Progressive sleep apnea?
Re: Progressive sleep apnea?
You need to listen to the pulmonologist who wants to help you manage your therapy better with probably the ASV type of machine. It's in the toilet right now.
When I say "don't obsess over numbers" it doesn't mean ignore stuff like you are showing here.. It's meant for people going into panic mode when the AHI goes from 1.5 to 2.5 and they are all centrals. Or for people who have a bad AHI night once a month of maybe 6.2 but all the other nights nicely below 5.0.
No way would I have suggested that anyone pooh pooh off a report like this.
I suspect your doc is thinking that you have developed Complex Sleep Apnea...while not extremely common it isn't all that rare either.
If it is Complex Sleep Apnea going on then this video might help you understand what is happening
https://www.youtube.com/watch?v=CU-XTcf ... e=youtu.be
I don't know for sure this is what we are seeing but it sure is suspicious for it and you need to be talking AND listening to the doctor about it.
I don't know what to make of the RT telling you "everything's fine" unless he was seeing something totally different way back when things might have been better. I don't know what he looked at or even if he looked at anything beyond hours of use.
Or else he's an idiot..which wouldn't be the first time.
When I say "don't obsess over numbers" it doesn't mean ignore stuff like you are showing here.. It's meant for people going into panic mode when the AHI goes from 1.5 to 2.5 and they are all centrals. Or for people who have a bad AHI night once a month of maybe 6.2 but all the other nights nicely below 5.0.
No way would I have suggested that anyone pooh pooh off a report like this.
I suspect your doc is thinking that you have developed Complex Sleep Apnea...while not extremely common it isn't all that rare either.
If it is Complex Sleep Apnea going on then this video might help you understand what is happening
https://www.youtube.com/watch?v=CU-XTcf ... e=youtu.be
I don't know for sure this is what we are seeing but it sure is suspicious for it and you need to be talking AND listening to the doctor about it.
I don't know what to make of the RT telling you "everything's fine" unless he was seeing something totally different way back when things might have been better. I don't know what he looked at or even if he looked at anything beyond hours of use.
Or else he's an idiot..which wouldn't be the first time.
_________________
| Machine: AirCurve™ 10 VAuto BiLevel Machine with HumidAir™ Heated Humidifier |
| Additional Comments: Mask Bleep Eclipse https://bleepsleep.com/the-eclipse/ |
Last edited by Pugsy on Wed May 14, 2014 10:55 am, edited 1 time in total.
I may have to RISE but I refuse to SHINE.
Re: Progressive sleep apnea?
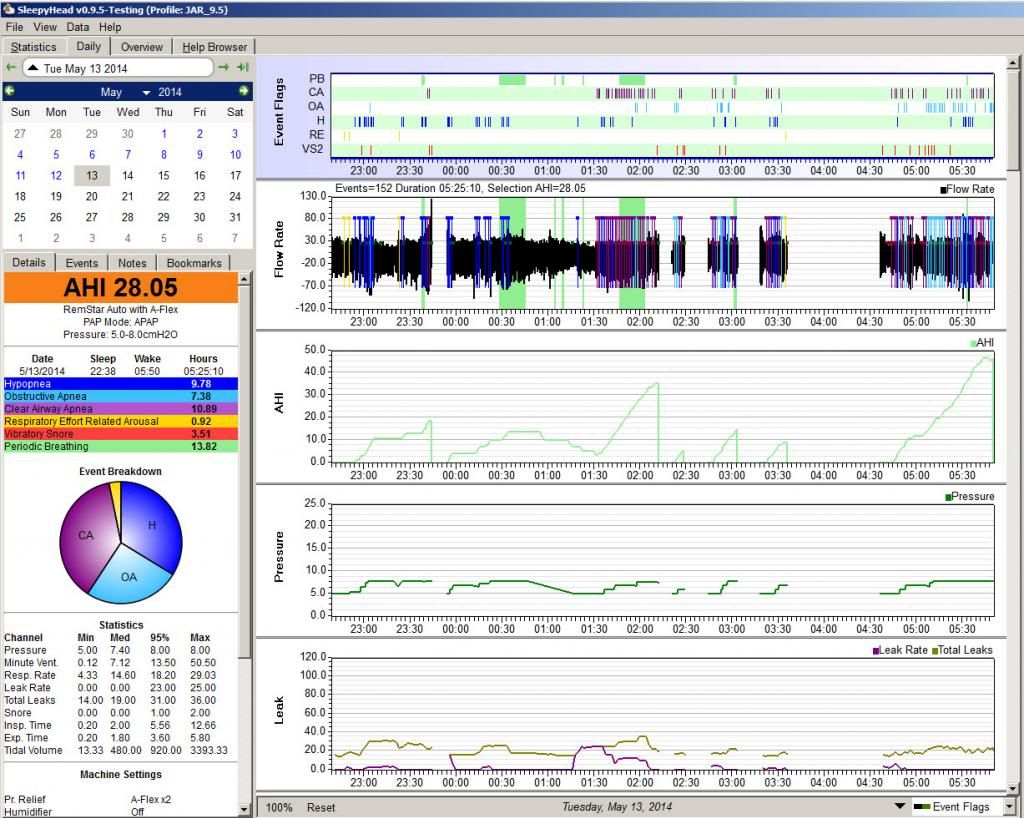
If this is typical of what your detailed data looks like, the pulmonologist is rightly concerned:
- The AHI is way, way too high
