You have to be specific as to which "it" you're referring to. WhileBleepingBeauty wrote:Sorry, Muffy dear, but please indulge my sleepy brain here. You said earlier that time should improve things, but now you say it's getting worse. Confusion abounds.
at the beginning of the thread the posterMuffy wrote:simply allowing time for the body to equilibrate may solve a lot of the central problem.
But since you'reStillAnotherGuest wrote:Your overall sleep architecture is awful (way too much wake), which is probably going to have to be dealt with separately-- however, a very important concept related to CompSAS is that sleep instability promotes breathing instability, so working on that aspect should pay good dividends.
that's great, (except the 5-6 hours of sleep time, and I would not be surprised if you still had a few too many awakenings). As long as the lifestyle has changed (which is really how you have to think of it), then things should continue to improve.BleepingBeauty wrote:.. practicing solid sleep hygiene for awhile now. No naps, no matter how much I want one. Yawning all day, but not allowing myself to sleep. To bed at a reasonable hour, and getting up about 5-6 hours later, as usual (unfortunately). I've been walking every other day (briskly, for about 40 minutes, with the dog) and eating better than I ever have in my life (less meat, lots more fish, skinless chicken, lots of veggies, no junk, lots of protein, few carbs)
Weight is determined by a scientific formula. Caloric Expenditure = Basal Metabolic Rate + Thermal Expenditure of Food + Exercise Expenditure. If caloric intake exceeds caloric expenditure, you gain weight. If caloric intake equals caloric expenditure you maintain weight. If caloric intake is less than caloric expenditure, you lose weight. If you burn 500 more calories a day than you take in, you'll lose about a pound a week (a deficit of about 3500 calories a week, which is a good goal).BleepingBeauty wrote:but I'm not losing the weight. IDK what else to do.
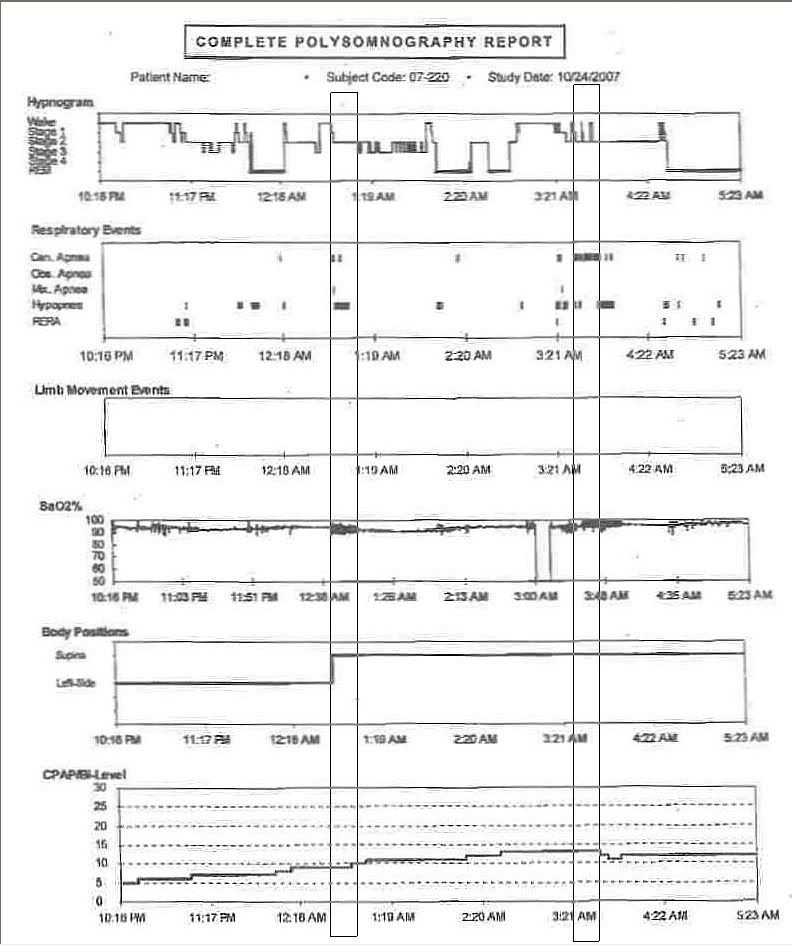
OK, just curious, it's still just an historical document.BleepingBeauty wrote:I can call the lab again on Monday, I guess, to see if there's more from the titration report.
