Clueless Family with Apnea--RANT!
- tillymarigold
- Posts: 426
- Joined: Mon Mar 26, 2007 4:01 pm
- Location: Albuquerque, NM
My mother finally got a referral for a sleep study after much prodding from me, but she refuses to get it until after she gets her blood pressure under control and her cardiac problems and joint problems straightened out and loses weight. I tell her that apnea can cause all those things and she says "Yes, but I still want to take care of those other things first."
I think next time she says that I may tell her that if she dies of a heart attack caused by apnea, I'm boycotting her funeral.
I think next time she says that I may tell her that if she dies of a heart attack caused by apnea, I'm boycotting her funeral.
That's interesting. 32 is the age I decided that kids were out of the question.Tasmania wrote:It seems my three half-brothers and I came to the same conclusion all on our own. Not one of us has had kids (I'm the youngest at 32) and when we finally started to talk to each other about why, it turned out none of us wanted to pass on the genetic crap shoot that runs down my dad's side of the family. True... they all tend to be brilliant folks... but that somehow gets offset a wee bit by the high incidence of bi-polar disorder, OCD, OSA, diabetes, heart disease, high blood pressure, obesity, and cancer. Oh and did I mention that all those things seem to run in a pack... get one ... you usually get them all sooner or later...JeffH wrote:Add me to the list. Apnea helped kill my old man, and he had the stubborn gene too.
My family is so nuts I purposely didn't have kids because I knew the gene pool needed to come to an end.
Oh well... there are plenty of cousins out there having kids... so the world won't be missing it's supply of paranoid obsessive terminally ill geniuses anytime soon.
LOL
- sharon1965
- Posts: 1232
- Joined: Thu Jan 18, 2007 4:59 pm
- Location: Windsor, Ontario, Canada
i'm sure my dad has OSA, as i've shared on here before...when i first learned about the disorder, i said, 'dad, this sounds like you! you snooze on the couch ALL THE TIME'...he said, "that's what you do when you're 70"...i said, "you did it when you were 40!" plus he has all the usual signs and symptoms...but yeah, he'll never look into it, he and my mom are both in denial about it...my hubby's brother too, just no talkin' to him
BUT...
one of my brothers went on sunday night for a sleep study! YAYYY...somebody finally listened...of course, sending him reminder emails on an almost constant basis might have influenced things
my niece just emailed me that her hubby got his results...SEVERE!! and the sec. told him his machine would cost around $10,000...anyone ever heard of this? plus the sleep doc wants him to have bariatric surgery
my other brother, (her dad) is booked in this month for his study...
my other 2 brothers don't have any signs or symptoms...at least not that they're admitting...time will tell
but i'm so proud of my bro's and my nephew-in-law...we all know we'd rather bury our heads in the sand than become part of this crazy culture, but it's better than being buried six feet under...
BUT...
one of my brothers went on sunday night for a sleep study! YAYYY...somebody finally listened...of course, sending him reminder emails on an almost constant basis might have influenced things
my niece just emailed me that her hubby got his results...SEVERE!! and the sec. told him his machine would cost around $10,000...anyone ever heard of this? plus the sleep doc wants him to have bariatric surgery
my other brother, (her dad) is booked in this month for his study...
my other 2 brothers don't have any signs or symptoms...at least not that they're admitting...time will tell
but i'm so proud of my bro's and my nephew-in-law...we all know we'd rather bury our heads in the sand than become part of this crazy culture, but it's better than being buried six feet under...
If you always do what you've always done, you'll always get what you've always got...
I had determined that kids were out of the question - period, end of story.JeffH wrote:...That's interesting. 32 is the age I decided that kids were out of the question.
LOL
My oldest was born when I was 38. My little guy is 2 years younger. They'll be 3 and 5 in a few months.
Late-Night Pillow Snorkeler.
I'm 51 now, so my decision took.___H wrote:I had determined that kids were out of the question - period, end of story.JeffH wrote:...That's interesting. 32 is the age I decided that kids were out of the question.
LOL
My oldest was born when I was 38. My little guy is 2 years younger. They'll be 3 and 5 in a few months.
