Hi from new member (tried taping my mask)
- DreamStalker
- Posts: 7509
- Joined: Mon Aug 07, 2006 9:58 am
- Location: Nowhere & Everywhere At Once
Re: Hi from new member (waiting for test results)
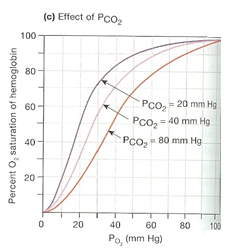
Well with your CO2 hanging out around 40 mm Hg, your O2 is still well above 90% ... which is not that bad. When your O2 gets below 90%, then there is something to start worrying about.
My O2 min was measured just below 60% on my sleep study so that's why after 25+ years of untreated OSA I'm brain damaged crazy I guess.
Again, I'm beginning to think that your events are more of restricted air flow rather than all out apnea ... but the results of a professional sleep study should tell you for sure.
My O2 min was measured just below 60% on my sleep study so that's why after 25+ years of untreated OSA I'm brain damaged crazy I guess.
Again, I'm beginning to think that your events are more of restricted air flow rather than all out apnea ... but the results of a professional sleep study should tell you for sure.
President-pretender, J. Biden, said "the DNC has built the largest voter fraud organization in US history". Too bad they didn’t build the smartest voter fraud organization and got caught.
Re: Hi from new member (waiting for test results)
Thanks - the only thing my plots really show is that there is no inhalation during around 25 seconds - it basically looks like a very long sigh. The actual numbers might not be reliable during such an event, since sampling depends on exhalation of sufficient force to displace all room air, and they likely underestimate the severity of blood gas changes (possibly by a large margin). I'm curious what the professional study will show...DreamStalker wrote:Well with your CO2 hanging out around 40 mm Hg, your O2 is still well above 90% ... which is not that bad. When your O2 gets below 90%, then there is something to start worrying about.
My O2 min was measured just below 60% on my sleep study so that's why after 25+ years of untreated OSA I'm brain damaged crazy I guess.
Again, I'm beginning to think that your events are more of restricted air flow rather than all out apnea ... but the results of a professional sleep study should tell you for sure.
_________________
| Machine: DreamStation Auto CPAP Machine |
| Mask: AirFit™ F10 Full Face Mask with Headgear |
| Humidifier: DreamStation Heated Humidifier |
- DreamStalker
- Posts: 7509
- Joined: Mon Aug 07, 2006 9:58 am
- Location: Nowhere & Everywhere At Once
Re: Hi from new member (waiting for test results)
Yes. That and you have those 25-second sighs recurring regularly every 45 seconds for a period of at least 8 minutes ... which I find to be weird (no offense ).leptic wrote:Thanks - the only thing my plots really show is that there is no inhalation during around 25 seconds - it basically looks like a very long sigh. The actual numbers might not be reliable during such an event, since sampling depends on exhalation of sufficient force to displace all room air, and they likely underestimate the severity of blood gas changes (possibly by a large margin). I'm curious what the professional study will show...DreamStalker wrote:Well with your CO2 hanging out around 40 mm Hg, your O2 is still well above 90% ... which is not that bad. When your O2 gets below 90%, then there is something to start worrying about.
My O2 min was measured just below 60% on my sleep study so that's why after 25+ years of untreated OSA I'm brain damaged crazy I guess.
Again, I'm beginning to think that your events are more of restricted air flow rather than all out apnea ... but the results of a professional sleep study should tell you for sure.
President-pretender, J. Biden, said "the DNC has built the largest voter fraud organization in US history". Too bad they didn’t build the smartest voter fraud organization and got caught.
- DreamStalker
- Posts: 7509
- Joined: Mon Aug 07, 2006 9:58 am
- Location: Nowhere & Everywhere At Once
Re: Hi from new member (waiting for test results)
One last thing leptic. I can't help but think that if your weird sleep sigh rhythms do have a neurologic or leptic source, that perhaps ketosis therapy may be somewhat of a solution for your EDS condition. You seem to have the background to take control of your condition and that is a good thing IMO.
http://madcapnarcolepsy.com/
http://sleepingresources.com/the-narcolepsy-diet/
http://www.ncbi.nlm.nih.gov/pubmed/15210901
http://madcapnarcolepsy.com/
http://sleepingresources.com/the-narcolepsy-diet/
http://www.ncbi.nlm.nih.gov/pubmed/15210901
President-pretender, J. Biden, said "the DNC has built the largest voter fraud organization in US history". Too bad they didn’t build the smartest voter fraud organization and got caught.