- The CAI makes up at least 50% of the AHI.
- The CAI all by itself is way too high.
- There's periodic breathing with a lot of Hs and CAs being scored, so some of the Hs are likely CA-wannabes instead of OA-wannabes. It's also possible that some of the OAs scored during the PB episodes are misscored CAs rather than OAs or perhaps they'd be scored as "mixed apneas" on an in-lab sleep test.
- The amount of PB itself is NOT insignificant.
- And the leak line is very reasonable. Even when the leaks are at their worst, they're no where near Large Leak territory for you machine. So we can trust that the AHI and PB data is reasonably accurate.
So listen to your doc: There's real solid evidence that supports the doc's hypothesis that you are dealing with Emergent Central Apnea (or Complex Sleep Apnea) issues. And in that case it does make sense to be talking about a switch to an ASV machine because the CAs are happening at relatively low PAP pressures.
In other words, you real question should be directed at the RT who's been telling you things are fine for several months: How the heck anybody with a half a brain who knows anything at all about PAP therapy could look at (multiple) reports like this one and tell a patient, "[Your] CPAP (software) results are good" is beyond belief. All I can think of is that the RT has never actually looked at any of the data beyond the usage data. Or, (to be more generous to the RT), perhaps the first few reports were substantially better and things started to go downhill more recently. In which case the RT still should have said something when things started to go downhill.
So I repeat: If this is typical of the kind of data you are seeing on multiple nights each week, it is CRITICALLY important for you to pay attention to what your pulmonologist is saying. You are actually LUCKY to have a pulmonologist who is LOOKING at this kind of data and telling you that something is wrong and that an ASV may be what you need.
If there's more to the story, you need to fill us in. And, more importantly, you need to fill you pulmonologist in on what's going on when you have nights that look as bad as this one does.Some things went on in this reading that I’ll inform you of later after I get a couple ‘reads’ on the data.
There's no need to be embarrassed. A lot of people (including me) post here as way of paying it forward. If it were not for the substantial help and emotional support I got from the good folks here at cpaptalk, I would not have managed to become a relatively successful PAPer. And paying it forward by helping others who are clearly in need of some real advice is something that gives me real satisfaction.Please don’t do this unless you enjoy it. I’m embarrassed at all of you good people’s time I’ve taken up with my questions.
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |
Re: Progressive sleep apnea? Pressure Too Low
IMNMO (In My Non-Medical Opinion) INCREASE THE PRESSURE!