-
Guest
- socknitster
- Posts: 1740
- Joined: Fri Jun 01, 2007 11:55 am
- Location: Pennsylvania
- Contact:
I used to think I would be crazy to pass on all the crazy genes in my family--all from one the one side. Heart, hi bp, diabetes, not to mention two generations of breast cancer (my grandfather (the titleholder) and my mom--and yes MEN can get breast cancer). There was a time in my life when I felt like a ticking time bomb. How could I pass that on?
I remember talking to friends about these thoughts and they were like, "Hey, every family has stuff like that. You aren't unique." I was like, "Oh." So, my desire for a child outweighed my paranoia eventually. I was 31 when I had Harry and I have never regretted it for a moment, he is the best thing that ever happened to me.
Later I discovered that my paranoia, anxiety and likely all the ailments I was so freaking worried about were probably due to sleep apnea. I don't know if anyone has pinned cancer to apnea yet, but I'm going to guess that all the stress hormones in an apneic's bod can't be hindering a tumor from growing.
So, if in your heart of hearts you want a child, go for it. Don't let your ancestors scare you off it. You shouldn't have to pay for the mistakes/foibles/poor medical care of your forefathers.
This article is so interesting that split_city posted because my 4 year old was just diagnosed with apnea. His ENT doc says a tonsil and adenoid surgery is 99% likely to cure it--his are GIGANTOID. In the discussion of the article, page 10 or 11, the author discusses how it is thought that apnea itself can cause the airway to become smaller over time--the condition worsens because the apnea causes so much trauma in the area.
Considering how much relief I have gotten from my tonsilectomy (7/30/07) I really think I might be saving my son from ever developing this disorder. Of course, I will be the nag from hell if I ever suspect it has recurred when he is older, but WOW! To save him from all of this. I feel so blessed, it brings tears to my eyes. Someday he will die from something, but I hope it won't be apnea or its myriad of related diseases. That alone, deserves a prayer of thanks.
Jen
I remember talking to friends about these thoughts and they were like, "Hey, every family has stuff like that. You aren't unique." I was like, "Oh." So, my desire for a child outweighed my paranoia eventually. I was 31 when I had Harry and I have never regretted it for a moment, he is the best thing that ever happened to me.
Later I discovered that my paranoia, anxiety and likely all the ailments I was so freaking worried about were probably due to sleep apnea. I don't know if anyone has pinned cancer to apnea yet, but I'm going to guess that all the stress hormones in an apneic's bod can't be hindering a tumor from growing.
So, if in your heart of hearts you want a child, go for it. Don't let your ancestors scare you off it. You shouldn't have to pay for the mistakes/foibles/poor medical care of your forefathers.
This article is so interesting that split_city posted because my 4 year old was just diagnosed with apnea. His ENT doc says a tonsil and adenoid surgery is 99% likely to cure it--his are GIGANTOID. In the discussion of the article, page 10 or 11, the author discusses how it is thought that apnea itself can cause the airway to become smaller over time--the condition worsens because the apnea causes so much trauma in the area.
Considering how much relief I have gotten from my tonsilectomy (7/30/07) I really think I might be saving my son from ever developing this disorder. Of course, I will be the nag from hell if I ever suspect it has recurred when he is older, but WOW! To save him from all of this. I feel so blessed, it brings tears to my eyes. Someday he will die from something, but I hope it won't be apnea or its myriad of related diseases. That alone, deserves a prayer of thanks.
Jen
_________________
| Machine: ResMed AirSense™ 10 AutoSet™ CPAP Machine with HumidAir™ Heated Humidifier |
| Mask: ResMed AirFit™ F30 Full Face CPAP Mask with Headgear |
Add my family to the list. My dad currently has heart problems, diabetes, kidney problems (dialysis) and cancer. He's been diagnosed with apnea for a few years and will not get treatment. I don't know exactly what the problem was but he never even went home with a machine. Oh and he used to have snoring contests with the saint bernard that we had when I was a kid.
My mother doesn't sleep well and probably should get a study done, but she won't... she spends more time dealing with my dad's issues than her own.
My mother doesn't sleep well and probably should get a study done, but she won't... she spends more time dealing with my dad's issues than her own.
-
CollegeGirl
- Posts: 1038
- Joined: Thu Oct 20, 2005 6:49 pm
- Location: VA
Jen, my family is the same way.
