Oh, Dave. Don't worry, no one can flex their epoch like you can.mollete wrote:Great question. Let's get The Kid to weigh in.BrianinTN wrote:Given that I sit around 4-5cm most of the night, and things seem to get worse when we go much above that, is an ASV even going to do much for me?
Hey Kid, you gonna add something here or just stand around and flex for SU?
Post-Surgery Blues: Scoring Question
- SleepingUgly
- Posts: 4690
- Joined: Sat Nov 28, 2009 9:32 pm
Re: Post-Surgery Blues: Scoring Question
_________________
| Mask: Swift™ FX For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Rescan 3.10 |
Never put your fate entirely in the hands of someone who cares less about it than you do. --Sleeping Ugly
Re: Post-Surgery Blues: Scoring Question
I'm feeling very small over here....SleepingUgly wrote: Oh, Dave. Don't worry, no one can flex their epoch like you can.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: minEPAP=4, minPS=2 |
Re: Post-Surgery Blues: Scoring Question
"Flex their epoch"?
I think Pugsy just jumped ahead of you in line.
I think Pugsy just jumped ahead of you in line.
Re: Post-Surgery Blues: Scoring Question
They can fix that, you know...BrianinTN wrote:I'm feeling very small over here....SleepingUgly wrote: Oh, Dave. Don't worry, no one can flex their epoch like you can.
Re: Post-Surgery Blues: Scoring Question
So if you guys can put away all the battery-powered devices for a minute...
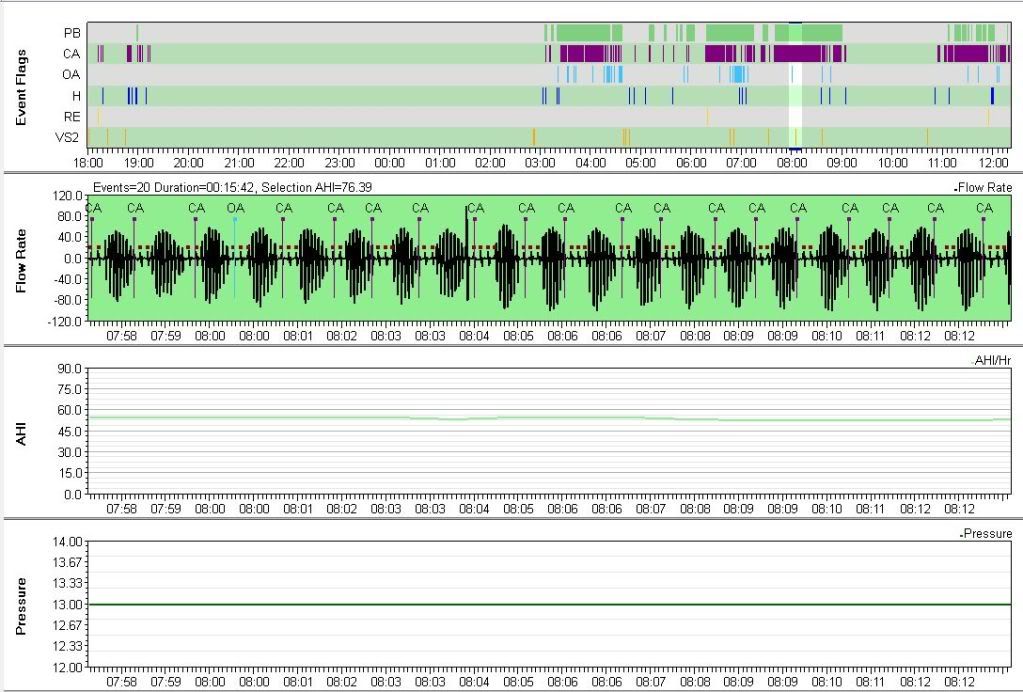
...looking at the morning of 7.26, there's a heap of central-based phenomena. It would appear that the ventilatory instablity was there for a while, so perhaps this current stuff shouldn't be a complete surprise...
...looking at the morning of 7.26, there's a heap of central-based phenomena. It would appear that the ventilatory instablity was there for a while, so perhaps this current stuff shouldn't be a complete surprise...
Re: Post-Surgery Blues: Scoring Question
Er, 7/26? That was pre-surgery. The stuff from this month is the only post-surgery data. (Although that you're seeing all those centrals pre-surgery is perhaps instructive data in and of itself, in that it suggests maybe this won't be self-resolving?)mollete wrote: ...looking at the morning of 7.26, there's a heap of central-based phenomena.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: minEPAP=4, minPS=2 |
Re: Post-Surgery Blues: Scoring Question
Correct, the ventilatory instability was apparently always there, so perhaps your initial concern ("Omigod! My AHI is 66!") may be better understood at this point.BrianinTN wrote:Although that you're seeing all those centrals pre-surgery is perhaps instructive data in and of itself..
