AfibApnea wrote:This is a lot of posts of my apnea results and a lot of information to go through.
The main pieces of information that pugsy and I have repeatedly tried to convey boil down to these two points:
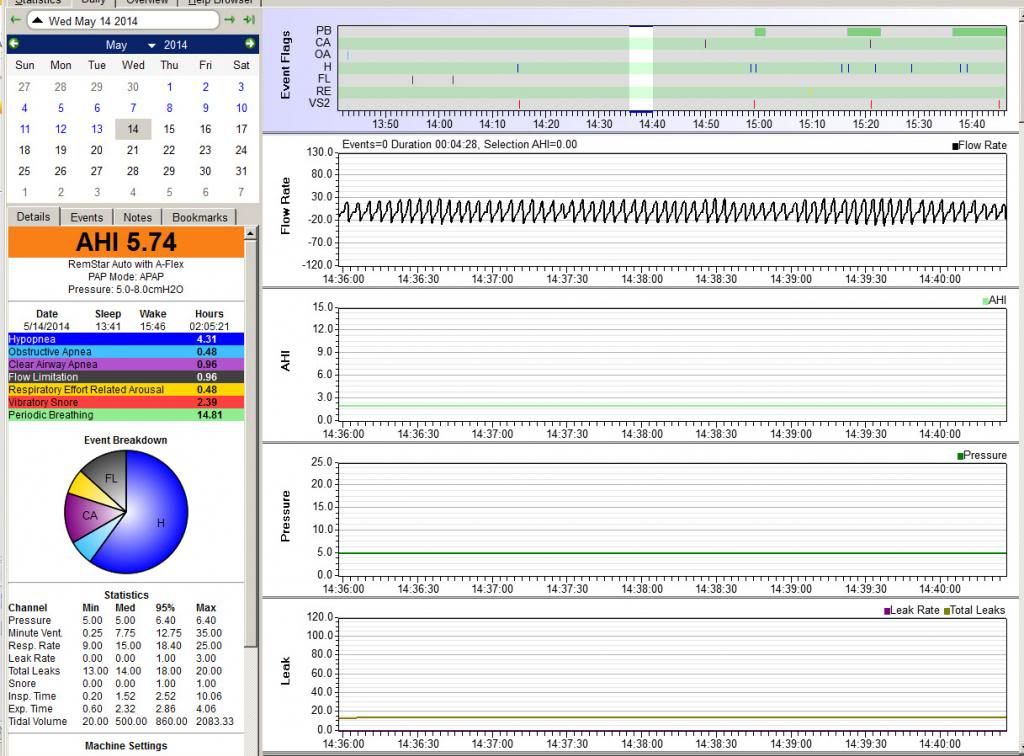
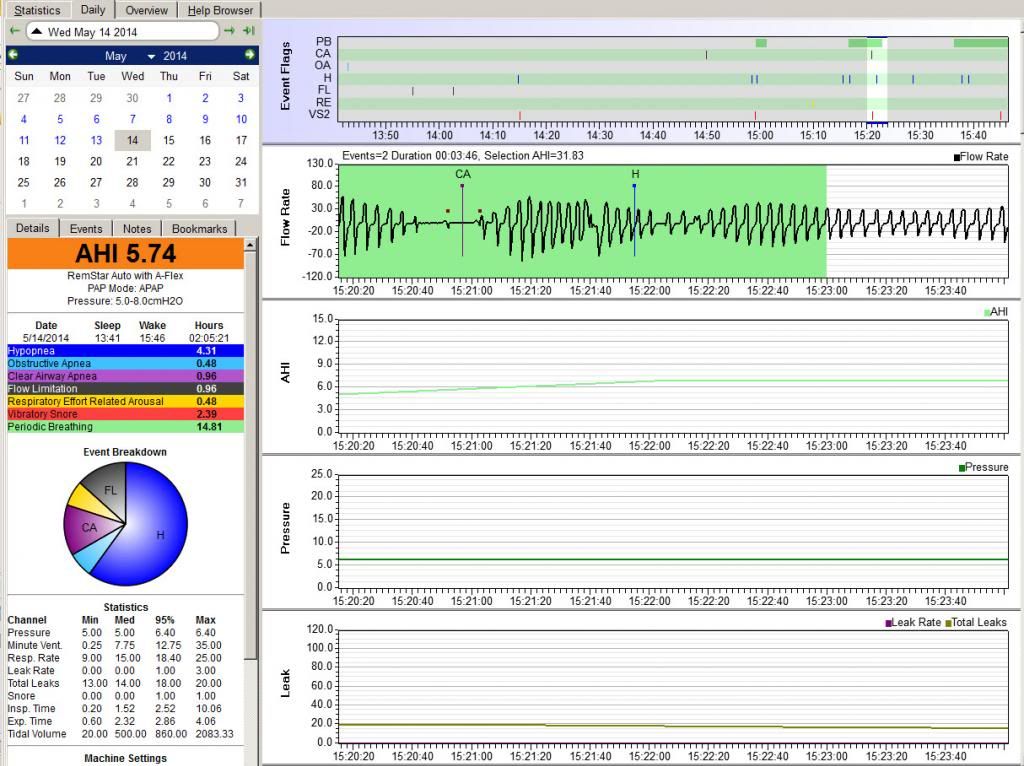
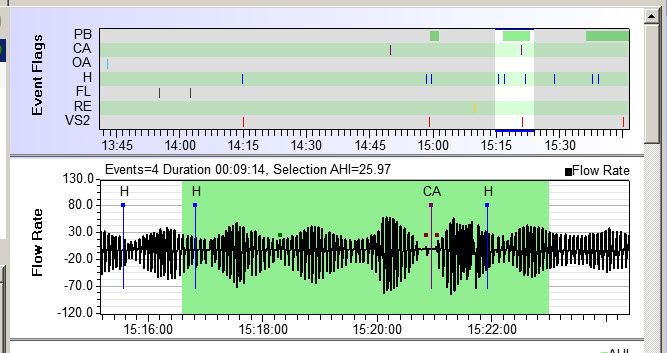
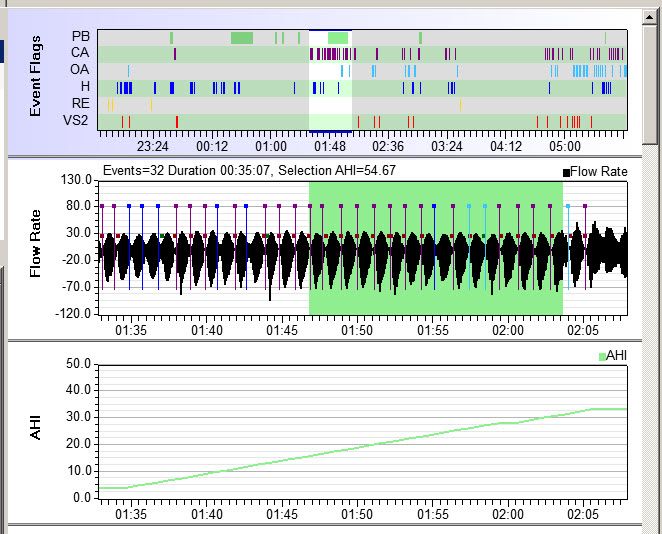
1) With the history of Afib and the data you have posted, your doc's concern about emergent CA is a valid concern. And the RTs who have been seeing you and telling you "that my CPAP (software) results are good (with an occasional muffed day or two-per-month)" are NOT understanding the data if they're looking the Encore equivalent of the Sleepy Head data you've posted.
2) You need to listen to your doctor and work with him to figure out
- whether you really have emergent sleep apnea---i.e. take the sleep test the doc has recommended and trust him when he tells you his impression about what the results indicate; and
- accept a presription of an ASV machine if your sleep doc does indeed diagnose you with some form of central sleep apnea or complex sleep apnea or emergent sleep apnea.
