I’ve been struggling with EDS for much of my adult life, but over the last year the levels of sleepiness and cognitive fuzziness have got to the point where I’ve been barely functional at work. I was told there is around a six month wait list for an OSA test in our public health system, but found out that there are also private sleep clinics nearby. Last week I paid for a home test using a Philips Alice PDx system, and was told I might have to wait another ten days to have the results, and so am on standby for that.
I’m a 51 year old male, 6’2”/220lbs (this is too heavy for my frame) with asthma that is well controlled (might use my inhaler once every couple of months). I’ve never smoked but frequently have 1-2 glasses of wine with dinner. When in my 20s, I volunteered as a control subject in a research study that included an overnight sleep test followed by a daytime multiple sleep-latency test. There was no mention of sleep apnea, but the researcher who scored the tests later noted that my MSLT was indicative of narcolepsy. Because it was a research study, there was no followup (at the time, I didn’t really realize my EDS wasn’t normal). My doctor at the time prescribed stimulant medication for the EDS, which I have used intermittently over the last 30 years.
I had a back injury in 2013 and gained some weight due to reduced activity, which coincided with a dramatic increase in snoring that led me to being banished to the sofa for a couple of months. The snoring has been an ongoing issue for my long-suffering wife, and I’ve been sleeping on the sofa again for the last eight months or so. She has described the snoring as a combination of weird breathing, clicking, and wheezing. However, she has been adamant that I don't stop breathing and has kind of dismissed the apnea testing as a waste of time and money.
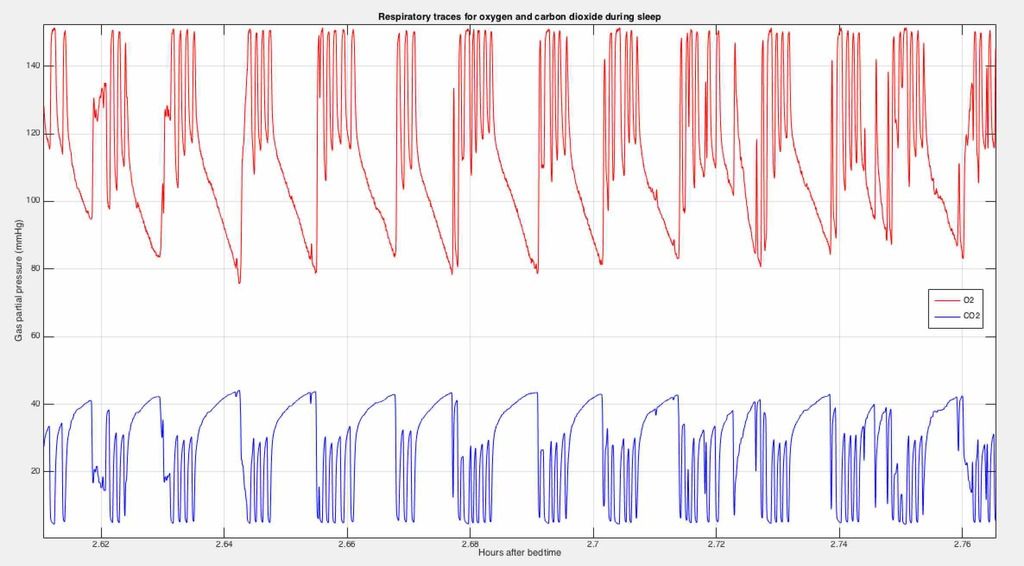
In an odd twist of fate, I actually work as a health science researcher in an area that involves a certain degree of respiratory physiology (I have a working knowledge but am not an expert, nor am I a physician). It happens that my group is building a system to record expired O2 and CO2 levels for a specific research application, so as part of the testing I decided to bring the prototype home and rig up a test circuit I could wear while sleeping (we do these measurements routinely in our work, although not usually during sleep). The traces I got last night are attached to this post - one image shows about ten minutes of recording and the other zooms in to show around a minute of data. I do not know much about sleep apnea, and while I wait for my ‘real’ doctor’s diagnosis (upon which any actual treatment will be based) I’d be interested in any comments on the signals I recorded.