I have two aunts and an uncle who refuse to use their CPAPs. "I just can't sleep with it" they say. But then when I offer to help them select masks/machines that will actually make it comfortable, or to help them advocate to their DMEs, or to help them talk to their doctors...they never take me up on it.
My stepdad, whom I've posted about multiple times here, is claustrophobic, and refuses to use his, regardless of all the help I've offered. Here's the kicker - he can't get to sleep, so he takes sleeping pills. I've told him how dangerous this is with untreated apnea - he keeps saying he's going to talk to his doctor. He never does. He has high blood pressure, GERD, all sorts of health issues caused by apnea.
I'm 99% sure my mom has apnea. She has snored, snorted, and choked my whole life. She refuses to get tested, and admits it's because (like with everything else in her life) if she doesn't know there's something wrong, nothing bad will happen (or at least, that's what she thinks).
Sigh. I totally feel you, Jen. It is SO frustrating!
I have two aunts and an uncle who refuse to use their CPAPs. "I just can't sleep with it" they say. But then when I offer to help them select masks/machines that will actually make it comfortable, or to help them advocate to their DMEs, or to help them talk to their doctors...they never take me up on it.
My stepdad, whom I've posted about multiple times here, is claustrophobic, and refuses to use his, regardless of all the help I've offered. Here's the kicker - he can't get to sleep, so he takes sleeping pills. I've told him how dangerous this is with untreated apnea - he keeps saying he's going to talk to his doctor. He never does. He has high blood pressure, GERD, all sorts of health issues caused by apnea.
I'm 99% sure my mom has apnea. She has snored, snorted, and choked my whole life. She refuses to get tested, and admits it's because (like with everything else in her life) if she doesn't know there's something wrong, nothing bad will happen (or at least, that's what she thinks).
Sigh. I totally feel you, Jen. It is SO frustrating!
Machine: M-Series Auto
Mask: Headrest
No humidifier
On the hose since 2005.
Mask: Headrest
No humidifier
On the hose since 2005.
sharon1965
Great job getting some of the family to have the study and get the treatment. Wow! Progress in the face of all the stories about stubborn resistance. It is nice to hear a success in all the " My relatives will not listen" posts.
My younger brother was referred for a study and was dragging his feet, as some of us have done. He had been MIA for a long time. Call him and you got someone in the middle of a nap, at any hour. I told him to get on with the study and get his life back. So far, he has had the study but no cpap yet. They like to get two sleep studies and payments before providing a machine in this area. I'm waiting to see if he makes it all the way to compliance.
Congrats on your success!!
Great job getting some of the family to have the study and get the treatment. Wow! Progress in the face of all the stories about stubborn resistance. It is nice to hear a success in all the " My relatives will not listen" posts.
My younger brother was referred for a study and was dragging his feet, as some of us have done. He had been MIA for a long time. Call him and you got someone in the middle of a nap, at any hour. I told him to get on with the study and get his life back. So far, he has had the study but no cpap yet. They like to get two sleep studies and payments before providing a machine in this area. I'm waiting to see if he makes it all the way to compliance.
Congrats on your success!!
- sharon1965
- Posts: 1232
- Joined: Thu Jan 18, 2007 4:59 pm
- Location: Windsor, Ontario, Canada
thanks daddysaur
i do feel pretty good about it, even though i felt like i was as annoying as a poke in the eye, but it was worth it to get the phone call from my brother telling me his psg was booked...so now he's waiting for results
my niece's husband is only in his late 20's and about 200 lbs overweight...they had their second child last christmas, and as i ooed and awwed over the little guy, i said to dad, "congrats on baby #2...too bad you won't be around to watch them grow up, huh?"...must have hit a nerve, since my niece told me she'd been trying to get him to go for ages...she even works at a clinic and could refer him herself! but after talking to me and hearing my experience, he decided to go...not sure what made her dad (my other bro) go, except maybe the fact that he remarried in august...i think his new wife pushed him to go...whatever it takes
now if i could just get my dad, who is otherwise an incredibly intelligent man, to listen to reason...