5-8cmH20 is pretty low. Is it not obvious that the immediate first step (which is simple to do but nobody makes any money on it, unlike endless "sleep studies") should be to see the effect of an increased pressure? It just seems like common sense.
Please feel free to disagree, I love to learn
_________________
| Mask: Mirage™ FX Nasal CPAP Mask with Headgear |
| Additional Comments: 14cmH20, User since 1999, SleepyHead Software, Apria, Anthem BlueCross California Silver EPO via Covered California |
Re: Progressive sleep apnea?
Okay. I will be the first to disagree. Under normal circumstances for the OAs and Hyponeas , if the centrals weren't present..yeah more pressure but in this situation with all the centrals...more pressure could very well make things a whole lot worse.cdean wrote:IMNMO (In My Non-Medical Opinion) INCREASE THE PRESSURE!
5-8cmH20 is pretty low. Is it not obvious that the immediate first step (which is simple to do but nobody makes any money on it, unlike endless "sleep studies") should be to see the effect of an increased pressure? It just seems like common sense.
Please feel free to disagree, I love to learn
The last thing we want to do is anything that might make the centrals increase in number and there's a real good chance they would with more pressure. Centrals are NOT treated with more pressure from an APAP machine. They won't respond except by likely increasing in numbers instead of decreasing and that could be very dangerous to someone.
Reports like this with this number of centrals...not something for dial a winging pressures and DIYing . This person needs to be getting with his doctor and not go changing stuff on his own.
Going up in pressure all by himself is the LAST thing he should be considering..it could be potentially very harmful. Very dangerous.
So for your learning process...remember that while it's okay and normal to have a handful of centrals (Clear Airway events on this report) and it not be a big deal...it is NOT normal to see them in this number and we never advised increasing pressure in situations like this. This person needs to be directly under a doctor's care. At this point we don't know if the centrals are related to pressure or if he would have them even without cpap therapy but all that is best left to his doctor and not us as much as we wish we could help.
We never ever want to offer an idea that remotely might hurt someone and in this instance...increasing the pressure might just do that.
_________________
| Machine: AirCurve™ 10 VAuto BiLevel Machine with HumidAir™ Heated Humidifier |
| Additional Comments: Mask Bleep Eclipse https://bleepsleep.com/the-eclipse/ |
I may have to RISE but I refuse to SHINE.
Re: Progressive sleep apnea?
A few details:
I don’t remember (I can assume I was sleeping) the 2230 to 0215 segment. (I must’ve woken, and turned the machine off at around 23:45, probably for a bathroom break.)
At around 2:15 I got up fairly frequently (for some reason I always think a lot more time has gone by) and did little more than (turn the machine off and) just sit by the side of the bed waiting for my nasal passages to clear (this is not the type of thing that required blowing my nose or the equivalent).
From 0330 to 0430 I got up, went downstairs and read.
From 0430 to 0545 I did not get up. Instead I breathed as well as I could, often compensating nasal breathing with: nasal-in/mouth-out. It’s hard to explain why my body uses this strategy.
I don’t remember (I can assume I was sleeping) the 2230 to 0215 segment. (I must’ve woken, and turned the machine off at around 23:45, probably for a bathroom break.)
At around 2:15 I got up fairly frequently (for some reason I always think a lot more time has gone by) and did little more than (turn the machine off and) just sit by the side of the bed waiting for my nasal passages to clear (this is not the type of thing that required blowing my nose or the equivalent).
From 0330 to 0430 I got up, went downstairs and read.
From 0430 to 0545 I did not get up. Instead I breathed as well as I could, often compensating nasal breathing with: nasal-in/mouth-out. It’s hard to explain why my body uses this strategy.
- - One reason seems to be that it is much harder to breath out against the air pressure;
- Second reason: it’s a reset mechanism. Breathing out through the mouth seems to restore some sort of pressure-balance through which it is easier both to breathe in and breathe out.