Re: Hi from new member (waiting for test results)
Thanks - you know it's funny, I work in neuroscience and there is an increasing body of research on the possible benefits of ketone metabolism. I will check it out in more detail.DreamStalker wrote:One last thing leptic. I can't help but think that if your weird sleep sigh rhythms do have a neurologic or leptic source, that perhaps ketosis therapy may be somewhat of a solution for your EDS condition. You seem to have the background to take control of your condition and that is a good thing IMO.
_________________
| Machine: DreamStation Auto CPAP Machine |
| Mask: AirFit™ F10 Full Face Mask with Headgear |
| Humidifier: DreamStation Heated Humidifier |
- DreamStalker
- Posts: 7509
- Joined: Mon Aug 07, 2006 9:58 am
- Location: Nowhere & Everywhere At Once
Re: Hi from new member (waiting for test results)
Indeed there is cutting edge research in metabolic therapy of neurologic disorders ... check out what Dominic D'Agostino and Richard Veech are up to and I think you will be surprised.leptic wrote:Thanks - you know it's funny, I work in neuroscience and there is an increasing body of research on the possible benefits of ketone metabolism. I will check it out in more detail.DreamStalker wrote:One last thing leptic. I can't help but think that if your weird sleep sigh rhythms do have a neurologic or leptic source, that perhaps ketosis therapy may be somewhat of a solution for your EDS condition. You seem to have the background to take control of your condition and that is a good thing IMO.
President-pretender, J. Biden, said "the DNC has built the largest voter fraud organization in US history". Too bad they didn’t build the smartest voter fraud organization and got caught.
Re: Hi from new member (waiting for test results)
Thanks for all the replies - I did the exhaled gas monitoring again last night and saw the same pattern of periodic clusters of regular apneas, with otherwise normal breathing.
I will open a new thread asking specifically about clustering of apneas like this. I'm still waiting for my doctor's test results (they downloaded the data last Friday).
I will open a new thread asking specifically about clustering of apneas like this. I'm still waiting for my doctor's test results (they downloaded the data last Friday).
_________________
| Machine: DreamStation Auto CPAP Machine |
| Mask: AirFit™ F10 Full Face Mask with Headgear |
| Humidifier: DreamStation Heated Humidifier |
Finally got (preliminary) test result
Sleep clinic called - said the test indicated moderate sleep apnea. Will see the doctor tomorrow morning.
_________________
| Machine: DreamStation Auto CPAP Machine |
| Mask: AirFit™ F10 Full Face Mask with Headgear |
| Humidifier: DreamStation Heated Humidifier |
Re: Hi from new member (waiting for test results)
Looking back on this, the desaturations did turn out to be in the upper 80% range, which seems in line with the textbook curve given the PO2 around 80mmHg.leptic wrote:
Here’s a curve that accounts for different CO2 levels, although I’d be careful to take this too literally as the real affinity depends on temperature and other variables. My CO2 looks like it only goes above 40, but that's also likely an underestimate because end-tidal values during an apnea are not really reliable.
I find it interesting that a reduced O2 sat of 80% is considered 'moderate' for sleep apnea - when we monitor O2 sat for research procedures, any decrease below mid-90's is considered very significant and cause for alarm. The O2 sat is normally very tightly regulated in healthy people, but I don't have much experience with cardiorespiratory disease so maybe this is why our rules are so conservative. We've done this on hundreds of healthy people, including very elderly individuals, and the resting O2 sat is always well into the 90's.
Disclaimer: I'm a researcher in a multi-disciplinary team and *not* a physician or healthcare professional.
_________________
| Machine: DreamStation Auto CPAP Machine |
| Mask: AirFit™ F10 Full Face Mask with Headgear |
| Humidifier: DreamStation Heated Humidifier |
Re: Hi from new member (waiting for test results)
The severity classifications for sleep apnea are based on average number of apnea events per hour of total sleep time and not the oxygen saturation levels.
There's really no standard factoring in of the oxygen levels which of course could be remarkable or not and may or may not give a full picture of what is going on. I have a friend whose AHI was mid 60s and her Oxygen levels never dropped below 94%.
My AHI in non rem sleep was only 12...in REM it was low 50s.
BUT in non rem sleep those 12 per hour must have been nasty long because my O2 was in the low 70s.
