And our magnetometer data should be able to show this decrease.StillAnotherGuest wrote: As an aside, this type of patient would now be below FRC.
SAG
Preliminary Data - Current project (exciting!)
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Well, I have to think about SOMETHING While I'm Running.
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
Pleural Musings
Well, then, by definition, intrapulmonary P = 0 at that point.split_city wrote:In simple terms, FRC is the lung volume at which the outward recoil of the chest is equal and opposite to the inward recoil of the lung.
It's neither of those, you just made a pleural space.split_city wrote:To understand why, I simply use an airfilled syringe. Please correct me if I'm wrong as this isn't my area, but I would love to learn. Think of the inside of the syringe as the lungs or esophagus..
Actually that would be IC, but go ahead.split_city wrote:Put your finger on top of the syringe and pull the plunger down and hold the plunger in place. Say this point is analagous to FRC i.e. the inward recoil (syringe/lungs) is balanced by the outward pull on the syringe (hand/chest).
OK, stop right there! That's FRC.split_city wrote:If you let go of the syringe, the syringe would recoil back.
Again, you're measuring the pleural pressure. This is a dynamic system, the lungs per se (and for that matter, Pes) are open to air, so if allowed to equilibrate, P will = 0. Pes inflections only occur when the system is in motion. It returns to baseline when it is static. Or perhaps, the slight elevation noted by the collapse of the surrounding structures which must be subtracted as artifact. The elastic recoil of the lungs pertains to the lung itself.split_city wrote:If you measure the pressure inside the syringe when you held the plunger in place, the value would be negative i.e. what it would be in the lungs at FRC.
That's not pleural pressure.split_city wrote:Yep, I understand that this positive value is an artifact. Unfortunately, we cannot measure pleural pressure.
SAG

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Mixing up Pes with intrapulmonary pressure?
Yes, the system is open to atmosphere. Intrapulmonary pressure = airway pressure = 0 at FRCStillAnotherGuest wrote:Well, then, by definition, intrapulmonary P = 0 at that point.split_city wrote:In simple terms, FRC is the lung volume at which the outward recoil of the chest is equal and opposite to the inward recoil of the lung.
Ok, thanks for clearing that up. It's good to learn new stuff . Now, my understanding is that pleural pressure at FRC is negative because opposite forces acting on it (inwards recoil of lungs and outwards recoil of the chest) acts to pull the lungs from the chest wall. Correct?StillAnotherGuest wrote:It's neither of those, you just made a pleural space.split_city wrote:To understand why, I simply use an airfilled syringe. Please correct me if I'm wrong as this isn't my area, but I would love to learn. Think of the inside of the syringe as the lungs or esophagus..
After all this discussion, are you suggesting that my negative Pes @ FRC readings are incorrect?? Pes is commonly used as a surrogate measure for pleural pressure. Given that pleural pressure is subatmospheric at FRC, Pes will also be negative. Correct? I have seen a number of papers stating that Pes is negative at FRC. Do you think Pes = intrapulmonary pressure?
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
More Minutia...
Intrapleural pressure is normally always negative. When it isn't, the lung turns into a raisin.split_city wrote:Now, my understanding is that pleural pressure at FRC is negative because opposite forces acting on it (inwards recoil of lungs and outwards recoil of the chest) acts to pull the lungs from the chest wall. Correct?
No, the +20 cmH2O seen during exhalation during a period of baseline breathing.split_city wrote:After all this discussion, are you suggesting that my negative Pes @ FRC readings are incorrect??
My point is that that value needs explanation. Either something has caused expiration to go from passive to active (although there's nothing there that would indicate that, like bronchospasm or upper airway obstruction) or the calibration is incorrect.
Is this a trick question? Oh what the hey, I'll go with sure, as long as the patient has no disease that causes loss of compliance.split_city wrote:Pes is commonly used as a surrogate measure for pleural pressure. Given that pleural pressure is subatmospheric at FRC, Pes will also be negative. Correct? I have seen a number of papers stating that Pes is negative at FRC. Do you think Pes = intrapulmonary pressure?