ResMed Air Curve 10 ASV w. humidifier
PR S1 REMstar 60 Series BiPAP ASV Advanced & PR S1 with humidifier
Various Nasal masks or Nasal pillows
Software:
PR S1 REMstar 60 Series BiPAP ASV Advanced & PR S1 with humidifier
Various Nasal masks or Nasal pillows
Software:
Re: Progressive sleep apnea? Pressure Too Low
Piggybacking on what pugsy said:cdean wrote: IMNMO (In My Non-Medical Opinion) INCREASE THE PRESSURE!
Given the number of CENTRAL apneas (a CAI = 10.89) AND the history of afib AND the periodic breathing, there is a very real chance that AfibApnea is dealing with Central Sleep Apnea or Complex Sleep Apnea. And remember that AfibApnea's pulmonologist has told AfibApnea that he (the pulmonologist) is very concerned that AfibApnea DOES have problems with Central Apnea that has emerged with the start of PAP therapy. And if the doc is correct, then INCREASING the pressure is the WRONG thing to do!!
In Complex Sleep Apnea (CompSA), the problem is that CPAP/APAP pressure causes the central apneas to happen. And increasing the CPAP/APAP pressure often INCREASES the problem rather than making it better.
In Central Sleep Apnea (CSA), additional pressure does NOT bring the number of CAs down because the CAs are NOT caused by a collapsed airway. And in someone with CSA,there is always a risk that if the pressure is increased, the unstable breathing patterns that cause CSA can be made worse. And so an increase in pressure CAN make the CSA problem worse.
So to suggest "increase the pressure" (aka dial winging) to anyone with this many centrals showing up on their reports is NOT merely naive, it MAY BE down right dangerous to the person if they follow the advice to just increase the pressure.
And it's important to all of us for us to remember to first do no harm when we are offering advice.
No. It is NOT obvious that the first thing to do is to increase the pressure in this particular case.5-8cmH20 is pretty low. Is it not obvious that the immediate first step (which is simple to do but nobody makes any money on it, unlike endless "sleep studies") should be to see the effect of an increased pressure? It just seems like common sense.
Please feel free to disagree, I love to learn
In an effort to inform and educate:
First, "low pressure" is in the airway of the patient. For many people on this board, their pressure needs are relatively high (anything over 10cm is "excessively high" in my sensitive airway's view). But NOT everybody needs a pressure that is above 8 or 9 cm. And there is NOTHING wrong with using a lower than average pressure range or setting if that's all you need.
Second, there are a lot of folks who have airways and bodies that are VERY sensitive to pressure issues. And any increase in their "low pressure" setting can lead to more problems than it fixes. And when a good sleep doc is dealing with such a patient, there is a lot of work involved in finding out both a PAP mode (CPAP? APAP? BiPAP? BiPAP Auto? ASV?) that can provide sufficient pressure to take care of the obstructive events without triggering the pressure induced problems. Dial winging without the aid of a doc is often counterproductive for people who are very sensitive to pressure.
For some of us who are unlucky enough to be very sensitive to pressure, the problem is rather straightforward and only deals with comfort issues. In my case if my EPAP pressure is AT or ABOVE 6cm for most of the night, I'll wake up with a distended stomach full of painful aerophagia. If my EPAP stays below 6 cm for 50% or more of the night and NEVER goes above 6cm, I'm usually fine when it comes to the aerophagia. I'm fortunate that my OSA is controlled AND my painful aerophagia is controlled when I run my BiPAP in Auto mode with settings that make little or no sense compared to what "common wisdom" says BiPAP settings should look like. I'm also fortunate to have a sleep doc who understands that.
But the really unlucky ones are like AfibApnea: Even very low pressures (as in 5-8cm) CAN trigger pressure induced central apneas in SOME patients. And many of these folks find themselves in the same conundrum that AfibApnea is in: The pressure required to properly control the OSA is unfortunately high enough to trigger clinically significant problems with CSA or CompSA. And these folks absolutely have to work with their sleep doc to find a mode of PAP therapy that both works on the OSA stuff and also does NOT trigger the CSA/CompSA stuff. And that usually means being switched to an ASV machine.