I think at this point it's apples and aardvarks. That was on CPAP 8.0 cmH20, and maybe an expected response in that scenario....it suggests maybe this won't be self-resolving?
Right now you have at least 5 sets of data: ambient, CPAP, APAP, ambient post-surgery and post-surgery with APAP, and now we have to add the time factor (which should allow some/all of the ventilatory instability to correct).
Sometimes, doing less is more...
Re: Post-Surgery Blues: Scoring Question
Plus data from my original CPAP setting of 13, BiPAP S/T (at 20/16), and ASV (min EPAP 4). YEAH SCIENCE!mollete wrote: Right now you have at least 5 sets of data: ambient, CPAP, APAP, ambient post-surgery and post-surgery with APAP, and now we have to add the time factor (which should allow some/all of the ventilatory instability to correct).
Yeah, I think of that as the corollary to Occam's razor. However, in this particular case, where I can't get back in to see a Stanford doc for a while (and the lead times for scheduling sleep studies are long), I'm unclear how to best go about "doing less." My options, as I see them, are:mollete wrote: Sometimes, doing less is more...
1) Stop using xPAP therapy for the time being. This certainly has the greatest emotional appeal to me, since I feel far less functional (and much more emotionally stressed) when using xPAP.
2) Continue using APAP within this narrow band of very low pressures.
3) Fire up the non-PR1 ASV that my old awful DME saddled me with to get rid of their old inventory, and allow it to work within similarly narrow bands of pressures, despite the noise being disruptive to my sleep.
I'll phrase my question carefully: if you were a patient, say, who had data sort of similar to mine, and couldn't get in to see anyone for a while, what might you choose? Hypothetically, of course.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: minEPAP=4, minPS=2 |
Re: Post-Surgery Blues: Scoring Question
Hypothetically, I would establish a treatment team. Division of labor would be as previously assigned:BrianinTN wrote:if you were a patient, say, who had data sort of similar to mine, and couldn't get in to see anyone for a while, what might you choose? Hypothetically, of course.
BrianinTN wrote:I'll leave the diagnostic observations to you and the DWing to me.
Re: Post-Surgery Blues: Scoring Question
Sorry to hear about the worrisome results. But for some ENT surgeries, complete recovery, including full remission of any swelling, is not expected until a year. So there may still be improvement to expect. Good luck!BrianinTN wrote: opted for surgery this past summer
_________________
| Mask: Wisp Nasal CPAP Mask with Headgear - Fit Pack |
| Humidifier: DreamStation Heated Humidifier |
PR Dreamstation BiPap ASV, WISP nasal mask with magnets
Re: Post-Surgery Blues: Scoring Question
However, and "IMHO", the application of DWing when CompSAS is underfoot may result in (results) that make it seem as though no progress is being made. If we are going to use the "time heals all" philosophy of CompSAS correction, then the body must see the same set of parameters, all night, every night, for x period of time (and I don't know what x is. Your Stanford guy is talking 3-4 months, the surgery guys reviewed at 6 months, the CompSAS guys seem to talk about 1 month a lot). Sporadic use will not allow equilibration to occur ("Insanity is...").BrianinTN wrote:I'll leave the diagnostic observations to you and the DWing to me.
