Dr. Krakow's book
- rested gal
- Posts: 12881
- Joined: Thu Sep 09, 2004 10:14 pm
- Location: Tennessee
fehler, when I look at my reports in either Encore Pro I click "Full Details" (in Encore Pro) as the type of report I want to see. Not Summary or Trend. EncoreViewer automatically brings up a Full Details report.
I never bother to look at the first three pages of the Full Details report in either Encore Pro or EncoreViwer. I go straight to the Daily Details graphs that start on page 4.
If you'll put screenshots of several of the "Daily Details" graphs (starting on page 4 of your report) up on PhotoBucket, that would be helpful. Those would be the pages with graphs that look like these... "Daily Details":
viewtopic/t27360/encore-pro-lessons.html
I never bother to look at the first three pages of the Full Details report in either Encore Pro or EncoreViwer. I go straight to the Daily Details graphs that start on page 4.
If you'll put screenshots of several of the "Daily Details" graphs (starting on page 4 of your report) up on PhotoBucket, that would be helpful. Those would be the pages with graphs that look like these... "Daily Details":
viewtopic/t27360/encore-pro-lessons.html
ResMed S9 VPAP Auto (ASV)
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Ok Rested Gal i have uploaded my daily data to Photobucket, like i said i am new to all this and i thank you for your sugestion
Ok I finally received my card reader today and down loaded my data. It looks really good to me but I still wake up several times a night mostly to go to the bathroom. Can someone tell me how my data looks and any suggestions you have. Here is the URL I don’t know if I am doing this right or not so let me know.
http://s267.photobucket.com/albums/ii311/fehler/
Ok I finally received my card reader today and down loaded my data. It looks really good to me but I still wake up several times a night mostly to go to the bathroom. Can someone tell me how my data looks and any suggestions you have. Here is the URL I don’t know if I am doing this right or not so let me know.
http://s267.photobucket.com/albums/ii311/fehler/
Pressure set at 12.
- rested gal
- Posts: 12881
- Joined: Thu Sep 09, 2004 10:14 pm
- Location: Tennessee
fehler, your Daily Details reports look very good. Looks like treatment is going quite well for you! The leak rate is a bit jagged, but staying down nicely enough.
You're getting good cpap treatment, imho.
You're getting good cpap treatment, imho.
ResMed S9 VPAP Auto (ASV)
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
-
BarryKrakowMD
- Posts: 65
- Joined: Wed Dec 05, 2007 12:48 am
- Contact:
Chasing the Numbers
If I'm following this thread, the assumption made is that if the numbers look right, then the patient must be obtaining a good response to PAP therapy. In medicine, we call this, "chasing the numbers," and it often proves erroneous.
In cases like these (and I start this way to be clear that I cannot advise this patient on his particular care plan), the real issues are why does nocturia persist and why can he only sleep 3 consecutive hours?
The answer in most cases is that the data presented is missing something of consequence. The most likely thing missed, given that AHI was low and leak was only sporadically high, is that the optimal pressure has not been identified to adequately titrate out all the flow limitations (aka UARS).
If this point were proven valid, then we would say that the patient continues to have nocturia because his SDB continues to drive the right atrium of the heart to produce more atrial natriuretic peptide, which in turn drives the kidneys to make more urine. We would also say that some of these untreated UARS events are causing arousals that lead to a full awakening after 3 hours of sleep.
As a sleep doc, I presume that I have missed something in these types of cases, because the patient isn't anywhere close to an optimal response, unless some other factors can obviously explain nocturia and short sleep periods. Finally, these are the types of cases that have led me to retain a high degree of skepticism about data downloads when the patient's clinical response doesn't match the supposedly stellar objective response.
Rest Wishes.
In cases like these (and I start this way to be clear that I cannot advise this patient on his particular care plan), the real issues are why does nocturia persist and why can he only sleep 3 consecutive hours?
The answer in most cases is that the data presented is missing something of consequence. The most likely thing missed, given that AHI was low and leak was only sporadically high, is that the optimal pressure has not been identified to adequately titrate out all the flow limitations (aka UARS).