AfibApnea's case is a really fine example of this very real conundrum: 5-8cm does NOT seem to be high enough to control his obstructive events (the treated OAI = 7.38), but 5-8cm also seems to be enough pressure to induce some really serious problems with central apneas---that CAI = 10.89 cannot be ignored given the facts that (a) this report is "typical" of what's been going on recently AND (b) AfibApnea's history of afib AND (c) AfibApnea's doctor is worried about central sleep apnea issues emerging since AfibApnea started PAP therapy.
To conclude: To suggest to AfibApnea that his problems can be fixed by bumping up the pressures in not merely foolish, it may actually be harmful.
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |
Re: Progressive sleep apnea?
Not really unless you can tell us that you were awake for a large part of the night that the machine was on and you were using it when all those centrals popped up.AfibApnea wrote: Does this explanation explain anything or cause you to change the way you read the data?
The breaks in the therapy...don't really matter why as they are easy to spot.
Awake breathing irregularities can sometimes cause the machine to flag events that wouldn't be flagged otherwise. The machine doesn't know if you were awake or asleep. It just calls the breathing like it sees it.
So if you were fully awake and laying there in bed for hours with the machine on...then it might explain some of those ugly centrals but I still think you need to get with your doctor. To blame all those centrals on awake breathing would be stretch and I for one am not comfortable pooh poohing off that many of centrals based on what we can get from these reports and we simply cannot tell for sure if you were awake when all that ugliness shows up.
So my advice is unchanged....see your doctor and do what he says.
_________________
| Machine: AirCurve™ 10 VAuto BiLevel Machine with HumidAir™ Heated Humidifier |
| Additional Comments: Mask Bleep Eclipse https://bleepsleep.com/the-eclipse/ |
I may have to RISE but I refuse to SHINE.
Re: Progressive sleep apnea?
So there's a good chance that the excessively large number of CAs scored between 1:30 and 2:00 AND the PB scored during 0:30-0:45 and 1:45-2:00 are the REAL thing. And because the PB is likely really there, some or all of those Hs scored between 0:15-0:40 may be central rather than obstructive. There's no way to tell which they are from the CPAP data; that really requires the data gathered in a full in-lab PSG study. The data from 22:30 to 2:15 is still strong enough to support your doc's idea that you may be dealing with emergent central apnea of some sort.AfibApnea wrote:A few details:
I don’t remember (I can assume I was sleeping) the 2230 to 0215 segment. (I must’ve woken, and turned the machine off at around 23:45, probably for a bathroom break.)
So some of the stuff going on between 2:15 and 4:30 may be sleep/wake/junk---i.e. irregular wake breathing patterns mixed in and getting misscored by the machine as OAs, Hs, and CAs. But it could also be the case that every time you started to drift off to sleep, your breathing became unstable and the CAs started to emerge. Only an in-lab sleep test can really distinguish between sleep/wake/junk and clinically significant problems with transitional central apneas.At around 2:15 I got up fairly frequently (for some reason I always think a lot more time has gone by) and did little more than (turn the machine off and) just sit by the side of the bed waiting for my nasal passages to clear (this is not the type of thing that required blowing my nose or the equivalent).
So the gap in the data is easily explained.From 0330 to 0430 I got up, went downstairs and read.
Again though the question is how much sleep did you get during this time? And I don't mean your impression of how much sleep---I know you think you were awake the entire time.From 0430 to 0545 I did not get up. Instead I breathed as well as I could, often compensating nasal breathing with: nasal-in/mouth-out. It’s hard to explain why my body uses this strategy.
But just like we don't remember short wakes when we're sleeping well, we also don't remember short sleeps when we're lying in bed fighting to get back to sleep. And so again the question becomes teasing out sleep/wake/junk patterns that don't mean anything from transition to sleep problems that DO mean something significant.