Length of event isn't factored in either.
Maybe at some time in the future O2 levels and event duration will have some standard guidelines but for now there aren't any.
https://en.wikipedia.org/wiki/Apnea%E2% ... pnea_index
There's really no standard factoring in of the oxygen levels which of course could be remarkable or not and may or may not give a full picture of what is going on. I have a friend whose AHI was mid 60s and her Oxygen levels never dropped below 94%.
My AHI in non rem sleep was only 12...in REM it was low 50s.
BUT in non rem sleep those 12 per hour must have been nasty long because my O2 was in the low 70s.
Length of event isn't factored in either.
Maybe at some time in the future O2 levels and event duration will have some standard guidelines but for now there aren't any.
https://en.wikipedia.org/wiki/Apnea%E2% ... pnea_index
The AHI is calculated by dividing the number of apnea events by the number of hours of sleep. The AHI values are categorized as:[1][2]
Normal: 0-4
Mild sleep apnea: 5-14
Moderate sleep apnea: 15-29
Severe sleep apnea: 30 or more
_________________
| Machine: AirCurve™ 10 VAuto BiLevel Machine with HumidAir™ Heated Humidifier |
| Additional Comments: Mask Bleep Eclipse https://bleepsleep.com/the-eclipse/ |
I may have to RISE but I refuse to SHINE.
Re: Hi from new member (waiting for test results)
Sorry you are right - the way I wrote the post was confusing. I realize that the apnea classification is based on the AHI, which is based purely on the number of events per unit time.Pugsy wrote:The severity classifications for sleep apnea are based on average number of apnea events per hour of total sleep time and not the oxygen saturation levels.
I have also seen, independently of this, a grading scheme for O2 sat severity - for example this summary.
I was surprised that O2 sats down to 80% were considered 'moderate' (at least by the clinic above); I guess this just shows how hard apnea is (or can be) hitting a person's body.
_________________
| Machine: DreamStation Auto CPAP Machine |
| Mask: AirFit™ F10 Full Face Mask with Headgear |
| Humidifier: DreamStation Heated Humidifier |
Re: Hi from new member (waiting for test results)
Here in the US oxygen levels of 88% or lower for a certain period of the night (I forget exact amount of time but it isn't all that long) will satisfy most insurance requirements for a person to have supplemental O2 at night and that's without sleep apnea being involved at all. Some how or other someone doesn't think that 87% is all that "moderate" or else insurance wouldn't be paying for adding O2.
Anyway, it's like anything else when it comes to medicine...we have to have some lines in the sand to start with and then we add in "clinical correlation is needed" when the lines start to get fuzzy.
I did have my overnight oxygen levels tested once I had my cpap therapy optimized just to make sure since mine went so low but I didn't really think that there was a problem because the killer headaches went away pretty much immediately. Killer headaches being a symptoms of the low O2 and high CO2O which often goes along with OSA.
As a population we seem to need or want numerical standards to "classify" anything and tend to rely on just the numbers as the standard and forget that often we have to add in the other stuff....like event duration or O2 levels.. My 12 per hour in non REM sleep may not seem like much if just looking at that number but they were lasting long enough to cause severe desats and I wasn't even getting much REM because every time I would hit REM things got much worse and I would wake up only to have to start the sleep cycle process all over again.
Sure made me wonder at the time what would have happened if I had events that long and had REM that lasted 30 minutes.
Personally...classifications don't mean all that much to me one way or the other. All I know is the killer headaches are gone and the getting up to pee every hour on the hour is gone and those results alone I consider a huge improvement. My husband says I no longer snore to rattle the windows so he sleeps better and in general I feel better.
It's sort of like being pregnant...you either are or aren't....need cpap therapy or you don't. Some one with "mild" needs therapy just as much as someone with "severe".
Anyway, it's like anything else when it comes to medicine...we have to have some lines in the sand to start with and then we add in "clinical correlation is needed" when the lines start to get fuzzy.
I did have my overnight oxygen levels tested once I had my cpap therapy optimized just to make sure since mine went so low but I didn't really think that there was a problem because the killer headaches went away pretty much immediately. Killer headaches being a symptoms of the low O2 and high CO2O which often goes along with OSA.