If this point were proven valid, then we would say that the patient continues to have nocturia because his SDB continues to drive the right atrium of the heart to produce more atrial natriuretic peptide, which in turn drives the kidneys to make more urine. We would also say that some of these untreated UARS events are causing arousals that lead to a full awakening after 3 hours of sleep.
As a sleep doc, I presume that I have missed something in these types of cases, because the patient isn't anywhere close to an optimal response, unless some other factors can obviously explain nocturia and short sleep periods. Finally, these are the types of cases that have led me to retain a high degree of skepticism about data downloads when the patient's clinical response doesn't match the supposedly stellar objective response.
Rest Wishes.
_________________
| Humidifier: HC150 Heated Humidifier With Hose, 2 Chambers and Stand |
| Additional Comments: Puritan Bennett Breeze Nasal Pillows; ResMed Mirage Quattro FFM; Respironics Premium Chinstrap; Breath Right Nasal Strips |
Barry Krakow, MD
Blogging at Fast Asleep (Sign up: https://fastasleep.substack.com/embed
Books & Videos at http://www.barrykrakowmd.com
Practice at http://www.barrykrakowmd.com
Blogging at Fast Asleep (Sign up: https://fastasleep.substack.com/embed
Books & Videos at http://www.barrykrakowmd.com
Practice at http://www.barrykrakowmd.com
Dr. Krakow,
In some ways i agree with you but considering i have been on CPAP for only 3 week, could it be that i still am not completely comfortable with CPAP theripy. i am still a newby but if i am wrong would a person with this problem need to raise his pressure or what do you think he should do,
Frank
In some ways i agree with you but considering i have been on CPAP for only 3 week, could it be that i still am not completely comfortable with CPAP theripy. i am still a newby but if i am wrong would a person with this problem need to raise his pressure or what do you think he should do,
Frank
Pressure set at 12.
-
BarryKrakowMD
- Posts: 65
- Joined: Wed Dec 05, 2007 12:48 am
- Contact:
Changing Pressures
It is very reasonable to wait through a period of acclimation, but it is equally important to not misinterpret a response as being better than it really is. SDB patients need to be clear on what their symptoms are and contrast those symptoms with a specific set of goals.
If you visit the bathroom twice per night, the goal in most cases is to reduce these visits to "zero," unless another factor (e.g prostate, lithium medication, prior surgery, etc.) indicates zero as an improbable goal. Our sense is that greater than 75% of SDB patients eliminate nocturia, so if one doesn't meet that goal in say the first month or two, we would want that patient to retain sufficient motivation to optimize their care.
Optimizing care could mean a new titration, switching to bilevel, working to reduce mask leak, overcoming mouth breathing, setting proper humidification, managing nasal hygiene, treating leg jerks and/or just learning how to gain comfort with PAP therapy.
The key is to be clear about what a good response is likely to mean for you, then stay focused on achieving that response.
If you visit the bathroom twice per night, the goal in most cases is to reduce these visits to "zero," unless another factor (e.g prostate, lithium medication, prior surgery, etc.) indicates zero as an improbable goal. Our sense is that greater than 75% of SDB patients eliminate nocturia, so if one doesn't meet that goal in say the first month or two, we would want that patient to retain sufficient motivation to optimize their care.
Optimizing care could mean a new titration, switching to bilevel, working to reduce mask leak, overcoming mouth breathing, setting proper humidification, managing nasal hygiene, treating leg jerks and/or just learning how to gain comfort with PAP therapy.
The key is to be clear about what a good response is likely to mean for you, then stay focused on achieving that response.