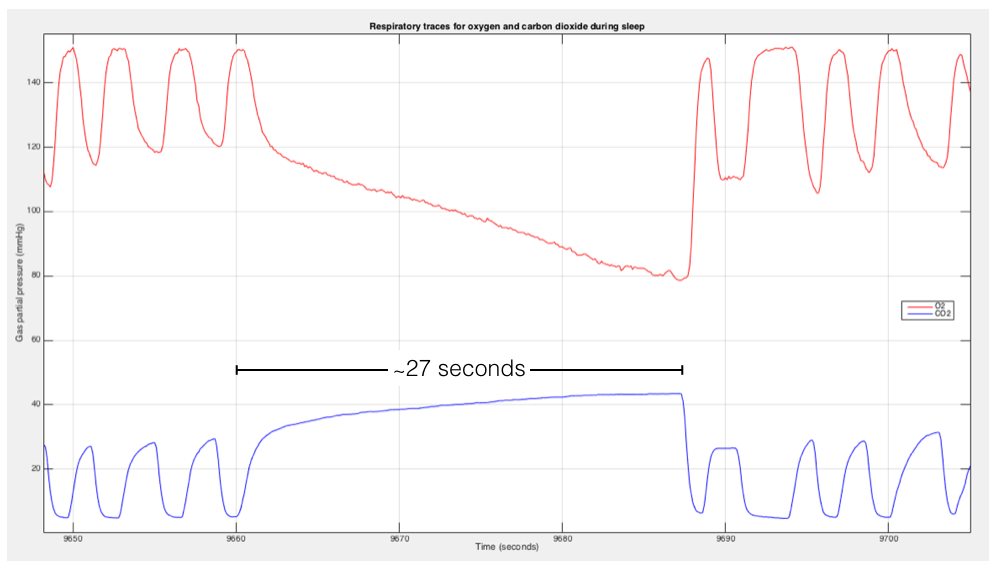
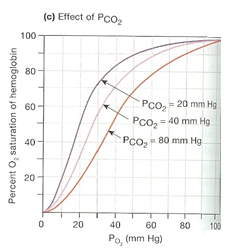
The red trace is the instantaneous concentration of O2 flowing past a sampling port in a well-sealed face mask (there is an aperture to allow air in and out with negligible resistance; the sampling port takes air that is flowing through this at all times). The peaks represent inhaled room air, and the valleys represent the exhaled air from which some of the O2 has been absorbed in the lung. The blue trace shows the corresponding waveform for CO2 - in this case the peaks represent the exhaled CO2 (unloaded from the blood in the lung) and the valleys reflect the near-zero levels of CO2 in the atmosphere. In both cases, the 'end expiratory' values are considered a surrogate for the concentration of O2 and CO2 in the arterial blood exiting the lung.
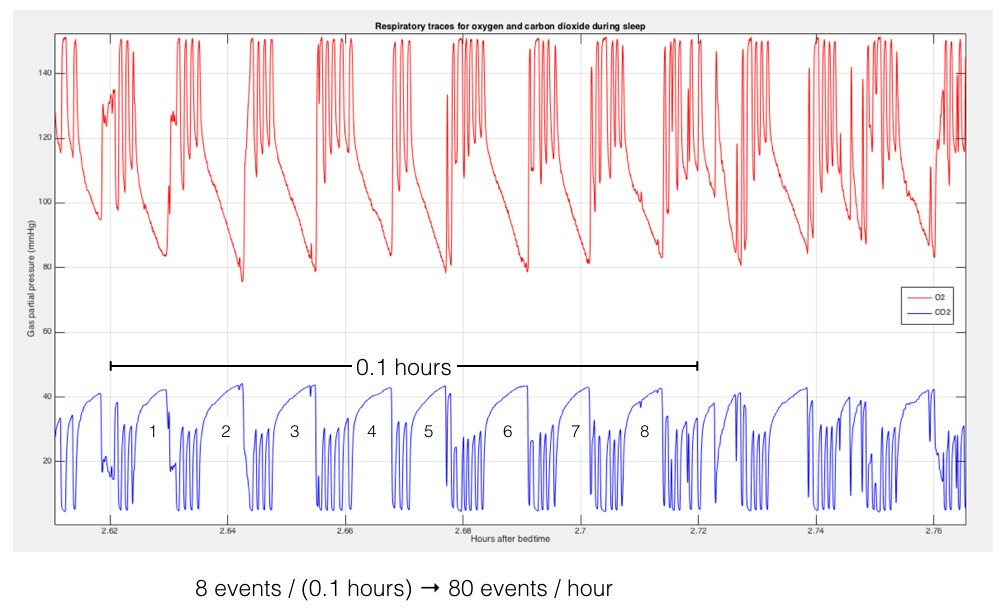
I included segments that appear to show regular interruptions of breathing that happened in clusters lasting around an hour. During these clusters, the repetitive rate works out to around 80 ‘events’ per hour (which seems very high). However, these events happen in clusters and there are some periods of what appear to be more ’normal’ breathing (it would probably not be 80 events/hour averaged over the whole night). In the second image, the continued reduction in O2 level and buildup of CO2 are clearly visible during the period of apnea, which really gives the appearance of a very prolonged exhalation. The sampling port continually