As a population we seem to need or want numerical standards to "classify" anything and tend to rely on just the numbers as the standard and forget that often we have to add in the other stuff....like event duration or O2 levels.. My 12 per hour in non REM sleep may not seem like much if just looking at that number but they were lasting long enough to cause severe desats and I wasn't even getting much REM because every time I would hit REM things got much worse and I would wake up only to have to start the sleep cycle process all over again.
Sure made me wonder at the time what would have happened if I had events that long and had REM that lasted 30 minutes.
Personally...classifications don't mean all that much to me one way or the other. All I know is the killer headaches are gone and the getting up to pee every hour on the hour is gone and those results alone I consider a huge improvement. My husband says I no longer snore to rattle the windows so he sleeps better and in general I feel better.
It's sort of like being pregnant...you either are or aren't....need cpap therapy or you don't. Some one with "mild" needs therapy just as much as someone with "severe".
_________________
| Machine: AirCurve™ 10 VAuto BiLevel Machine with HumidAir™ Heated Humidifier |
| Additional Comments: Mask Bleep Eclipse https://bleepsleep.com/the-eclipse/ |
I may have to RISE but I refuse to SHINE.
Re: Hi from new member (waiting for test results)
Thanks Pugsy (and happy belated birthday, by the way!)
Agree that somewhat arbitrary numerical criteria are a fact of life in medicine. I suppose common sense and the big picture help a lot.
Glad to hear your headaches are better - in some of the stuff we do at my job, we manipulate CO2 because it dilates blood vessels throughout the brain (and this is of interest for various research topics - it's all approved by hospital ethics boards and we have doctors and RTs involved). The headache you get is because the CO2 actually increases intracranial pressure - it has nothing to do with the O2. Another illustration of this is when a neurosurgeon wants to reduce herniation of the brain through a craniotomy, he or she will ask the anesthesiologist to ventilate the person a bit faster so their CO2 goes down (the opposite of apnea). The effect is quite visible - you can actually see how higher levels of CO2 leads to the brain being forced out of the skull, and reducing the levels immediately fixes it.
Low O2, independent of CO2 levels, is really dangerous because so long as you can blow off CO2 you feel great as you gradually go into a nice (endless) sleep. Old MRI systems used to use nitrogen as part of the magnet cooling, and you'd occasionally hear about service techs being asphyxiated during N2 fills due to (an undetectable) buildup in the room displacing all O2. Your lungs will happily unload CO2 into pure N2, but the hypoxia (which you can't feel) will still kill you.
Sorry for the lecture - I'm really interested in this stuff and it doesn't take much to get me going...
Agree that somewhat arbitrary numerical criteria are a fact of life in medicine. I suppose common sense and the big picture help a lot.
Glad to hear your headaches are better - in some of the stuff we do at my job, we manipulate CO2 because it dilates blood vessels throughout the brain (and this is of interest for various research topics - it's all approved by hospital ethics boards and we have doctors and RTs involved). The headache you get is because the CO2 actually increases intracranial pressure - it has nothing to do with the O2. Another illustration of this is when a neurosurgeon wants to reduce herniation of the brain through a craniotomy, he or she will ask the anesthesiologist to ventilate the person a bit faster so their CO2 goes down (the opposite of apnea). The effect is quite visible - you can actually see how higher levels of CO2 leads to the brain being forced out of the skull, and reducing the levels immediately fixes it.
Low O2, independent of CO2 levels, is really dangerous because so long as you can blow off CO2 you feel great as you gradually go into a nice (endless) sleep. Old MRI systems used to use nitrogen as part of the magnet cooling, and you'd occasionally hear about service techs being asphyxiated during N2 fills due to (an undetectable) buildup in the room displacing all O2. Your lungs will happily unload CO2 into pure N2, but the hypoxia (which you can't feel) will still kill you.
Sorry for the lecture - I'm really interested in this stuff and it doesn't take much to get me going...