_________________
| Humidifier: HC150 Heated Humidifier With Hose, 2 Chambers and Stand |
| Additional Comments: Puritan Bennett Breeze Nasal Pillows; ResMed Mirage Quattro FFM; Respironics Premium Chinstrap; Breath Right Nasal Strips |
Barry Krakow, MD
Blogging at Fast Asleep (Sign up: https://fastasleep.substack.com/embed
Books & Videos at http://www.barrykrakowmd.com
Practice at http://www.barrykrakowmd.com
Blogging at Fast Asleep (Sign up: https://fastasleep.substack.com/embed
Books & Videos at http://www.barrykrakowmd.com
Practice at http://www.barrykrakowmd.com
- rested gal
- Posts: 12881
- Joined: Thu Sep 09, 2004 10:14 pm
- Location: Tennessee
Frank, I'm not a doctor, but I think you're absolutely right. I do believe that for many people, getting used to this crazy new way of trying to sleep -- especially getting used to trying to sleep with a mask on -- is responsible for many people's "wakeups", even if cpap treatment is doing its part of the job fine.fehler wrote:Dr. Krakow,
In some ways i agree with you but considering i have been on CPAP for only 3 week, could it be that i still am not completely comfortable with CPAP theripy.
"New" is relative to each person. One person might get quite acclimated and comfortable with cpap treatment immediately. Another person might take months (if ever) to get completely used to it, even if they've been titrated perfectly in the sleep lab and their sleep disordered breathing is being treated perfectly right from the get-go.
I think most of the problems people have with "sleeping" well with cpap treatment -- even if their pressure is right, they're not having any trouble breathing with the way their machine delivers the pressure, and are not having excessive leaks -- goes back again, again, and again to the MASK.
Let's face it (no pun intended! lol ) Wearing a mask, even one the person finds relatively comfortable, is not as conducive to uninterrupted sleep for many people as not having to wear a mask at all.
For one thing, most masks do not allow a person to sleep with their head on their pillow exactly as they used to. The person may even have changed their sleep position quite a bit, trying to keep the mask from bumping the pillow or mattress.
I'd say it's possible that sometimes just the "feeling" of a mask that's gotten a bit dislodged, or straps digging in, or hose tugging as you turn over... any of those things might jog the brain awake from lighter stages of sleep...especially in someone who was still fairly new to "cpap."
Even the increased sound of the exhaust vent at times when the exhaust gets too close to bedcovers or pillow could wake up a light sleeper.
I'm aware of at least a couple of awakenings during the night, every night. I could very well have more that are so brief I'm not aware of them. Fortunately, I'm able to simply turn over and go right back to sleep from the awakenings I am aware of, and I wake up every morning feeling very well rested.
However, if a person in their early days and weeks of cpap treatment wakes up during the night, for any reason, I can well imagine that some people find it more difficult to "just turn over and go back to sleep." They may start notice the mask is uncomfortable, the machine is noisy. Might start thinking about their "breathing" or start rearranging pillows, straps, hose, etc....staying awake longer until they have even more difficulty going back to sleep.
With the way your data looks -- quite good, imho -- I personally would not be worrying about whether your titration was right. I'd be looking for other reasons why you're waking up, and why you feel an urge to go to the bathroom when you do wake during the night.
This is not what would be one of the first things that would come to my mind, but I'm not a doctor:
My bet is that your optimal pressure probably has already been identified and is adequately titrating out flow limitations for you. Of course, without another PSG (easier said than done!) there's no way to see everything that's going on with your breathing.The most likely thing missed, given that AHI was low and leak was only sporadically high, is that the optimal pressure has not been identified to adequately titrate out all the flow limitations (aka UARS).
However, things I'd consider much more likely to be causing your wakeups are other health problems (prostate checked recently?) or sleep hygiene issues including working on ways to make mask and hose management as comfortable and undisturbing as possible.
I don't think a person can even start counting, "I've been using cpap treatment for ___ days, weeks, months" until the person has worked out every sleep hygiene issue that might be interfering with sleep or with effective treatment.
Only when everything conducive to a good sleep environment has been taken care of, and possible other health issues and possible med side effects are considered, should a person even start counting "how long" they've been using cpap. Especially if the data from the machine looks as good as yours does, Frank.
