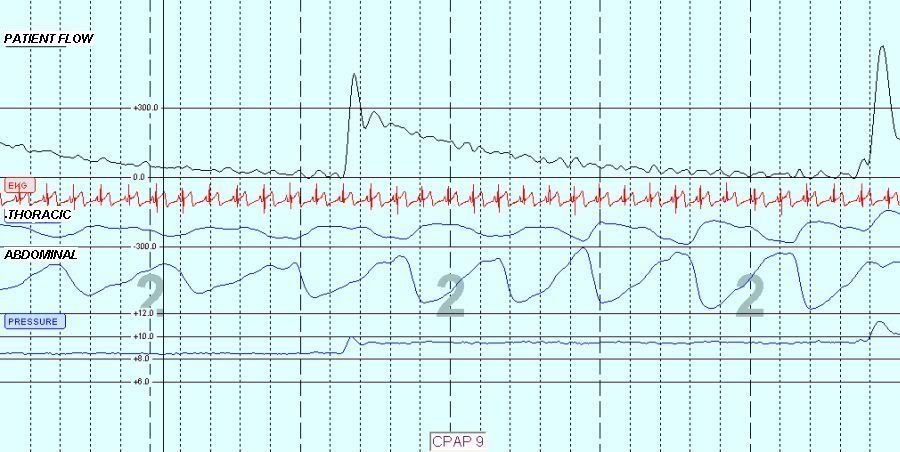
What is pretty clear is that the "bumps" are independent of patient effort as they merrily march through 8 respiratory cycles, so this is clearly not exclusively an expiratory phenomenon, be it "expiratory intolerance" or "expiratory flow limitation". And while the frequency of this phenomena is close to cardiac frequency, it doesn't match up perfectly, so I'm still not sure if that's it (or at least, entirely it).
SAG
What is pretty clear is that the "bumps" are independent of patient effort as they merrily march through 8 respiratory cycles, so this is clearly not exclusively an expiratory phenomenon, be it "expiratory intolerance" or "expiratory flow limitation". And while the frequency of this phenomena is close to cardiac frequency, it doesn't match up perfectly, so I'm still not sure if that's it (or at least, entirely it).
SAG

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
-
Guest
Dr. Krakow, I immensely enjoy your highly novel presentations here.
I expect the slight "resultant skewing" you see to be attributed to allowable energy-wave reflection. That energy-wave reflection would result from inevitable signal-line contour variations as well as characteristic-impedance mismatching.
The 420e machinery does not "inject" these pulsations while the other CPAP brands manage to avoid similar spurious noise injection. Rather, the 420e simply utilizes a narrow-diameter signal line that the other CPAP brands do not rely on. The 420e and stethoscope alike rely on narrow-diameter tubes to optimally channel the cardiac signal to either a flow-sensor (a delicate pressure-based transducer) or human ear.
-SWS
disclaimer: non-professional & non-expert.
Those skewed pulsations are very likely the result of the human heartbeat. The pulsations are really the result of pressure-wave based "cardiac oscillations" as they travel through: 1) the open human airway, and 2) the 420e narrow-diameter signal line (which is waveguide/wavelength optimized for this acoustic signal).And while the frequency of this phenomena is close to cardiac frequency, it doesn't match up perfectly, so I'm still not sure if that's it (or at least, entirely it).
I expect the slight "resultant skewing" you see to be attributed to allowable energy-wave reflection. That energy-wave reflection would result from inevitable signal-line contour variations as well as characteristic-impedance mismatching.
The 420e machinery does not "inject" these pulsations while the other CPAP brands manage to avoid similar spurious noise injection. Rather, the 420e simply utilizes a narrow-diameter signal line that the other CPAP brands do not rely on. The 420e and stethoscope alike rely on narrow-diameter tubes to optimally channel the cardiac signal to either a flow-sensor (a delicate pressure-based transducer) or human ear.
-SWS
disclaimer: non-professional & non-expert.
Sorry for not having logged in above.