man, if i'd known about OSA sooner, wild horses couldn't have kept me from a sleep study...go figure
i do feel pretty good about it, even though i felt like i was as annoying as a poke in the eye, but it was worth it to get the phone call from my brother telling me his psg was booked...so now he's waiting for results
my niece's husband is only in his late 20's and about 200 lbs overweight...they had their second child last christmas, and as i ooed and awwed over the little guy, i said to dad, "congrats on baby #2...too bad you won't be around to watch them grow up, huh?"...must have hit a nerve, since my niece told me she'd been trying to get him to go for ages...she even works at a clinic and could refer him herself! but after talking to me and hearing my experience, he decided to go...not sure what made her dad (my other bro) go, except maybe the fact that he remarried in august...i think his new wife pushed him to go...whatever it takes
now if i could just get my dad, who is otherwise an incredibly intelligent man, to listen to reason...
man, if i'd known about OSA sooner, wild horses couldn't have kept me from a sleep study...go figure
If you always do what you've always done, you'll always get what you've always got...
Add some strange mental stuff to the mix and that was the main reason I made the decision I did. Physical stuff had very little to do with it.socknitster wrote:I used to think I would be crazy to pass on all the crazy genes in my family--all from one the one side. Heart, hi bp, diabetes, not to mention two generations of breast cancer (my grandfather (the titleholder) and my mom--and yes MEN can get breast cancer). There was a time in my life when I felt like a ticking time bomb. How could I pass that on?
I remember talking to friends about these thoughts and they were like, "Hey, every family has stuff like that. You aren't unique." I was like, "Oh." So, my desire for a child outweighed my paranoia eventually. I was 31 when I had Harry and I have never regretted it for a moment, he is the best thing that ever happened to me.
Later I discovered that my paranoia, anxiety and likely all the ailments I was so freaking worried about were probably due to sleep apnea. I don't know if anyone has pinned cancer to apnea yet, but I'm going to guess that all the stress hormones in an apneic's bod can't be hindering a tumor from growing.
So, if in your heart of hearts you want a child, go for it. Don't let your ancestors scare you off it. You shouldn't have to pay for the mistakes/foibles/poor medical care of your forefathers.
This article is so interesting that split_city posted because my 4 year old was just diagnosed with apnea. His ENT doc says a tonsil and adenoid surgery is 99% likely to cure it--his are GIGANTOID. In the discussion of the article, page 10 or 11, the author discusses how it is thought that apnea itself can cause the airway to become smaller over time--the condition worsens because the apnea causes so much trauma in the area.
Considering how much relief I have gotten from my tonsilectomy (7/30/07) I really think I might be saving my son from ever developing this disorder. Of course, I will be the nag from hell if I ever suspect it has recurred when he is older, but WOW! To save him from all of this. I feel so blessed, it brings tears to my eyes. Someday he will die from something, but I hope it won't be apnea or its myriad of related diseases. That alone, deserves a prayer of thanks.
Jen
- goose
- Posts: 1382
- Joined: Sun Mar 11, 2007 7:59 pm
- Location: The left coast - CA... If you're not living on the edge, you're taking up too much space!!
Hey ya'll,
Won't even go into the whole family history -- suffice it to say that I'm the only one on the machine -- all others in denial. Apnea's only one thing for denial though....one younger brother ignores hiBP and diabetes -- can't understand why I take it so seriously. AND he's got 4 kids (grown, but still)...
I don't know anyone that's come out of this alive -- something is going to kill us all, but why not try to extend the ride a bit??
Feel your frustration Jen -- still working on RN wife who is also in denial...."Oh I'll go get tested when yours is all taken care of"......Mine has been taken care of since June!!!!!!! I told her the other day I was going to get more insurance on her.....
You might try that one -- just ask them if it's ok for you to take out some additional life insurance on them......when they ask why, just say, "I can use the Money, and it won't be that long 'till I get it".......
cheers
goose
Won't even go into the whole family history -- suffice it to say that I'm the only one on the machine -- all others in denial. Apnea's only one thing for denial though....one younger brother ignores hiBP and diabetes -- can't understand why I take it so seriously. AND he's got 4 kids (grown, but still)...
I don't know anyone that's come out of this alive -- something is going to kill us all, but why not try to extend the ride a bit??
Feel your frustration Jen -- still working on RN wife who is also in denial...."Oh I'll go get tested when yours is all taken care of"......Mine has been taken care of since June!!!!!!! I told her the other day I was going to get more insurance on her.....