SAG

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
At full expiration and during forced expiration such as the case during a spirometery test, intrapleural pressure becomes positive. This is why we still have air inside the lungs at RV because the postive pleural pressure compresses the airways, trapping air downstream.StillAnotherGuest wrote:Intrapleural pressure is normally always negative. When it isn't, the lung turns into a raisin.split_city wrote:Now, my understanding is that pleural pressure at FRC is negative because opposite forces acting on it (inwards recoil of lungs and outwards recoil of the chest) acts to pull the lungs from the chest wall. Correct?
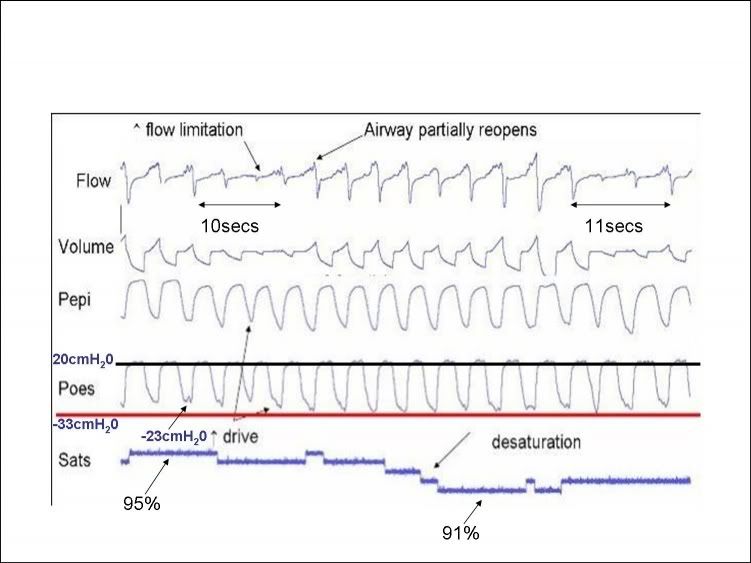
I have already discussed the reasons why peak Pes is increased. You must remember, this +20cmH20 also includes the +5-10cmH20 artifact caused by the compression of the medialstinal structures. The true peak value is likely to be between 10-15cmH20. All the other patients also had increased peak expiratory Pes during their apneas. I'm pretty sure peak Pes also increased during hypopneas in other patients.StillAnotherGuest wrote:No, the +20 cmH2O seen during exhalation during a period of baseline breathing.split_city wrote:After all this discussion, are you suggesting that my negative Pes @ FRC readings are incorrect??
You keep saying baseline breathing. I keep disagreeing with this because the patient is under a high drive state. What would you call his breathing when his airway is patent and there is no flow limitation? Baseline, baseline breathing??
I told you why his expiration has become active. The patient is under a high drive state because his airway is acting as a Starling resistor. I have no doubt he was actively recruiting his abdominal muscles.StillAnotherGuest wrote:
My point is that that value needs explanation. Either something has caused expiration to go from passive to active (although there's nothing there that would indicate that, like bronchospasm or upper airway obstruction) or the calibration is incorrect.
There are no smoke and mirrors. You have clearly stated that you believe that Pes should be zero at FRC.StillAnotherGuest wrote:Is this a trick question? Oh what the hey, I'll go with sure, as long as the patient has no disease that causes loss of compliance.split_city wrote:Pes is commonly used as a surrogate measure for pleural pressure. Given that pleural pressure is subatmospheric at FRC, Pes will also be negative. Correct? I have seen a number of papers stating that Pes is negative at FRC. Do you think Pes = intrapulmonary pressure?
StillAnotherGuest wrote:so baseline Pes is normally 0 cmH2O
What the hey, I'll provide some references to show you that Pes is negative at FRC, thus confirming that Pes does not equal intrapulmonary pressure.StillAnotherGuest wrote:(and for that matter, Pes) are open to air, so if allowed to equilibrate, P will = 0
I have said that Pes can be used as an alternative measure for pleural pressure.
Here is a study comparing pleural pressure with Pes in humans
Mead et al (1959) Journal of Applied Physiology 14(1): 81-83
Upright
Mean pleural pressure at end-expiration was -5.1cmH20
Mean esophageal pressure at end-expiration was -4.8cmH20
Supine
Mean pleural pressure at end-expiration was -1.1cmH20
Mean esophageal pressure at end-expiration was +2.6cmH20
They did not mention the BMI of the subjects
Other studies which have shown Pes to be negative at end-expiration include:
Mead et al (1963) Journal of Applied Physiology 18(2): 295-296
Ferris et al (1959) Journal of Applied Physiology 14(4): 521-524
Coulam and Wood (1971) Journal of Applied Physiology 31(2): 277-287
Gillespie et al (1973) Journal of Applied Physiology 35(5): 709-713 showed that Pes correlated well with pleural pressure in the anesthetized dog.
I hope this clears it up for you.
Going back to the first point. Now remember, it has been shown that Pes is considered a relatively good alternative measurement of pleural pressure (in the upright posture anyway), Mead et al (1955), Knowles et al (1959) and Milic-Emili et al (1964) all showed that Pes was positive at RV
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
Keep It Real
As noted:split_city wrote:At full expiration and during forced expiration such as the case during a spirometery test, intrapleural pressure becomes positive. This is why we still have air inside the lungs at RV because the postive pleural pressure compresses the airways, trapping air downstream.
And those manuevers are not considered "normal".SAG wrote:Intrapleural pressure is normally...
OK, but you're kinda going back and forth here, quoting a bunch of references documenting negative Pes and then adding in mediastinal pressure artifact when the numbers don't fit. Do a wake supine end-expiratory Pes at the begining of the study and then you can properly account for artifact.split_city wrote:I have already discussed the reasons why peak Pes is increased. You must remember, this +20cmH20 also includes the +5-10cmH20 artifact caused by the compression of the medialstinal structures. The true peak value is likely to be between 10-15cmH20.
SAG is confused. Do you mean increased negative or positive peak expiratory Pes? If it occurs during their apneas then how can you have positive Pes? If there's a brief period of increased positive activity post event, then that should be dismissed as normal artifact.split_city wrote:All the other patients also had increased peak expiratory Pes during their apneas. I'm pretty sure peak Pes also increased during hypopneas in other patients.
And again, the Starling principle only applies during inhalation. The only way you could invoke Starling during exhalation would be if there were another factor applied to expiration, like reactive airways or obstructed airway.split_city wrote:The patient is under a high drive state because his airway is acting as a Starling resistor.
During that whole period, independent of the surrounding events? I do.split_city wrote: I have no doubt he was actively recruiting his abdominal muscles.
Very impressive, but for the most part, "upright" is not applicable in the sleep laboratory.split_city wrote:Here is a study comparing pleural pressure with Pes in humans
Mead et al (1959) Journal of Applied Physiology 14(1): 81-83
Upright
Mean pleural pressure at end-expiration was -5.1cmH20
Mean esophageal pressure at end-expiration was -4.8cmH20
Don't forget to subtract out the structure compression factor!split_city wrote:Supine
Mean pleural pressure at end-expiration was -1.1cmH20
Mean esophageal pressure at end-expiration was +2.6cmH20
Oh for cryin' out loud! I'll give you a couple of cmH20 +/-. But I ain't gonna give you 20.split_city wrote:You have clearly stated that you believe that Pes should be zero at FRC.
StillAnotherGuest wrote:so baseline Pes is normally 0 cmH2OWhat the hey, I'll provide some references to show you that Pes is negative at FRC, thus confirming that Pes does not equal intrapulmonary pressure.StillAnotherGuest wrote:(and for that matter, Pes) are open to air, so if allowed to equilibrate, P will = 0
Sleep lab patients are rarely upright, and even less so at RV, so that significance is unclear to me. And if you look closely at Knowles, you will see that given practical clinical consideration, patients are a heckuva lot closer to Pes = 0 than anything else.split_city wrote:Going back to the first point. Now remember, it has been shown that Pes is considered a relatively good alternative measurement of pleural pressure (in the upright posture anyway), Mead et al (1955), Knowles et al (1959) and Milic-Emili et al (1964) all showed that Pes was positive at RV

SAG

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Keep It Real
Nor would I call the breathing in the +20cmH20 peak expiratory patient "baseline breathing."StillAnotherGuest wrote:As noted:split_city wrote:At full expiration and during forced expiration such as the case during a spirometery test, intrapleural pressure becomes positive. This is why we still have air inside the lungs at RV because the postive pleural pressure compresses the airways, trapping air downstream.
And those manuevers are not considered "normal".SAG wrote:Intrapleural pressure is normally...
I was simply quoting negative Pes numbers because it seemed that you thought Pes = 0 at FRC.StillAnotherGuest wrote:OK, but you're kinda going back and forth here, quoting a bunch of references documenting negative Pes and then adding in mediastinal pressure artifact when the numbers don't fit. Do a wake supine end-expiratory Pes at the begining of the study and then you can properly account for artifact.split_city wrote:I have already discussed the reasons why peak Pes is increased. You must remember, this +20cmH20 also includes the +5-10cmH20 artifact caused by the compression of the medialstinal structures. The true peak value is likely to be between 10-15cmH20.
So taking into account the compression artifact, is an adjusted peak Pes during expiration of between 10-15cmH20 still too high for you?
I meant a an increase i.e. a more positive peak Pes (try saying that 5 times fast) during active expiratory attempts during apneas when abdominal muscles are cranking away.StillAnotherGuest wrote:SAG is confused. Do you mean increased negative or positive peak expiratory Pes? If it occurs during their apneas then how can you have positive Pes? If there's a brief period of increased positive activity post event, then that should be dismissed as normal artifact.split_city wrote:All the other patients also had increased peak expiratory Pes during their apneas. I'm pretty sure peak Pes also increased during hypopneas in other patients.
I will post a snapshot of the patient I had in last night when I next get a chance. He predominantly only had hypopneas during the night. As soon as he fell asleep, he was cranking up is abdominal muscles. Initially, Pes and Pga pressure swings were opposite when he was awake, but Pga peaked during expiration as soon as he went off to sleep.StillAnotherGuest wrote:During that whole period, independent of the surrounding events? I do.split_city wrote: I have no doubt he was actively recruiting his abdominal muscles.
So? You didn't define posture in your original argument.StillAnotherGuest wrote:Very impressive, but for the most part, "upright" is not applicable in the sleep laboratory.split_city wrote:Here is a study comparing pleural pressure with Pes in humans
Mead et al (1959) Journal of Applied Physiology 14(1): 81-83
Upright
Mean pleural pressure at end-expiration was -5.1cmH20
Mean esophageal pressure at end-expiration was -4.8cmH20
Yes, but the initial aim of the study was to determine the effect of posture on both pleural and Pes.StillAnotherGuest wrote:Don't forget to subtract out the structure compression factor!split_city wrote:Supine
Mean pleural pressure at end-expiration was -1.1cmH20
Mean esophageal pressure at end-expiration was +2.6cmH20
Good. I'm glad that's sortedStillAnotherGuest wrote:Oh for cryin' out loud! I'll give you a couple of cmH20 +/-. But I ain't gonna give you 20.split_city wrote:You have clearly stated that you believe that Pes should be zero at FRC.
StillAnotherGuest wrote:so baseline Pes is normally 0 cmH2OWhat the hey, I'll provide some references to show you that Pes is negative at FRC, thus confirming that Pes does not equal intrapulmonary pressure.StillAnotherGuest wrote:(and for that matter, Pes) are open to air, so if allowed to equilibrate, P will = 0
That figure doesn't ignore the compression artifact.StillAnotherGuest wrote:Sleep lab patients are rarely upright, and even less so at RV, so that significance is unclear to me. And if you look closely at Knowles, you will see that given practical clinical consideration, patients are a heckuva lot closer to Pes = 0 than anything else.
SAG
BUT
IF you are in the supine position AND you take into account the compression artifact, THEN true Pes will be close to 0 at FRC. In an UPRIGHT posture, Pes will be subatmospheric at FRC. Agreed??
Here's a question for you. FRC decreases in healthy-weight individuals when moving from an upright position to the supine position. This is partially due to mass loading on the abdomen, displacing the diaphragm cranially. If this is true, why is there little to no decrease in FRC in the obese population following the same postural transition?
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
We'll Be Right Back After These Messages...
Can't chat too much right now, gotta bring the Knowles book back to the library (we got the salient point out of that anyway) and go to a football game (real football, not that rolling around in the dirt thing you guys got).
Meanwhile, post the electrical and biophysical Pes calibrations from that 20 cmH2O patient, that should answer most of these questions.
And also, you might wanna rethink this concept:
Meanwhile, post the electrical and biophysical Pes calibrations from that 20 cmH2O patient, that should answer most of these questions.
And also, you might wanna rethink this concept:
SAGsplit_city wrote:I meant a an increase i.e. a more positive peak Pes (try saying that 5 times fast) during active expiratory attempts during apneas when abdominal muscles are cranking away.

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: We'll Be Right Back After These Messages...
What game are you talking about? You going to a scoccer game or a gridiron match?StillAnotherGuest wrote:Can't chat too much right now, gotta bring the Knowles book back to the library (we got the salient point out of that anyway) and go to a football game (real football, not that rolling around in the dirt thing you guys got).
SAG
I'd rather watch the paint dry thanks....particularly if you're talking about gridiron
Are you talking about australian rules football or rugby for us when you said "not that rolling around in the dirt thing you guys got"
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
Now THAT'S What I'm Talkin' 'Bout...
Gridiron...split_city wrote:....particularly if you're talking about gridiron...
It even sounds manly...

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Now THAT'S What I'm Talkin' 'Bout...
hahahaha...oh the irony!! So manly that the guys who play the game prance around in helmets and padding. Everyone gets so excited when someone passes the ball ten yards. Please let me know when they decide to take off their skirtsStillAnotherGuest wrote:Gridiron...split_city wrote:....particularly if you're talking about gridiron...
It even sounds manly...
Even some of our "old" and "retired" Australian Rules Football players have been recruited over the last few years to play in your manly game.
Anyways, back on topic....
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
Personally, I Think We Should Just Send Food Coupons
I blame Affirmative Action for that (part of the "Give a Poor Aussie A Job" initiative).split_city wrote:Even some of our "old" and "retired" Australian Rules Football players have been recruited over the last few years to play in your manly game.

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Off topic (again)
Here's a link to a youtube video of one of our Aussies in the "manly" sport of NFL. Nice hit on Rocca but he just laughs it off. We are used to these types of bumps (without the pansy helmets and padding) in Aussie Rules
http://www.youtube.com/watch?v=cerDBOd_zlg
A video showing a kick-in from Ben Graham, another Aussie over in the States. The kick was 85m (93 yards).
http://www.youtube.com/watch?v=J47ccoM0Dvg
According to Wiki, "on May 22, 2006, the Jets signed Graham to a six-year contract worth US$5.17 million"
A 75m (82yards) kick from Dustin Fletcher:
http://www.youtube.com/watch?v=J47ccoM0Dvg
http://www.youtube.com/watch?v=cerDBOd_zlg
A video showing a kick-in from Ben Graham, another Aussie over in the States. The kick was 85m (93 yards).
http://www.youtube.com/watch?v=J47ccoM0Dvg
According to Wiki, "on May 22, 2006, the Jets signed Graham to a six-year contract worth US$5.17 million"
A 75m (82yards) kick from Dustin Fletcher:
http://www.youtube.com/watch?v=J47ccoM0Dvg
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
I'm Sure That's Great, But...
Sorry, I don't do "YouTube".
Where's my DC and biocals?
SAG
Where's my DC and biocals?
SAG

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: I'm Sure That's Great, But...
SpoilsportStillAnotherGuest wrote: Sorry, I don't do "YouTube".
Do you simply want me to post some data where I did the calibrations for Pes?StillAnotherGuest wrote:Where's my DC and biocals?
SAG