If your mask is comfortable for you to sleep in, and if you're pretty comfortable in general with your "cpap" treatment, a health issue (besides the obvious...getting prostate checked) that you might want to take a closer look at -- very common in people with OSA -- is GERD. Untreated or undertreated acid reflux disease. Can even be "Silent GERD" without the usual recognized "acid reflux" symptoms.
GERD might account for some of your wakeups, but not necessarily for your need to visit the bathroom.
Good luck on sleeping longer and longer at a time!
ResMed S9 VPAP Auto (ASV)
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
How Many Is Many?
It is unclear to me exactly how many times you actually end up urinating. How many is it?fehler wrote:It looks really good to me but I still wake up several times a night mostly to go to the bathroom. Can someone tell me how my data looks and any suggestions you have.
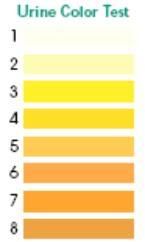
How much do you go (get out the big Pyrex measuring cup)(you'll know which one to use after the first time you do this). Report in milliliters.
How about the color?
SAG

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
fehler wrote:Ok Rested Gal i have uploaded my daily data to Photobucket, like i said i am new to all this and i thank you for your sugestion
Ok I finally received my card reader today and down loaded my data. It looks really good to me but I still wake up several times a night mostly to go to the bathroom. Can someone tell me how my data looks and any suggestions you have. Here is the URL I don’t know if I am doing this right or not so let me know.
http://s267.photobucket.com/albums/ii311/fehler/
Frank,
Your data looks good to me, too. I think it's only logical to want to see what's going on during the night. At least you now have some data reports to use as comparisons as you progress through your therapy.
You mentioned trying to give up smoking.....do you have high blood pressure or diabetes? Do you drink a lot of fluids during the evening before bedtime? Any of those could countribute to your nightly bathroom trips. I think it also takes more time to get one's body used to this new way of sleeping/breathing.
Hang in there. It'll get better.
Den
(5) REMstar Autos w/C-Flex & (6) REMstar Pro 2 CPAPs w/C-Flex - Pressure Setting = 14 cm.
"Passover" Humidification - ResMed Ultra Mirage FF - Encore Pro w/Card Reader & MyEncore software - Chiroflow pillow
User since 05/14/05
"Passover" Humidification - ResMed Ultra Mirage FF - Encore Pro w/Card Reader & MyEncore software - Chiroflow pillow
User since 05/14/05
I'm on the third read of the book. First was a speed read-then an in depth read-now a read and practice the techniques/exercises. I can't agree with the person who said your techniques were simple. At least for me it is taking a fair amount of practice. I've found out some things about myself that surprised me. And really applying the "techniques" has ramifications beyond the sleep issue. And yes I am sleeping better.
Faced with the choice between changing one's mind and proving that there is no need to do so, almost everyone gets busy on the proof.....Galbraith's Law
-
BarryKrakowMD
- Posts: 65
- Joined: Wed Dec 05, 2007 12:48 am
- Contact:
Responses
I think a lot of the points Rested Gal has offered are quite useful in her last post, but I would disagre with or modify a few items in the following ways:
1. Early Retitration. There is a notion among some people that the first titration you get has a strong potential for providing definitive pressures. I don't think there is any scientific basis to that claim. Given all the variables we are talking about as well as the difficulty adapting to this foreign physiological process, the odds are actually against finding the best pressure the first time. This has been described in a variety of papers showing or implying how far off the first titration was in many cases. Also, where I trained at Stanford, the original model was to repeat the titration 1 month after the first to enable a fine-tuning process. Some insurance carriers have attempted to dissuade this process from occurring, but that has been financially driven.
2. Interpretation of Findings.There's no way for any of us to know what a data download really means, and there is no way for us to know whether an original titration was reliable or not. To reiterate, the algorithms dealing with flow limitation (UARS) on these machines have not reached the state of "rocket science." They may point us in useful directions, but there is no way to look at them and declare, "your data looks good, so you don't need another titration." And, if we don't know the type of lab where the original titration was conducted, the titration style of the sleep tech and supervising physician, the scoring technique of the lab, the aggressiveness in titrating out flow limitation, the amount of consolidated REM generated, and the stability of the oxygen baseline (irrespective of desaturations), then we cannot formulate any specific theories on the accuracy of the first titration.