I really believe that if I had let myself sleep another 3 hours this afternoon that the chart would’ve continued to reflect the fairly benign results the 2-hour nap did (whether they’re really benign or not). To put it differently, I really believe that the results I’m getting in the evenings (not all evenings, but more than I’d like) might not reflect my true condition.
This is something that you ought to discuss with your sleep doc. Nap sleeping (even long naps) is not quite the same as night sleeping. We don't get into as much Stage 3 sleep and we don't tend to have as long of REM cycles.
What I would like to see addressed by the medical practitioners I’m seeing are the OBVIOUS issues surrounding the breathing problems I experience: the nasal passages closing down due to phantom(?) congestion; the rapid mouth-outtake of breath I feel I need to make to somehow equalize my breathing pressure; the raw state of my nasal interior. Correct me if I’m wrong, but I don’t think any of these factors are directly connected with sleep apnea. (You don’t read in the literature: “If you have a stuffy nose you might have sleep apnea.”) (A friend suggested it might be due to the high pollen count, for example. I’ve never had asthma problems…)
The congestion may or may not be connected to less than optimized humidifier settings on your PAP machine. You can (and should) play around with the humidifier settings. Since you are currently using very low humidifier settings, it may be worth turning the humidifier up some. Too little humidification leads to congestion too. A heated hose that can be set to a fixed temp, like 72 degrees might let you get more humidity while not adding too much heat.
But in my humble opinion,
the "rapid mouth-outtake of breath [you] feel [you] need to make to somehow equalize [your] breathing pressure" may very well be connected to some of the breathing problems that your doc is describing as emergent central apnea. What you are describing is NOT normal breathing with a PAP. And that may be one way your unstable breathing is manifesting itself. It sounds to me like your difficulties on exhaling through your nose have nothing to do with the nasal congestion but have a lot to do with a sensation of not being able to fully exhale against the pressure. And not being able to exhale fully against the pressure MAY be leading to the CO2 levels starting to fluctuate enough to trigger the problems with central apnea and periodic breathing that are clearly present in the data you've shown us.
You need to report the
rapid mouth-outtake of breath breathing pattern to your pulmonologist. If you cannot fully exhale comfortably against 5-8 cm of pressure, then switching from an APAP with A-Flex to a genuine bi-level machine of some sort with both an IPAP and EPAP pressure may significantly increase your comfort and fix the
rapid mouth-outtake of breath breathing pattern by making it much, much easier for you to fully exhale against your EPAP pressure.
I’m worried that the actions of the “specialists” (the pulmonologist, the cardiologist) might be guided so much by their specialty that they can't or choose not to focus first on these much more mundane issues. And I don't quite know how to have these issues expedited and addressed...FIRST.
Right now the data that you've posted clearly demonstrates that your current APAP settings are NOT doing much of anything to treat your sleep apnea problems. Fixing the "mundane" stuff is NOT going to change the fact that there's something seriously amiss with the current APAP settings. And so even if the mundane stuff was all magically made better, you'd still be feeling pretty lousy if the central apneas continue to be a problem beause your doc is correct and you have central apnea of some sort.
Fixing the ineffective pressure settings may very well require you to switch machines. But if a genuinely effective set of settings for a BiPAP, BiPAP ST, or BiPAP ASV can be found, it may actually then become
easier to fix the mundane stuff. Once the settings are optimized to where it is possible for you to get some high quality sleep
at night, you may find that it will be easier to breathe with the (probably new) machine, and that may (all by itself) fix the
rapid mouth-outtake of breath breathing problems. Once exhaling with the machine does not require you to do the exhalation puffs, it may be easier to figure out a better setting on the humdifier to help with the congestion problem.
To draw a very crude analogy: It's like you've got a serious laceration on your hand that needs medical attention NOW, but you are focusing on the discomfort of having hangnails on your fingers, and you're hoping that alleviating the hangnails will fix the laceration.