Here's an abstract looking at the effect of posture on lung function
Spirometric values of obese and non-obese subjects on orthostatic, sitting and supine positions][Article in Portuguese]
Domingos-Benício NC, Gastaldi AC, Perecin JC, Avena Kde M, Guimarães RC, Sologuren MJ, Lopes-Filho JD.
Centro Universitário do Triângulo (UNIT MG) e Universidade de Cuiabá (UNIC).
BACKGROUND: It is possible that obesity could lead to pulmonary restriction with decreasing lung volumes. However, controversies about this restriction and its etiology still exist. Thus, the purpose of this report was to evaluate the effects of body weigh excess on spirometry, on three different body positions, evaluated by Body Mass Index (BMI), percentage of fatness and the ratio of abdominal girth to hip breadth (AG/HB). METHODS: Forty-six sedentary volunteers, with ages between 20 and 40 years, were studied and distributed on five groups, based on BMI. Skin fold thickness and ratio of abdominal girth to hip breadth (AG/HB) of the volunteers were measured. FVC, FEV1 and ratio of FEV1 to FVC were measured on three different body positions--sitting, supine and orthostatic positions. RESULTS: Comparing the values measured and predicted between the groups, no difference was detected.
Comparing body positions, the supine position shows lower values than sitting and orthostatic positions (p<0.05). Associations between CVF, VEF1 e VEF1/CVF values and BMI, percentage of fatness and ratio of AG/HB were not found. CONCLUSIONS: Spirometric values from obese people are into normality range and decrease on the supine position.
and another...
Spirometry in normal subjects in sitting, prone, and supine positions.Vilke GM, Chan TC, Neuman T, Clausen JL.
Department of Emergency Medicine, UC San Diego Medical Center 92103, USA.
gmvilke@ucsd.edu
OBJECTIVE: Determine whether pulmonary function testing is affected by patient positioning. METHODS: In a descriptive study with measurements made in a sequential but randomized order at a university-based pulmonary function laboratory, 20 healthy men, ages 18-50 years, were evaluated with spirometric assessment of forced vital capacity (FVC), forced expiratory volume in the first second (FEV1), and maximum voluntary ventilation (MVV) in the sitting, supine, and prone positions. Subjects were excluded for body mass index (BMI) > 30 kg/m2 or abnormal baseline spirometry. RESULTS:
Comparing sitting to supine and prone positions, there was a statistically significant decline in the spirometry values (reported as percent of predicted normal +/- standard error of the mean). FVC was 102% +/- 4% while sitting, 95% +/- 4% while supine, and 94% +/- 4% while prone. FEV1 was 104% +/- 3% while sitting, 96% +/- 3% while supine, and 94% +/- 3% while prone. MVV was 115% +/- 4% while sitting, 102% +/- 4% while supine, and 97% +/- 3% prone. CONCLUSION: In healthy men with BMI < 30 kg/m2, changing from the sitting to supine or prone position results in statistically significant change in respiratory pattern. However, all spirometry values in each position were normal by American Thoracic Society definitions.
Now in the obese..
Am J Respir Crit Care Med. 1997 Sep;156(3 Pt 1):998-9. Links
Spirometric values in obese individuals. Effects of body position.Gudmundsson G, Cerveny M, Shasby DM.
Division of Pulmonary, Critical Care and Occupational Medicine, University of Iowa, College of Medicine, Iowa City 52242, USA.
gunnar-gudmundsson@uiowa.edu
Obesity is increasingly prevalent. Earlier studies indicated that there was a significant but small difference in spirometric values between sitting and standing position in the normal population. It is not known if this is true for obese individuals. The recommendations of the American Thoracic Society (ATS) are to document if a spirometry is done in a sitting or standing position. We performed a study in which we compared sitting and standing spirometric values in obese individuals. Patients with a body mass index (BMI) > or = 30 kg/m2 who were referred for spirometry were invited to participate. All tests were done according to American Thoracic Society recommendations. We studied 50 subjects (32 females and 18 males; mean age 45 yr [SD +/- 14.4]). Age range was 20-71 years. Average BMI was 39 (SD +/- 7, range 30 to 65). Twenty-two did the first testing in the sitting position and 28 standing.
There was a small but statistically significant difference between forced vital capacity (FVC) in the standing versus sitting position (Wilcoxen test, p < or = 0.05). There was no significant difference in FEV1 between sitting and standing. Our conclusion is that body position is not important when performing spirometry in persons with BMI > or = 30 kg/m2.
We COULD counduct our PFTs when the patient was in the supine position, but is it really neccessary for my study? Moving all the equipment around just to cater for a supine test probably isn't really worth it. The room I do my testing in really isn't that big. Plus, all the forumale used to determine % predicted were defined in subjects who were upright.
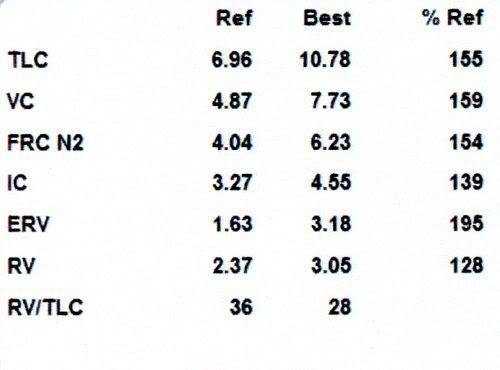
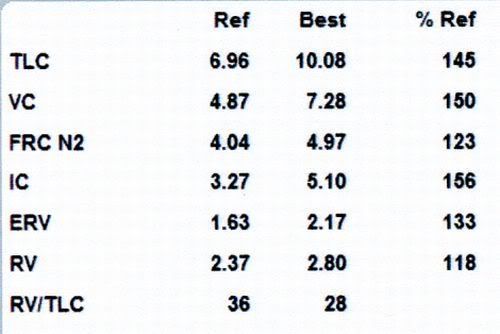
Ok, lung volume stuff. I'm really focussed at lung volume changes (well, lack of) in the obese when moving from an upright position to the supine position.

Why doesn't lung volume decrease in the obese?
We have come up with a couple of theories:
1) FRC is already close to RV in the obese. RV doesn't really change much with alterations in posture. Maybe the additional mass loading on the chest and abdomen isn't enough to further "compress" the lung in the obese?
or
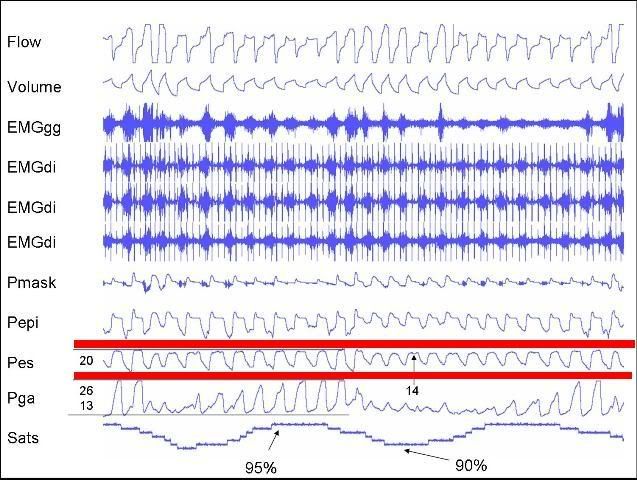
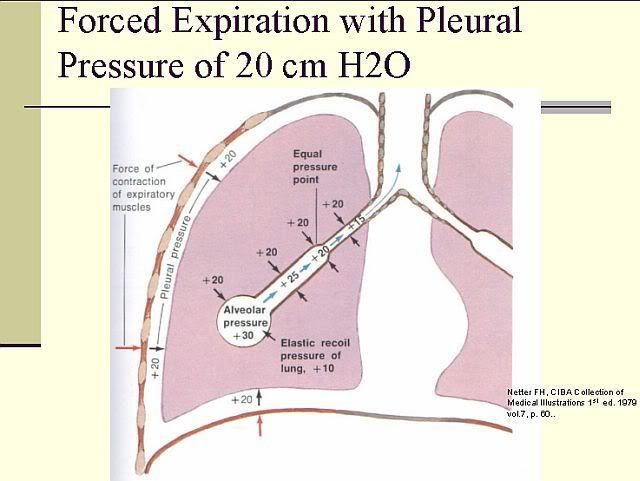
2) Maybe there is some sort of neuromuscular reflex which prevents the diaphragm from ascending, and thus preventing a reduction in lung volume in the obese when they move to the supine posture. Muller actually looked at the effect of abdominal compression on tonic diaphragm activity. The diaphragm is generally electrically inactive at FRC. However, Butler et al 2001 showed that about 4% of costal diaphragm motor units fired tonically. But just for this discussion, the diaphragm is electrically quiet at FRC. Therefore, the position of the diaphragm is partially dependent upon the pressure gradients acting upon the muscle.
Anyways, Muller showed that abdominal compression increased tonic activity of the diaphragm.

This is what they said:
"Our data strongly suggest that there is a stretch reflex
in the diaphragm, which is not surprising given the
presence of spindles. The natural stimulus for this reflex
is the weight of the abdominal contents in the supine
position."
Conversely, they also stated that there was also a decrease in tonic diaphragm activity when the subjects were in REM sleep.
Now, a couple of things to note in their abdominal compression protocol:
1) Abdominal compression wasn't sustained for more than about 30 secs. Is this increased maintained over a longer period?
From our own work, we did show an initial increase in tonic activity during abdominal compression but the activity dissipated after about 30secs and there was no further increase during each of our ten minute periods (I can supply a picture when I get a chance).
2) Diaphragm EMG activity in the Muller paper (and in our study) was measured by an esophageal catheter. The increase in tonic activity may in fact have been an increase in abdominal muscle EMG activity rather than the diaphragm. Maybe the subjects "tensed" up their abdominal muscles during abdominal loading and then relaxed once they got used to the load.
Nevertheless, going back to the lack of change in FRC in the obese. As I said earlier, perhaps the obese do in fact activity defend against a fall in lung volume when moving to the supine position by increasing tonic diaphragm activity. Increasing tonic activity will likely prevent the diaphragm from moving upwards. Maybe this tonic activity is lost at sleep onset, allowing the diaphragm to ascend, resulting in a reduction in FRC. This decrease in FRC will likely increase upper airway collapsibility. However, I have not see any real differences in tonic activity in our obese subjects compared to our healthy weight individuals.