As an example, if we look back at 2010, where a very aggressive pressure was being used, some terrific runs of PICs were seen:
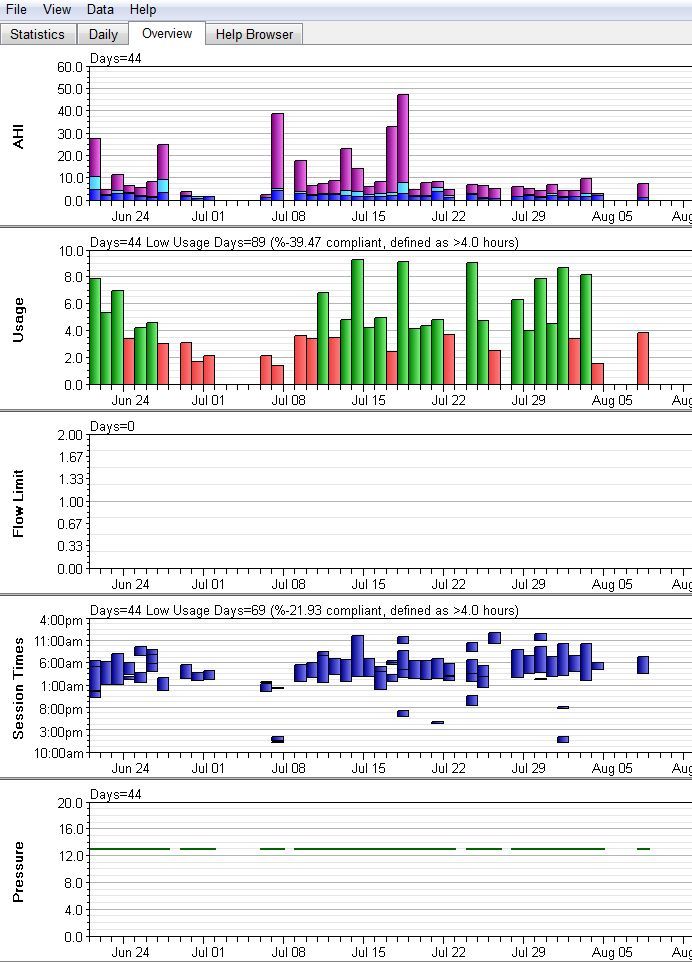
However, if we review patterns of use, there was no real opportunity for equilibration. Only a few days utilization, partial use during some nights, skipping nights:
TS, there are strong suggestions that equilibration would occur with consistent use.
TS2, there are tons of variables that must be considered here (one of the reasons that mollete does not DWing).
Re: Post-Surgery Blues: Scoring Question
I get your point. I know there have been a lot of changes, which given your theory about needing time for things to "settle in" makes any sort of scientific evaluation difficult at best.
Obviously, from the patient perspective, your central conclusion is immensely frustrating because it implies the potential for literally years of experimentation and tweaking, rather than days or weeks or even a couple months. It would also cast doubt, as framed, as to the usefulness of an in-lab titration, yes? If the whole point is that the body needs proper time to acclimate, then a set of data points that are, in effect, random shocks wouldn't be very useful.
As for compliance, I'm not altogether sure what to do about that. When you saw partial nights in the data, it was always me giving it a go and being exasperated by my frequency of cognizantly waking up. I usually tried, if at all possible, to get the requisite minimum 4 hours of xPAP therapy.
On nights where I didn't use it at all, other than the occasional ones where I was traveling and it was infeasible to take my machine, I was generally saying, "Damn it, I feel like a zombie, and I have crucial work tomorrow that just cannot wait, so I HAVE to get at least a reasonable night of sleep tonight." (My Epworth before "treatment" was actually OK; it goes up in flames while on xPAP, especially the higher the pressure.) So given that I can't sit like a bump on a log for years on end, yeah, I dunno. I know a lot of people around here are kind of sissy-ish and give up easily, but I don't think that's the case for me. I have literally hundreds of nights of me trying to make it work (170ish just in this CPAP data, plus the BiPAP and ASV data separately). I just flat-out feel more exhaustion and daytime sleepiness the next day after using xPAP than not, regardless of the pressure settings.
Obviously, from the patient perspective, your central conclusion is immensely frustrating because it implies the potential for literally years of experimentation and tweaking, rather than days or weeks or even a couple months. It would also cast doubt, as framed, as to the usefulness of an in-lab titration, yes? If the whole point is that the body needs proper time to acclimate, then a set of data points that are, in effect, random shocks wouldn't be very useful.
As for compliance, I'm not altogether sure what to do about that. When you saw partial nights in the data, it was always me giving it a go and being exasperated by my frequency of cognizantly waking up. I usually tried, if at all possible, to get the requisite minimum 4 hours of xPAP therapy.
On nights where I didn't use it at all, other than the occasional ones where I was traveling and it was infeasible to take my machine, I was generally saying, "Damn it, I feel like a zombie, and I have crucial work tomorrow that just cannot wait, so I HAVE to get at least a reasonable night of sleep tonight." (My Epworth before "treatment" was actually OK; it goes up in flames while on xPAP, especially the higher the pressure.) So given that I can't sit like a bump on a log for years on end, yeah, I dunno. I know a lot of people around here are kind of sissy-ish and give up easily, but I don't think that's the case for me. I have literally hundreds of nights of me trying to make it work (170ish just in this CPAP data, plus the BiPAP and ASV data separately). I just flat-out feel more exhaustion and daytime sleepiness the next day after using xPAP than not, regardless of the pressure settings.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: minEPAP=4, minPS=2 |
Re: Post-Surgery Blues: Scoring Question
I think you have to treat this whole thing from 2 angles.BrianinTN wrote:Obviously, from the patient perspective, your central conclusion is immensely frustrating because it implies the potential for literally years of experimentation and tweaking, rather than days or weeks or even a couple months. It would also cast doubt, as framed, as to the usefulness of an in-lab titration, yes? If the whole point is that the body needs proper time to acclimate, then a set of data points that are, in effect, random shocks wouldn't be very useful.
First, you need military sleep hygiene. Looking at that history, assuming all the clocks are correct, and poor compliance notwithstanding, if you improved your sleep hygiene by 300% you would only get up to "awful".
Second, it depends on how you want to deal with the CompSAS. Your DLs show the potential for improvement with machine use (there was even some good areas at 13 cmH2O), as shown in graph above (although the stretches are very short). If we are to look your overall use of 166 days:
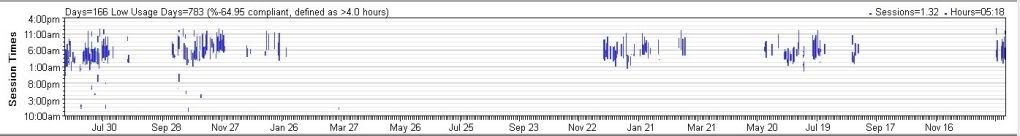
it is clear that the sporadic use would NEVER allow equilibration to occur. You can't use for a couple days, then try it again after a couple weeks to see if things got better.
While surgical and CPAP CompSAS take time, ASV does not. It takes effect in about 15 - 20 minutes (or often less). That's when it's being used appropriately, treating chain centrals (which is what you got).
Re: Post-Surgery Blues: Scoring Question
Yeah, I get you. One qualifier that I'll add is that some of those gaps are periods of time when I was on the BiPAP S/T and the ASV -- but even adding those in, it's still not going to look great. Some of the gaps are me just giving up entirely, saying, "I just can't do this anymore," during especially busy periods in my life...and then later trying to return to it when things are a bit more calm.
EDIT: I amend my previous statement. I pulled up my old ASV data, and it has180 days of treatment logged on its own. Add in the BiPAP S/T time, and in retrospect, I think my compliance efforts are actually pretty decent, all things considered.
I am trying to do better on the hygiene piece, as you saw from my previous post, but I find that to be very hard. Previously, it was the nature of my job (I headed up both US operations and several projects working with teams around the globe for my old company, which meant a lot of wacky hours and deadlines). Right now, it's school, which will end in June but has been stressful and exhausting in its own right and has made any sort of rhythm hard. And, add to all of that the fact that I am a stresser and a worrier, which often makes it impossible for me to settle down at night lest I toss and turn for hours. So, rather than that, I generally try to wait to get into bed until I'm ready to sleep.
Yes, I know. Blah blah blah excuses blah blah blah.
Given your last comment, maybe the thing to do is to pull out the behemoth ASV and see how it copes.
EDIT: I amend my previous statement. I pulled up my old ASV data, and it has180 days of treatment logged on its own. Add in the BiPAP S/T time, and in retrospect, I think my compliance efforts are actually pretty decent, all things considered.
I am trying to do better on the hygiene piece, as you saw from my previous post, but I find that to be very hard. Previously, it was the nature of my job (I headed up both US operations and several projects working with teams around the globe for my old company, which meant a lot of wacky hours and deadlines). Right now, it's school, which will end in June but has been stressful and exhausting in its own right and has made any sort of rhythm hard. And, add to all of that the fact that I am a stresser and a worrier, which often makes it impossible for me to settle down at night lest I toss and turn for hours. So, rather than that, I generally try to wait to get into bed until I'm ready to sleep.
Yes, I know. Blah blah blah excuses blah blah blah.
Given your last comment, maybe the thing to do is to pull out the behemoth ASV and see how it copes.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: minEPAP=4, minPS=2 |
Re: Post-Surgery Blues: Scoring Question
Over 948 days (6/21/2010 - 1/24/2013)? "IMHO", you'd need to double utilization to get to "decent".BrianinTN wrote:EDIT: I amend my previous statement. I pulled up my old ASV data, and it has180 days of treatment logged on its own. Add in the BiPAP S/T time, and in retrospect, I think my compliance efforts are actually pretty decent, all things considered.
In order to expect equilibration to occur, the body must see the same thing every night. Clearly, there is a difference between "utilization" and "consistent utilization".
Looking at the aforementioned time period:

The goal is to paint a solid blue bar in the red box.
Is the ASV file uploadable?