Unfortunately the mask is the convenient place for you to measure. However, in signal processing physics trumps convenience every time. Since you are interested in measuring what the 420e sees in the transient domain, you would have one of two suitable options: 1) electronically collect your tandem measurements at the 420e flow sensor's leads, or 2) impedance-match as you flow-measure at the machine end of the 420e sensor line.
In the transient domain you see largely anomalous signal reflection when you measure acoustic signals at the wrong end of the signal line. Conversely, less delicate respiratory flow signals are suitable to measure at the mask and compare with what the 420e sees at the other end of the hose. Rock-solid constant pressure, on the other hand, can be measured anywhere in a pressurized circuit of reasonable length.
disclaimer: non-professional & non-expert.
Anyway, when you measure wave-guided cardiac oscillations at the mask, you unfortunately measure at the 420e signal-path midpoint. That means you're collecting transient-domain cardiac signals that have been largely wave-reflected....cardiac frequency, it doesn't match up perfectly, so I'm still not sure if that's it (or at least, entirely it).
Unfortunately the mask is the convenient place for you to measure. However, in signal processing physics trumps convenience every time. Since you are interested in measuring what the 420e sees in the transient domain, you would have one of two suitable options: 1) electronically collect your tandem measurements at the 420e flow sensor's leads, or 2) impedance-match as you flow-measure at the machine end of the 420e sensor line.
In the transient domain you see largely anomalous signal reflection when you measure acoustic signals at the wrong end of the signal line. Conversely, less delicate respiratory flow signals are suitable to measure at the mask and compare with what the 420e sees at the other end of the hose. Rock-solid constant pressure, on the other hand, can be measured anywhere in a pressurized circuit of reasonable length.
disclaimer: non-professional & non-expert.
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
That's A Lot Of It, But...
Well -SWS, I sure would have liked to simply attribute all of the pulsations to cardiac oscillations, but the discrepancy seen in Distinct PB420E Cardiac Pulsation Discord was just too great to dismiss without a closer look. I mean, cardiac oscillations simply do not shift position relative to the QRS. There are a number of other possibilities that need exploration first, including, for that matter, patient anatomy. But the point that I think really needs to be made is that a "bumpy" waveform on expiration, seen in Dr. Krakow's initial example, can have causes that are not appropriately addressed with an aggressive bilevel titration.-SWS-guested wrote:Those skewed pulsations are very likely the result of the human heartbeat. The pulsations are really the result of pressure-wave based "cardiac oscillations" as they travel through: 1) the open human airway, and 2) the 420e narrow-diameter signal line (which is waveguide/wavelength optimized for this acoustic signal).
I expect the slight "resultant skewing" you see to be attributed to allowable energy-wave reflection. That energy-wave reflection would result from inevitable signal-line contour variations as well as characteristic-impedance mismatching.
The 420e machinery does not "inject" these pulsations while the other CPAP brands manage to avoid similar spurious noise injection..
And again, these waveforms were obtained not through the 420E sensors, but 2 separate transducers with higher acquisition sampling and less filtering that one would see from the 420E signal.
I'm also going to contend that 420E (or any machine) will create pressure surges and valleys as it tries to maintain pressure during patient inspiration and expiration because it reacts mechanically. It just depends on how close you want to look.
To illustrate this, here's an interesting composite. Same patient on the PB420E. The respirations have been filtered out so just the pressure oscillations remain in patient flow (PTAF/CPAP) and abdomen. Breaths can be inferred from the CPAP Pressure. I believe that the Pressure fluctuations are due mainly to the machine increasing and decreasing flow in response to patient demand, and varying a bit from the "set" pressure (about +/- 1 cmH2O). The abdomen shows quite clearly the cardiac oscillations. And I believe that the Patient Flow (PTAF/CPAP) is a net of these 2 (at least) influences.

SAG

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
SAG wrote:But the point that I think really needs to be made is that a "bumpy" waveform on expiration, seen in Dr. Krakow's initial example, can have causes that are not appropriately addressed with an aggressive bilevel titration.