_________________
| Machine: DreamStation Auto CPAP Machine |
| Mask: AirFit™ F10 Full Face Mask with Headgear |
| Humidifier: DreamStation Heated Humidifier |
Got actual numbers - about to try first night of cpap
Met with sleep doc this morning and got a printout of the test results from the Alice PDx monitor. Here are some numbers:
Lights off (LOFF): 10:45pm
Lights on: 6:20am
Sleep latency from LOFF: 4 min (confirms what my wife has always said)
Total recording time: 454 min
Sleep period time: 445 min
Total sleep time: 434 min
Number of central apneas: 11 (1.5/hour)
Number of obstructive apneas: 148 (20.4/hour)
Hypopnias: 41 (5.7/hour)
AHI: 27.6 (30.1 supine)
Mean duration of central apneas: 19.1s (max 29s)
Mean duration of obstructive apneas: 30.0s (max 97.5s)
Average O2 saturation: 92%
Total number of desats: 167 (23.1/hour)
Longest desat: 52.5s
Lowest O2 sat: 84%
The cpap machine is a Philips DreamStation CPAP, which seems to be popular here. Mask is an AirFit F10 (full face, at my request, as I am a mouth breather). I am very impressed with the comfort and fit of the mask, and overall industrial design of the DreamStation. I tried the system during a short pseudo-nap before getting my kids and did not have any issues with the airflow or mask comfort. Downloaded the DreamMapper software and SleepyHead and was able to offload data from the SIM card. The system also has a modem that the clinic will apparently monitor.
Sorry if it seems like I'm obsessing about it, or appear to be proud of the numbers. I have been worrying for so long that my fatigue symptoms etc. are 'all in my head' that seeing some of the objective numbers (like O2 sats) is a relief in a strange sort of way. My wife has been saying 'there's no way you have sleep apnea' for over a year; she was kind of mad that I went for the sleep study, saying it was a waste of time and money. Now she's upset about the cpap, saying it's just a lazy solution when I should really be losing weight. I am hoping that increasing my energy level will enable me to exercise more and be a more energetic spouse; I do need to improve my diet (have been really bad about stress eating).
Very interested to see how the night will go and (more importantly) how the next days and weeks feel. Thanks to all for the advice and support.
Lights off (LOFF): 10:45pm
Lights on: 6:20am
Sleep latency from LOFF: 4 min (confirms what my wife has always said)
Total recording time: 454 min
Sleep period time: 445 min
Total sleep time: 434 min
Number of central apneas: 11 (1.5/hour)
Number of obstructive apneas: 148 (20.4/hour)
Hypopnias: 41 (5.7/hour)
AHI: 27.6 (30.1 supine)
Mean duration of central apneas: 19.1s (max 29s)
Mean duration of obstructive apneas: 30.0s (max 97.5s)
Average O2 saturation: 92%
Total number of desats: 167 (23.1/hour)
Longest desat: 52.5s
Lowest O2 sat: 84%
The cpap machine is a Philips DreamStation CPAP, which seems to be popular here. Mask is an AirFit F10 (full face, at my request, as I am a mouth breather). I am very impressed with the comfort and fit of the mask, and overall industrial design of the DreamStation. I tried the system during a short pseudo-nap before getting my kids and did not have any issues with the airflow or mask comfort. Downloaded the DreamMapper software and SleepyHead and was able to offload data from the SIM card. The system also has a modem that the clinic will apparently monitor.
Sorry if it seems like I'm obsessing about it, or appear to be proud of the numbers. I have been worrying for so long that my fatigue symptoms etc. are 'all in my head' that seeing some of the objective numbers (like O2 sats) is a relief in a strange sort of way. My wife has been saying 'there's no way you have sleep apnea' for over a year; she was kind of mad that I went for the sleep study, saying it was a waste of time and money. Now she's upset about the cpap, saying it's just a lazy solution when I should really be losing weight. I am hoping that increasing my energy level will enable me to exercise more and be a more energetic spouse; I do need to improve my diet (have been really bad about stress eating).
Very interested to see how the night will go and (more importantly) how the next days and weeks feel. Thanks to all for the advice and support.
_________________
| Machine: DreamStation Auto CPAP Machine |
| Mask: AirFit™ F10 Full Face Mask with Headgear |
| Humidifier: DreamStation Heated Humidifier |
Re: Hi from new member (waiting for test results)
It would have been interesting to know the approx. times of your centrals, whether they were falling-asleep and awakening ones, or throughout the night and/or clustered. However...
Do tell your wife that apnea is thought to put on weight, not that weight creates apnea. Big difference!
And if her reaction to your having a serious condition is to call you lazy... but that's for you to deal with.
Maybe she needs to do some reading, at the very least, and not listen to water cooler opinions (if that's relevant).
Do tell your wife that apnea is thought to put on weight, not that weight creates apnea. Big difference!
And if her reaction to your having a serious condition is to call you lazy... but that's for you to deal with.
Maybe she needs to do some reading, at the very least, and not listen to water cooler opinions (if that's relevant).