That said, let's look at what you're describing as your breathing pattern:
What you are describing is call "exhalation puffs" and they're actually recorded on either the F&P or Devillbass PAPs as I recall. But they can also be described as "Pursed Lip Breathing" that is commonly used by people with COPD (in the daytime as well as at night).Instead I breathed as well as I could, often compensating nasal breathing with: nasal-in/mouth-out. It’s hard to explain why my body uses this strategy.
- - One reason seems to be that it is much harder to breath out against the air pressure;
- Second reason: it’s a reset mechanism. Breathing out through the mouth seems to restore some sort of pressure-balance through which it is easier both to breathe in and breathe out.
Exhalation puffs are often considered a potential problem for getting CPAP therapy optimized.
Part of this is that when your are exhaling through your mouth there's a chance that you are losing therapeutic pressure. (Although at your pressure range, that's not likely to be as big of a problem as it would be for someone using a higher pressure setting.
Another reason that exhalation puffs can be problematic is that they can confuse the machine about the breathing pattern, leading to the scoring of false events. (And also occasionally making it easier for a machine to miss scoring a real event.)
Exhalation puffs would also explain why you notice the exhaust flow so much more on your inhalations rather than your exhalations: When you are exhaling through your mouth, much (perhaps most) of the venting is being done through your mouth and NOT through the exhaust vents. But as soon as you close the mouth at the start of the inhalation, all the venting from the system is once again through the mask's exhaust vents. So of course it's much more noticeable.
Since you are doing a lot of exhalation puff breathing, the bigger issue that has to be addressed is: Why are you finding it so much more difficult to exhale through your nose? You may think it's just "congestion". But given the afib, I beginning to wonder if there isn't something more to this. Are you ever short of breath during the daytime? Do you ever do the exhale puffs when you are NOT trying to use the CPAP? Do you do a lot of chest breathing? Or are you mainly a diaphragmatic breather?
You could try increasing the Flex from 2 to 3: That will provide a bit more exhalation relief pressure at the beginning of the exhalation, which should make it easier to exhale. But if switching from Flex = 2 to Flex = 3 makes the problem WORSE rather than better, then there's a chance that part of what's driving your discomfort on exhalation is the fact that the PR System One's Flex system starts to increase the pressure before the end of the exhalation. And in some super sensitive folks (like me) that subtle increase in the pressure during the second half of the exhalation can make it feel as though it is very diffiult to fully exhale against the machine. And in that case? Turning Flex off completely make make it easier to exhale.
But the long term solution to the exhalation problem may be a switch to a different machine. Both a BiPAP and ASV will have two distinct pressures: One for inhalations (IPAP) and one for exhalations (EPAP). And the machine can be set up so that there is NO pressure increase until the beginning of the inhalation is detected (in "spontaneous" mode) OR when an ASV machine decides that it needs to start "triggering" inhalations because your breathing pattern is unstable and you are at high risk of having a cluster of CAs get started.
Not really.Does this explanation explain anything or cause you to change the way you read the data?
I'm willing to consider the data collected AFTER 2:15 as possibly having significant sleep/wave/junk patterns, but that does NOT explain the data collected between 22:30 and 2:15, when you don't remember any serious restlessness. And the data between 0:15 and 2:15 is pretty troubling and has way too many CAs for me to be comfortable saying that it's ok to ignore the possibility of CompSA or CSA being a issue.
And given your history of afib and the fact that your sleep doc has good reasons to worry about the possibility of CompSA or CSA, I'm inclined to think that this stuff needs to be properly investigated in an in-lab sleep test, even though that's not a comfortable thing to deal with.
Out of curiosity, could you post a more typical night's data---one where you don't remember being awake for most of the night???
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |
Re: Progressive sleep apnea?
And just to be very,very clear:robysue wrote:Not really.AfibApnea wrote:Does this explanation explain anything or cause you to change the way you read the data?
In light of the data between 0:15 and 2:15, I really think you need to LISTEN to your pulmonologist and do what he recommends.