Interesting topic. Your above two statements do not seem to corroborate the same theory about those signal bumps.SAG wrote:I'm also going to contend that 420E (or any machine) will create pressure surges and valleys as it tries to maintain pressure during patient inspiration and expiration because it reacts mechanically.
At least here's what I'm thinking along those lines: If you attribute patient flow-variations largely to machine-sourced pressure bumps (on "any machine"), then aggressive bilevel titrations should theoretically accentuate those hypothetical machine-sourced flow bumps. But if the opposite happens--if the bumps actually smooth out during an aggressive titration--then those former bumps cannot be attributed to the machine pressure swings (which are now more drastic).
But I agree there are potentially many different reasons for those bumps. The question remains in my mind whether fixing those bumps via a novel application of BiLevel therapy accounts for significantly improved efficacy. I see what I think are many potentially productive techniques simultaneously occurring at Dr. Krakow's sleep center. So the question is which of his methods contribute to increased efficacy--and to what degree do each contribute?
-
BarryKrakowMD
- Posts: 65
- Joined: Wed Dec 05, 2007 12:48 am
- Contact:
Write A Book In Your Spare Time
Wow! The feedback and discussion are quite intense and honestly far above my background and training, probably my IQ as well. When I see you all writing in this manner while repeatedly suggesting that I write another book, I don't understand why you don't see that you are the people to write the next book. I'd bet the ranch that some combination of your group could write a multi-purpose manual and market it as an online resource. You might want to consider a medical editor or two to enhance "perceptual" credibility as well as to insure that you make accurate clinical links to your instructions. Seriously, I've been imagining a book coming from this group for some time now, given the impressive commentary I consistently read on these posts. You really do possess a level of expertise, if properly harnessed, that not only has distinctive market potential, but unquestionably you could assist a large number of frustrated PAP therapy users. So, it's financial rewards and altruism, the perfect combo!
The main response to what I've read through and to what I think I understand is much more pragmatic and I'm sure disappointing to many. However, I still believe it's clinically relevant, which is what I feel to be my strong suit in offering comments.
Whatever the cause of these perturbations of the airflow, I feel confident that the two extremes we see on expiration--pressure intolerance where the person is fighting with pressurized airflow and expiratory flow limitation in which the patient is suffering a breathing event similar (but not identical) to inspiratory flow limitation--are much more common in SDB patients during titrations than most sleep labs attend to.
Do I think this approach can lead to treating a waveform? I think that is certainly possible, and I'm sure I've seen such a problem in the lab, e.g. the curve won't round so we keep pushing the pressure, and yet it becomes obvious that we're barking up the wrong tree. But such an example is not our common experience.
The most common experience is as I've described previously. The patient is started on CPAP, and the expiratory limb gets bumpy somewhere along the way. Then, in the most obvious cases, the pressure intolerance results in iatrogenic central apneas. Switch the patient to bilevel, and voila, the central events abate along with nearly all of the expiratory intolerance. We have seen this phenomenon in probably 1000 patients, some with more obvious effects and some with more subtle. And, among this group were a sizeable number of patients using fixed CPAP pressures who came from other sleep centers. We put them in our lab, spotted the pressure intolerance, switched them to bilevel, and the next morning, they reported a higher sleep quality than previously achieved. So, experientially, I remain firmly convinced that these are genuine pressure intolerance problems. But, I remain very open to the idea that other variables are influencing this process.
Still, the bottom line for me is whether or not the patient is reporting what appears to be an optimal response. To clarify our perspective, we would not be satisfied with a reasonable response unless the patient chose that as his or her stopping point. We want to push the envelope because we are intrigued by the observations that some people with persistent fine-tuning appear to be able to essentially eliminate daytime sleepiness or night-time nocturia. Even more important, we're most impressed by the reported changes in cognitive function in which the patient continues to optimize their PAP therapy response and reports consistently clearer thinking.