BTW, that first study, as awful as it is, is just an historical document, too. Don't wave that one around to justify ASV because that's not you anymore. Other data suggests that you're not doing too badly:
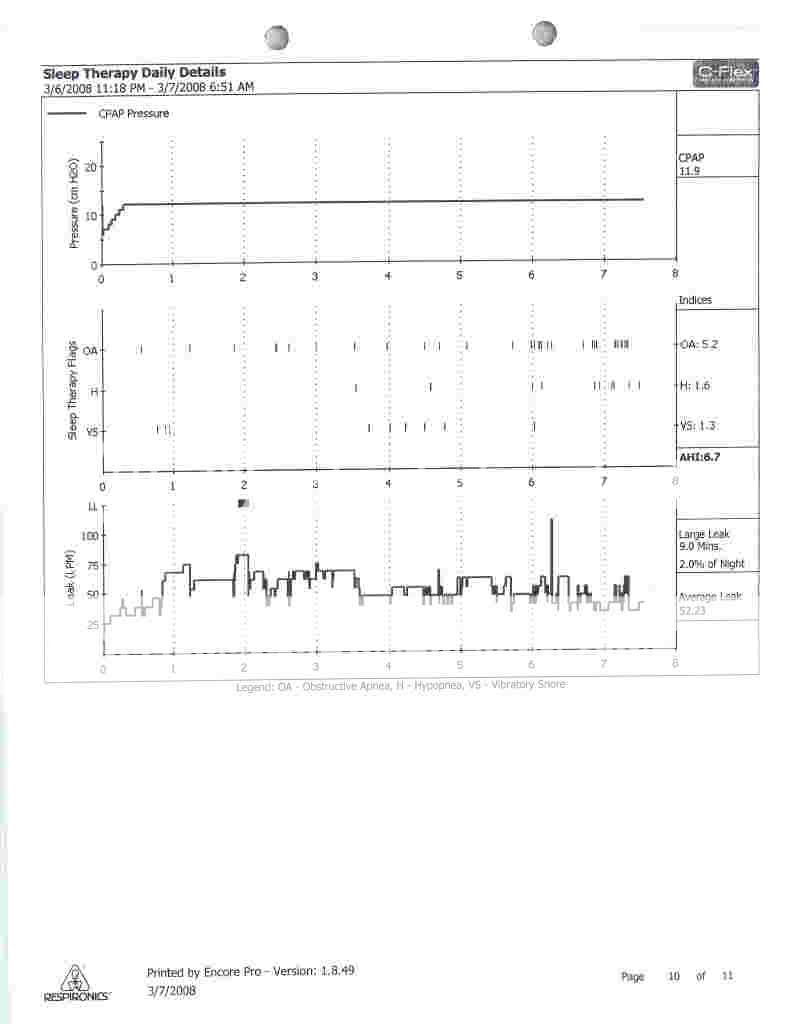
I mean decreasing AHI from 107 to 6.7's not too shabby. If the remaining events are due largely to sleep instability, then ASV may not help all that much. As a tool to stabilize breathing, it takes a little time to "catch", so AHI 0.0 may be an unreachable goal.
That said, if your therapeutic pressure is going to be 14 cmH2O, then moving to an ASV approach, using much lower base pressures and a bilevel attack, could add a significant amount of overall comfort and contribute greatly to improving sleep quality.
I'll have to say, I certainly am curious about your most recent APAP trial. It seems like if it really was "fine", they would have handed it over and said "See, I told you so, now shaddup!" Ask 'em again, nicely, tell 'em then you'll go away, a War of Attrition doesn't do anybody any good. Most CompSAS patients have a tough time AHI-wise, so it's not a Capital Offense to flounder around a bit.
BTW, RG's analysis of the situation up there was "spot on". Either way they're stuck, and they know it. Let them know you know it, too. Nicely.
Don't forget the download.
And you should really try to get a data-capable machine. Have you ever looked into that?
Muffy