There's a very real possibility of CompSA or CSA issues here and they need to be properly investigated. And if the in-lab sleep test backs up the doc's hypothesis that centrals are NOW a very real issue affecting your sleep, and the doc recommends a switch to an ASV machine, you should follow the doc's advice and (at the same time) be grateful that you don't have a doc who simply ignores this kind of data and just tells you to keep on trying "harder" at APAP.
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |
Re: Progressive sleep apnea?
Thanks! I appreciate the opportunity to learnPugsy wrote:Okay. I will be the first to disagree. Under normal circumstances for the OAs and Hyponeas , if the centrals weren't present..yeah more pressure but in this situation with all the centrals...more pressure could very well make things a whole lot worse.cdean wrote:IMNMO (In My Non-Medical Opinion) INCREASE THE PRESSURE!
5-8cmH20 is pretty low. Is it not obvious that the immediate first step (which is simple to do but nobody makes any money on it, unlike endless "sleep studies") should be to see the effect of an increased pressure? It just seems like common sense.
Please feel free to disagree, I love to learn
_________________
| Mask: Mirage™ FX Nasal CPAP Mask with Headgear |
| Additional Comments: 14cmH20, User since 1999, SleepyHead Software, Apria, Anthem BlueCross California Silver EPO via Covered California |
Re: Progressive sleep apnea? Effect of Pressure on Cental Apneas
Thanks so much for the info!robysue wrote:Piggybacking on what pugsy said:cdean wrote: IMNMO (In My Non-Medical Opinion) INCREASE THE PRESSURE!
In Complex Sleep Apnea (CompSA), the problem is that CPAP/APAP pressure causes the central apneas to happen. And increasing the CPAP/APAP pressure often INCREASES the problem rather than making it better.
Can you direct me to published studies that might have a title like The Effect of CPAP/APAP Pressure on Central Apneas ?
I would love to learn a bit more about this.
_________________
| Mask: Mirage™ FX Nasal CPAP Mask with Headgear |
| Additional Comments: 14cmH20, User since 1999, SleepyHead Software, Apria, Anthem BlueCross California Silver EPO via Covered California |
Re: Progressive sleep apnea? Effect of Pressure on Cental Apneas
The relationship between pressure and emergent central apneas is "the elephant in the room" amongst the sleep medicine community these days.cdean wrote:Thanks so much for the info!robysue wrote:Piggybacking on what pugsy said:cdean wrote: IMNMO (In My Non-Medical Opinion) INCREASE THE PRESSURE!
In Complex Sleep Apnea (CompSA), the problem is that CPAP/APAP pressure causes the central apneas to happen. And increasing the CPAP/APAP pressure often INCREASES the problem rather than making it better.
[/b]
Can you direct me to published studies that might have a title like The Effect of CPAP/APAP Pressure on Central Apneas ?
I would love to learn a bit more about this.
They dance around it in amazing ways.
But look into “apneic threshold” “sleep apnea ventilatory instability” “central sleep apnea (non-hypercapnic)” “sleep apnea carbon dioxide maintenance” “sleep apnea high respiratory control loop gain” as a search in Google Scholar or PubMed, and take note (especially in articles before about 2006) of how they induce centrals (they used to simply call it non-invasive pressure but now go as far as to use ASV type equipment to hide what is actually going on).
For myself I have found that there is a pressure which will prevent obstructions. And there is a pressure where centrals emerge en masse. And that stress can cause the pressure which will prevent obstruction to be more than that which induces centrals. Higher pressure more centrals. Yup.
But if either an obstructive or a central apnea occur the body changes. The inflammation in the body increases (tending toward more obstructive apneas) AND the respiratory control loop gain is raised. Since pressure is also a gain factor in the respiratory control loop the pressure at which a central will be induced decreases.
The situation can rapidly become unsolvable with CPAP which is why I use EERS.
May any shills trolls sockpuppets or astroturfers at cpaptalk.com be like chaff before the wind!
Re: Progressive sleep apnea?