Again, to repeat a concept we regularly use, we fear that many patients "normalize" their improvements, because they cannot imagine something better if they have never experienced the better in recent times. I agree that other factors influence symptoms, but let me provide the best example on how even this perspective misses the mark. We have seen innumerable patients who report prostate problems and declare this condition as the sole cause of their nocturia. Yet, in the vast majority of these men, the nocturia does not just decrease, it usually disappears. What does that say about the prostate influence? I'm not talking about a few isolated cases; in our experience most men with prostate problems and SDB report complete elimination of nocturia. Of course, the real test would be to evaluate patients from a Urology Clinic and see what proportion eliminate nocturia with PAP therapy and what differences might be found between CPAP vs. Bilevel?
Rest Wishes.
The main response to what I've read through and to what I think I understand is much more pragmatic and I'm sure disappointing to many. However, I still believe it's clinically relevant, which is what I feel to be my strong suit in offering comments.
Whatever the cause of these perturbations of the airflow, I feel confident that the two extremes we see on expiration--pressure intolerance where the person is fighting with pressurized airflow and expiratory flow limitation in which the patient is suffering a breathing event similar (but not identical) to inspiratory flow limitation--are much more common in SDB patients during titrations than most sleep labs attend to.
Do I think this approach can lead to treating a waveform? I think that is certainly possible, and I'm sure I've seen such a problem in the lab, e.g. the curve won't round so we keep pushing the pressure, and yet it becomes obvious that we're barking up the wrong tree. But such an example is not our common experience.
The most common experience is as I've described previously. The patient is started on CPAP, and the expiratory limb gets bumpy somewhere along the way. Then, in the most obvious cases, the pressure intolerance results in iatrogenic central apneas. Switch the patient to bilevel, and voila, the central events abate along with nearly all of the expiratory intolerance. We have seen this phenomenon in probably 1000 patients, some with more obvious effects and some with more subtle. And, among this group were a sizeable number of patients using fixed CPAP pressures who came from other sleep centers. We put them in our lab, spotted the pressure intolerance, switched them to bilevel, and the next morning, they reported a higher sleep quality than previously achieved. So, experientially, I remain firmly convinced that these are genuine pressure intolerance problems. But, I remain very open to the idea that other variables are influencing this process.
Still, the bottom line for me is whether or not the patient is reporting what appears to be an optimal response. To clarify our perspective, we would not be satisfied with a reasonable response unless the patient chose that as his or her stopping point. We want to push the envelope because we are intrigued by the observations that some people with persistent fine-tuning appear to be able to essentially eliminate daytime sleepiness or night-time nocturia. Even more important, we're most impressed by the reported changes in cognitive function in which the patient continues to optimize their PAP therapy response and reports consistently clearer thinking.
Again, to repeat a concept we regularly use, we fear that many patients "normalize" their improvements, because they cannot imagine something better if they have never experienced the better in recent times. I agree that other factors influence symptoms, but let me provide the best example on how even this perspective misses the mark. We have seen innumerable patients who report prostate problems and declare this condition as the sole cause of their nocturia. Yet, in the vast majority of these men, the nocturia does not just decrease, it usually disappears. What does that say about the prostate influence? I'm not talking about a few isolated cases; in our experience most men with prostate problems and SDB report complete elimination of nocturia. Of course, the real test would be to evaluate patients from a Urology Clinic and see what proportion eliminate nocturia with PAP therapy and what differences might be found between CPAP vs. Bilevel?
Rest Wishes.
_________________
| Humidifier: HC150 Heated Humidifier With Hose, 2 Chambers and Stand |
| Additional Comments: Puritan Bennett Breeze Nasal Pillows; ResMed Mirage Quattro FFM; Respironics Premium Chinstrap; Breath Right Nasal Strips |
Barry Krakow, MD
Blogging at Fast Asleep (Sign up: https://fastasleep.substack.com/embed
Books & Videos at http://www.barrykrakowmd.com
Practice at http://www.barrykrakowmd.com
Blogging at Fast Asleep (Sign up: https://fastasleep.substack.com/embed
Books & Videos at http://www.barrykrakowmd.com
Practice at http://www.barrykrakowmd.com