3. Masks vs Pressures. This is a critical topic, and although I agree with many of the points made, there is a basic flaw in the presentation, because the assumption is made that all these mask variables can emerge in isolation unrelated to pressure settings. For some people, it really is the mask, and focusing on fixing it is the right emphasis. But we must never forget the following: If you have the wrong pressures, you are going to suffer from lighter sleep or outright awakenings because the pressure did not properly resolve SDB events. In either case, lighter sleep or awakenings, your attention is clearly going to be directed at the mask if you wake up, because there's little else for it to shine on. You are not going to wake up after 1, 2, or 3 hours and say, "oh, I just had another one of those darn UARS events." But you might say, "this mask feels funny, painful, weird, annoying, and embarrassing."
THE LIGHTER YOU SLEEP DUE TO INVALID PRESSURES will lead just about anyone to eventually have restless or disturbed sleep that eventually leads to awakenings, which in turn may inappropriately rush you to the judgment that it was the mask causing the whole problem.
Yes, it can be chicken and egg here, but never lose sight of the fact that many (not all) mask issues are also interconnected with the wrong pressure settings.
4. Timing is Everything The big issue on retitration is timing, because the longer a person waits for the retitration, the more they may develop sufficient negativity or poor habits with respect to using PAP therapy. These negative perspectives reduce the initial high prospects for a good adaptation. For our center, we often can rely on a single question, asked the morning after the first titration: "Did you sleep better, the same, or worse with PAP Therapy?" When an SDB patient reports sleeping better the very first night of treatment, there's a much greater likelihood that we are not only closer to definitive pressures, but also, the patient has already swept through much of the adaptation process on that very first night. We often bring back these patients for retitrations in 2 to 3 months. If however the patient reports no improvement in sleep quality the first night, then we encourage them to return for the retitration in 1 month.
5. Long-Term Followup. The long-term followup plan for SDB patients is clearly evolving towards a "chronic disease state management" approach, which simply means "more is better." The more here is more followup with providers to fine tune equipment and other sleep related issues and more time spent in the lab to fine tune pressures and equipment. Many facilities are already starting to recommend yearly titrations for the majority of their patients, and these "tune ups" will result in adjustments that enhance sleep quality and outcomes.
6. Book Followup. I've never heard or noticed a comment about the techniques in Sound Sleep being simple. I've heard that the writing style and the format of the book laid out the techniques in ways that were very easy to understand. Techniques such as "mental imagery," and "emotional processing" are two methods that intuitively are quite simple to appreciate, but I concur fully that they take time to learn to apply skillfully and to incorporate into your daily regimen.
Rest Wishes
1. Early Retitration. There is a notion among some people that the first titration you get has a strong potential for providing definitive pressures. I don't think there is any scientific basis to that claim. Given all the variables we are talking about as well as the difficulty adapting to this foreign physiological process, the odds are actually against finding the best pressure the first time. This has been described in a variety of papers showing or implying how far off the first titration was in many cases. Also, where I trained at Stanford, the original model was to repeat the titration 1 month after the first to enable a fine-tuning process. Some insurance carriers have attempted to dissuade this process from occurring, but that has been financially driven.
2. Interpretation of Findings.There's no way for any of us to know what a data download really means, and there is no way for us to know whether an original titration was reliable or not. To reiterate, the algorithms dealing with flow limitation (UARS) on these machines have not reached the state of "rocket science." They may point us in useful directions, but there is no way to look at them and declare, "your data looks good, so you don't need another titration." And, if we don't know the type of lab where the original titration was conducted, the titration style of the sleep tech and supervising physician, the scoring technique of the lab, the aggressiveness in titrating out flow limitation, the amount of consolidated REM generated, and the stability of the oxygen baseline (irrespective of desaturations), then we cannot formulate any specific theories on the accuracy of the first titration.
3. Masks vs Pressures. This is a critical topic, and although I agree with many of the points made, there is a basic flaw in the presentation, because the assumption is made that all these mask variables can emerge in isolation unrelated to pressure settings. For some people, it really is the mask, and focusing on fixing it is the right emphasis. But we must never forget the following: If you have the wrong pressures, you are going to suffer from lighter sleep or outright awakenings because the pressure did not properly resolve SDB events. In either case, lighter sleep or awakenings, your attention is clearly going to be directed at the mask if you wake up, because there's little else for it to shine on. You are not going to wake up after 1, 2, or 3 hours and say, "oh, I just had another one of those darn UARS events." But you might say, "this mask feels funny, painful, weird, annoying, and embarrassing."
THE LIGHTER YOU SLEEP DUE TO INVALID PRESSURES will lead just about anyone to eventually have restless or disturbed sleep that eventually leads to awakenings, which in turn may inappropriately rush you to the judgment that it was the mask causing the whole problem.
Yes, it can be chicken and egg here, but never lose sight of the fact that many (not all) mask issues are also interconnected with the wrong pressure settings.
4. Timing is Everything The big issue on retitration is timing, because the longer a person waits for the retitration, the more they may develop sufficient negativity or poor habits with respect to using PAP therapy. These negative perspectives reduce the initial high prospects for a good adaptation. For our center, we often can rely on a single question, asked the morning after the first titration: "Did you sleep better, the same, or worse with PAP Therapy?" When an SDB patient reports sleeping better the very first night of treatment, there's a much greater likelihood that we are not only closer to definitive pressures, but also, the patient has already swept through much of the adaptation process on that very first night. We often bring back these patients for retitrations in 2 to 3 months. If however the patient reports no improvement in sleep quality the first night, then we encourage them to return for the retitration in 1 month.
5. Long-Term Followup. The long-term followup plan for SDB patients is clearly evolving towards a "chronic disease state management" approach, which simply means "more is better." The more here is more followup with providers to fine tune equipment and other sleep related issues and more time spent in the lab to fine tune pressures and equipment. Many facilities are already starting to recommend yearly titrations for the majority of their patients, and these "tune ups" will result in adjustments that enhance sleep quality and outcomes.
6. Book Followup. I've never heard or noticed a comment about the techniques in Sound Sleep being simple. I've heard that the writing style and the format of the book laid out the techniques in ways that were very easy to understand. Techniques such as "mental imagery," and "emotional processing" are two methods that intuitively are quite simple to appreciate, but I concur fully that they take time to learn to apply skillfully and to incorporate into your daily regimen.
Rest Wishes
_________________
| Humidifier: HC150 Heated Humidifier With Hose, 2 Chambers and Stand |
| Additional Comments: Puritan Bennett Breeze Nasal Pillows; ResMed Mirage Quattro FFM; Respironics Premium Chinstrap; Breath Right Nasal Strips |
Barry Krakow, MD
Blogging at Fast Asleep (Sign up: https://fastasleep.substack.com/embed
Books & Videos at http://www.barrykrakowmd.com
Practice at http://www.barrykrakowmd.com
Blogging at Fast Asleep (Sign up: https://fastasleep.substack.com/embed
Books & Videos at http://www.barrykrakowmd.com
Practice at http://www.barrykrakowmd.com
What a wonderful list of reasons for making the case to have a data-capable Auto-titrating XPAP machine and the software to interpret the data!
Den
Den
(5) REMstar Autos w/C-Flex & (6) REMstar Pro 2 CPAPs w/C-Flex - Pressure Setting = 14 cm.
"Passover" Humidification - ResMed Ultra Mirage FF - Encore Pro w/Card Reader & MyEncore software - Chiroflow pillow
User since 05/14/05
"Passover" Humidification - ResMed Ultra Mirage FF - Encore Pro w/Card Reader & MyEncore software - Chiroflow pillow
User since 05/14/05