sucks a small amount of air (it’s driven by a noisy pump and I had to keep the analyzer outside of the basement room where I sleep), and the samples probably represent a mix of air pulled out of the mouth/throat/trachea and room air pulled in from outside (so the O2 depletion and CO2 buildup may actually be worse than depicted due to mixing with room air during apnea).
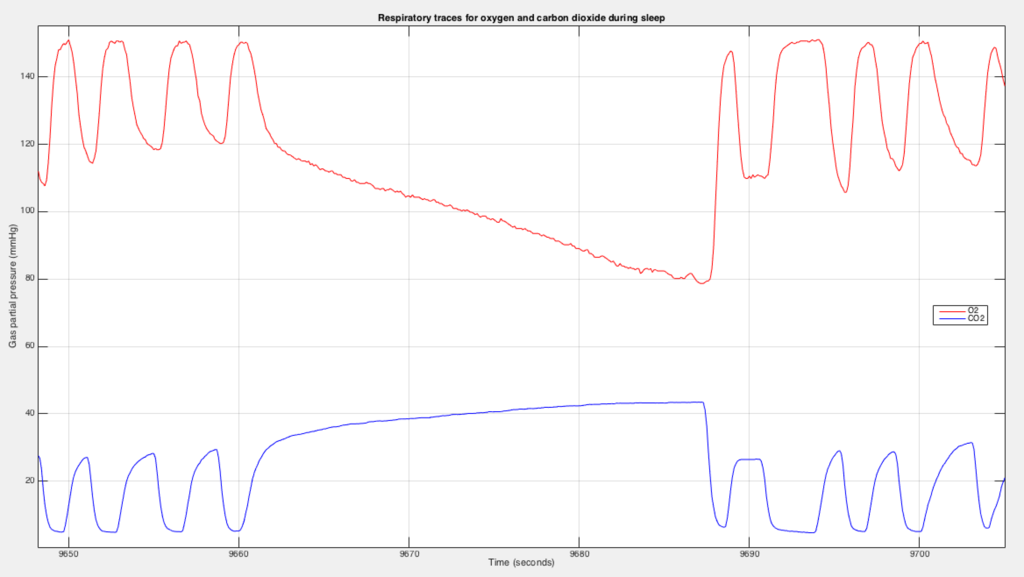
I was thus wondering: are the diagnostic criteria for AHI based on the total number of events in the whole night divided by the total hours of sleep, or the rate of events observed over shorter periods such as the clusters I’ve noted? Do the traces displayed here look like apneas? I have felt absolutely wretched on waking for many months, completely unrested and often with a headache and burning ache in my legs. I also seem to have at best around two hours per day when I’m really functional to any degree, the rest being spent in a kind of brain fog and just trying to stay awake. I had a doctor before just up the dosage of the Concerta I was taking, but I’ve realized that if I really have OSA then no amount of drugs will make up for the lack of quality sleep.
I will finish by stressing that I am going to base all treatment decisions on the advice of my physician. However, I am interested in both physiology and my health and would like to learn more as I wait for the official test result.
Thanks for reading this *long* first post! I am hoping that CPAP therapy will help manage this.