While this last page of responses were coming in Mr. Hyde turned into Dr. Jekyl. (and this is what makes the matter so confusing for me)
I was so tired last night that I felt I needed to take a rest. I limited the time to 2 hours. Here's the CPAP output. How does this change things?

I was so tired last night that I felt I needed to take a rest. I limited the time to 2 hours. Here's the CPAP output. How does this change things?

ResMed Air Curve 10 ASV w. humidifier
PR S1 REMstar 60 Series BiPAP ASV Advanced & PR S1 with humidifier
Various Nasal masks or Nasal pillows
Software:
PR S1 REMstar 60 Series BiPAP ASV Advanced & PR S1 with humidifier
Various Nasal masks or Nasal pillows
Software:
Re: Progressive sleep apnea?
In SleepyHead the top panel represents the entire night. But in any chart you can "zoom in" on a particular section by dragging across it. Then you can drag across the top panel to "reset" if desired.AfibApnea wrote:While this last page of responses were coming in Mr. Hyde turned into Dr. Jekyl. (and this is what makes the matter so confusing for me)
I was so tired last night that I felt I needed to take a rest. I limited the time to 2 hours. Here's the CPAP output. How does this change things?
Once you drag across a section in a chart all charts set to look at the "zoomed in" time slot.
I would love to see a "zoom in" set of charts looking at 14:36 to 14:40 and 15:20 to 15:24 on the May 14th data.
Thanks
May any shills trolls sockpuppets or astroturfers at cpaptalk.com be like chaff before the wind!
Re: Progressive sleep apnea?
In my non doctor's opinion? Not much.How does this change things?
You still have way too much periodic breathing going on. And even at this scale, the wave flow pattern from 15:00 to 15:40 is potentially troubling---particularly where the green bars indicating the PB are located.
Yes, there are many fewer events scored. And only two CAs. But most of the Hs are scored VERY NEAR or IN the the areas flagged as periodic breathing. And hence, there is still a higher than normal chance that some (or all) of these hypopneas are central in nature rather than obstructive.
Given your afib, the PB is a concern and PB is NOT addressed by simply increasing the PAP pressure. The amount of PB may be indicating that you are having some trouble maintaining the proper CO2 levels in your blood. And it is the CO2 level that triggers the respiration drive. Full blown Chenye-Stokes breathing (which you may or may not have) is a form of periodic breathing that is commonly associated with some forms of heart disease (including afib as I recall). And it is quite possible that once your PB really gets going, you will start having CAs or central Hs at the nadir of each and every waxing/waning breathing cycle.
The waxing and waning of the size of the breaths in the PB cycle are largely driven by the body's inability to respond correctly (or to correctly maintain) the appropriate CO2 levels in the blood. During the waxing part of the cycles, the breaths become larger and larger, which leads to hyperventilation and blowing off too much CO2, which in turn leads to a depressed respiratory drive and the breaths become shallower and shallower. Eventually they may (momentarily) stop for several seconds (and a Central Apnea occurs) OR the respiration is reduced enough that a central H occurs. During this part of the cycle, not enough CO2 is blown off in the exhalations and the CO2 levels start to increase. Eventually the increasing CO2 levels lead to increasing respiratory effort, which once again leads to hyperventilation and blowing off too much CO2 and the cycle starts over.
The real problems with central and complex sleep apnea start when the CO2 overshoot/undershoot cycle are severe enough to trigger a CA or a central H at the nadir of each and every single waxing/waning cycle. That's not happening here (yet), but it is not unreasonable to suspect that some (maybe all) of the eight Hs scored after (roughly) 15:00 are potentially related to periodic type breathing and may be central in nature rather than obstructive.
Once again I close with this: Given your history of afib AND the amount of PB in your reports AND the distribution of the events relative to the PB AND the history of high numbers of CAs on some of your reports, you need to listen to your doctor when he says that he's worried about whether you are developing problems with (potentially pressure induced) central apneas. It is worth having the sleep test done (but you should ask about exactly what the study parameters are). And if the end result is a recommendation that you switch to AVS, then you ought to follow your doc's advice.
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |