Muffy wrote:split_city wrote:First of all, by start inspiration do you mean start of inspiratory effort or start of inspiratory flow? If you mean start of inspiratory effort, then yes, I agree that it's at the end of the plateau. As I and others have shown, there will be a delay between start inspiratory effort and start inspiratory flow because the individual needs to overcome the positive airway pressure before they can't generate flow i.e. due to iPEEP.
Now I should move my green lines to the left even a little more (and you have to move that red one):
First of all, you put the red line in based on what you believed I thought was start inspiration. I never picked that as start inspiratory effort or inspiratory flow if we are going down that track.
Muffy wrote:so by this criteria, inspiratory start "effort" is now definitely at 20 cmH2O, and that's the end of iPEEP.
If we are going by what others have said:
Steier et al 2009 "Intrinsic positive end-expiratory pressure (PEEPi) as defined by change of oesophageal pressure (DPoes) from end-expiratory
baseline prior to inspiratory flow (vertical dashed line) in the supine posture in a morbidly obese subject." (From figure 1)
Lotti et al 2005 "The difference in esophageal pressure between end-expiration and the initiation of inspiratory flow was considered as an expression of dynamic positive end-expiratory alveolar pressure (PEEPi)."
Figure from Pankow et al

...then yes, the 20cmH20 represents start inspiratory effort. All these studies were conducted during wakefulness under stable breathing conditions. Whether the end of the plateau represents start inspiratory effort when
expiratory drive is high, such is the case in my example, is another question. I assume it would but I'm not positive about it. Which comes to my next point...
Muffy wrote:Carley shows two, not the sustained 20 cmH2O baseline you demonstrated during stable breathing (and I'm calling this stable breathing because those respiratory variations appear to be central (this critical information could have/should have been supported by information from the RIP belts)):
Muffy wrote:and you're trying to compare this to obstruction as noted by Carley. This is apples and aardvarks. Look at the increasing effort during respiratory event in his Pes vs the sustained low effort which then increases during normal respiration in yours.
Hang on, which figure are you having issues with? The one above or this one (which is the one we have been primarily looking at) OR BOTH?
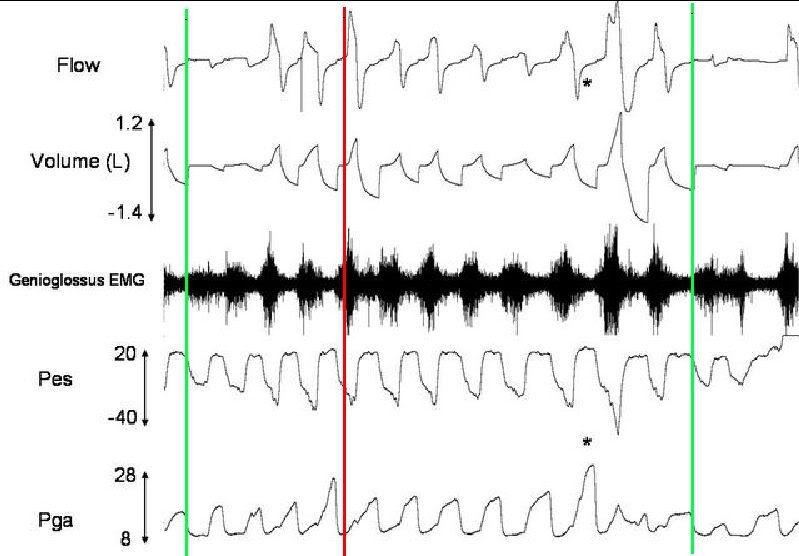
So to first of those two figures. Stable breathing? In what sense? Stable, as in the same what would be happening during wakefulness? Stable, as in not having any respiratory events? He maybe stable to you but it doesn't discount the fact that the individual is demonstrating increased drive. For example, the figure below shows an extended period (~3mins) of the first figure. It's a mixture of stage 2 and 3 sleep (sorry, EEG data was recorded on different computer but I have referred back to the stage data). You classify this as stable breathing? Perhaps, but the patient is certainly demonstrating increased drive (large swings in Pes and Pepi). Inspiratory phasic GG activity is certainly elevated. Upper airway resistance is high. Lots of snoring seen in the mask pressure channel. Importantly, not one EEG arousal was scored during this whole period despite the presence of respiratory events (again, EEG data not recorded on same computer). It has been speculated that arousals are potentially a necessary outcome to dissipate high drive, such is the case during respiratory events. Without arousals, this patient seems to a) overcome respiratory events and b) continues to maintain a high level of drive. But more to the point, call it "stable" breathing if you wish, but don't ignore the fact that they are experiencing high drive. During periods of less drive, end-expiratory Pes was much closer to 10cmH20.

Back to this end-expiratory 20cmH20 Pes. Unfortunately, we had technical difficulties with the gastric balloon catheter in this patient displaying the data above, so I am unable to comment on whether increased
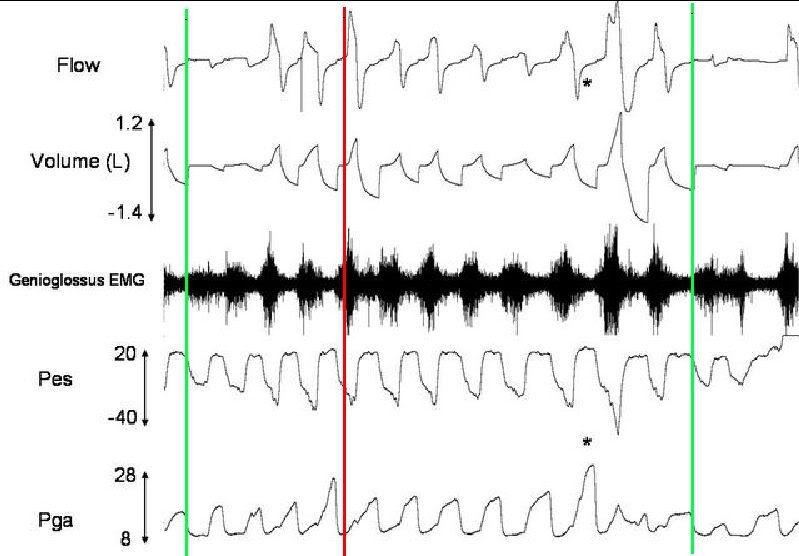
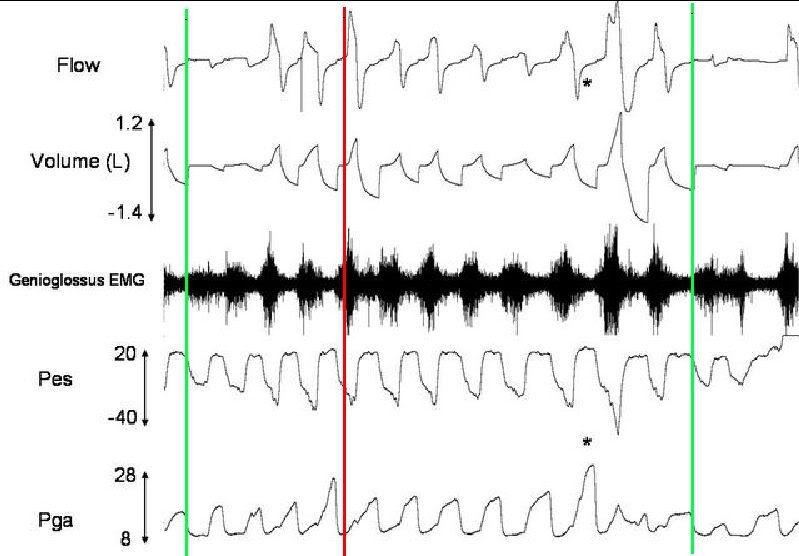
expiratory swings in gastric pressure were occurring at the same time during this period of increased drive. However, back to figure 2 (the one we have mostly been looking at).
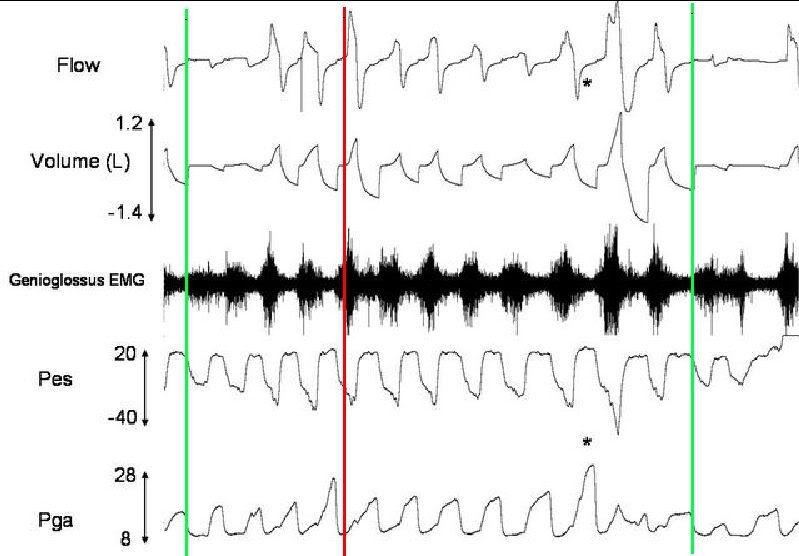
Stable breathing?? Again, maybe but again, high drive state. I mean, just look at those expiratory gastric pressure swings!! I reckon this guy must have a rock hard six-pack under his shirt given the constant abdo crunches he does at night!! He constantly demonstrated these expiratory swings throughout the night. So, in essence, this might be "normal" to him but certainly not normal to most of the other patients I have studied.
Back to a previous point, it appears that this end-expiratory Pes increases as expiratory gastric pressure swings rise (figure below). Are they related? Is the increased abdo crunching contributing to the increased end-expiratory Pes?

It's a bummer that the Carley and co. didn't measure gastric pressure. It would have been interesting to see if the rise in end-expiratory Pes followed similar trends in expiratory gastric pressure swings.
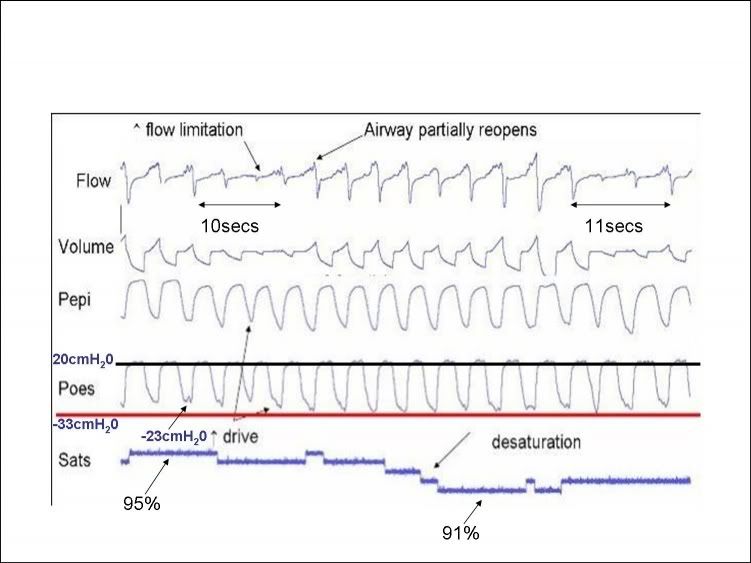
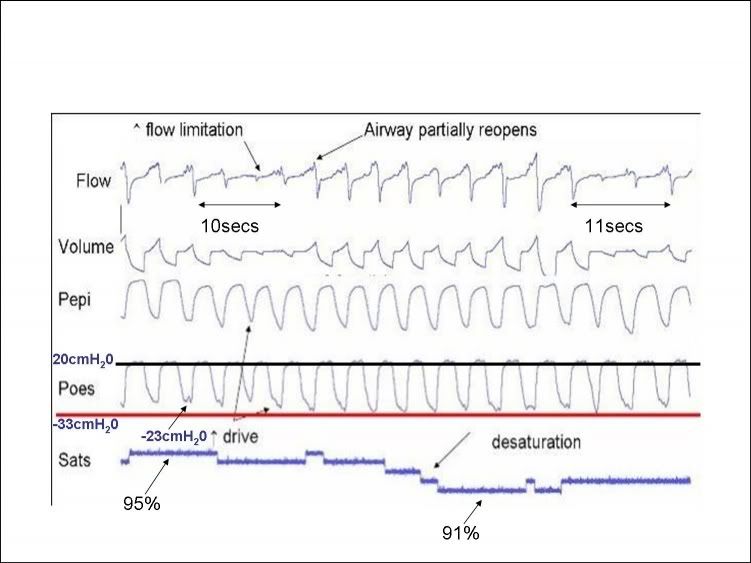
Oh, what the heck. I'll do it for them. From a different patient, similar to Carley and co., end-expiratory Pes is on the rise during an obstruction. BUT, more importantly, look at those increments in expiratory gastric pressure swings towards the end of the event. They look nice. End-expiratory Pes appears to rise in line with increasing expiratory gastric pressure swings. What's more, the peak in expiratory gastric pressure corresponds pretty much to the peak of Pes.

So, in this example, this patient develops expiratory drive during obstruction which coincides with the increase in end-expiratory Pes. Our other 20cmH20 patient appears to have increased expiratory drive even during so called "stable" breathing. So what's to say the maintenance of expiratory gastric pressure swings is contributing to the increased end-expiratory Pes during the period of increase drive? I have already shown that end-expiratory Pes is much less in this patient when he is having normal Pes and Pga pressure swings.
On a side note, it's interesting that this individual (figure above) is able to still achieve some expiratory flow during obstruction without any inspiratory flow i.e. continues to lose lung volume.
Muffy wrote:split_city wrote:But please feel free to write a letter to the editor of Thorax expressing your concerns with the Steier article and perhaps also Journal of Applied Physiology in regards to the Carley paper.
Have their people call my people and I'll see if I can work them in, but you're the one who just bad-mouthed his iPEEP thing, not me.
Oooooh, is he ever gonna be mad.....
Muffy
What you talking about willis? Nope, I didn't bad mouth it at all. I keep referring to it to support my work. You're the one expressing concerns with their data. You follow it up with him. Why not send an email directly to Steier to ask him for his biocals?