You might try that one -- just ask them if it's ok for you to take out some additional life insurance on them......when they ask why, just say, "I can use the Money, and it won't be that long 'till I get it".......
cheers
goose
_________________
| Humidifier: HC150 Heated Humidifier With Hose, 2 Chambers and Stand |
| Additional Comments: Also Use ComfortGel (s); Headrest (XL) and a PAP-Cap. |
Wars arise from a failure to understand one another's humanness. Instead of summit meetings, why not have families meet for a picnic and get to know each other while the children play together?
-the Dalai Lama
-the Dalai Lama
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
Yeah, But What Exactly Is Hereditary...
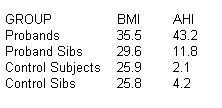
I wouldn't even go so far as to say that that's interesting. Those guys go through all the trouble to get matched study sets but severity in the proband sibs is only 25% of that of the probands (AHI 43.2 +/- 26.3 vs 11.8 +/- 16.6).split_city wrote:Talking about family members and OSA, here's an interesting paper by Richard Schwab.
All I see is a loose weight relationship:
(I'm such a Mango.)
Running around with a tape measure while you're awake is all well and good, but it's all about what happens when you go to sleep:
SAGCon: Sleep Apnea Is Not an Anatomic Disorder
Kingman P. Strohl, M.D., Center for Sleep Disorders Research, Louis Stokes Cleveland DVA Medical Center, Case Western Reserve University, Cleveland, Ohio
The most fundamental argument for neural events as initiating obstructive sleep apnea is the fact that closure of the pharyngeal airway occurs during sleep. In sleep, there is a reorganization of cortical (e.g., neural) control that includes changes in direct cortical drive to and peripheral reflex control of the muscles of the chest wall and upper airway and ventilation. The disease-defining event is state-related, requiring sleep in the presentation of the disease-obstructive sleep apnea–hypopnea syndrome. The presence of an anatomic encroachment of the upper airway by itself does not produce an obstruction. Obesity, tonsillar hypertrophy, neuromuscular disease, and a craniopharyngeal anomaly are risk factors present during wakefulness but do not invariably produce obstructive sleep apnea. Apparent anatomic predispositions require greater levels of upper airway muscle activity to maintain an open airway during wakefulness. With sleep onset, however, this neural compensation is reduced, thus providing the fundamental cause.
In the original analysis as well as in peer-reviewed published records by others, electromyographic recordings of patients with obstructive sleep apnea consistently inform me that respiratory muscle activity declines before and with the onset of the first obstructive breath. (The main limitation of using these studies is that they are contaminated with state changes. Increased upper airway muscle activity with arousal as well as the "startle"-like effect that Horner talks about could create an illusion that upper airway activity is decreased and that that is why apnea occurs. The timing data, however, are more compelling. Upper airway activity begins before pump muscles. This is observed not only in the genioglossus muscle but also in other muscles of the upper airway, including the alae nasi, a muscle loaded by intrapharyngeal events. Even if phasic activity is observed, preceding the obstruction or early in the obstructive event there is a reduction or reversal in the interval between the onset of activation of pharyngeal muscles and either the onset of inspiratory flow or chest wall muscle activation. In contrast, those individuals without sleep apnea exhibit a consistent (100–200 milliseconds) interval of preactivation before the events of inspiration, an interval that is more apparent at sleep onset and with sleep than during wakefulness. Furthermore, individuals with evidence of inspiratory flow limitation (individuals without apnea who snore) are dependent on their ventilatory motor output to preserve upper airway patency during sleep. In such individuals, mild hypoxia or mild hypocapnia is needed to precipitate occlusion—findings that indicate the critical role of respiratory control in the determination of sleep apnea. Therefore, for one obstructive apnea to occur there is an attenuation of neuromuscular activation in both amount and coordination that permits the airway to close. Once closed, other neural events, such as motor coordination, inertia in the control system, and/or arousal from sleep, determine apnea length. The main point is that to close a nasopharynx during sleep a deactivation of neuromuscular drive is required, and then to reopen the air passage another set of neural events acts to determine duration and recovery of the obstruction.
One apnea is not enough. Obstructive sleep apnea–hypopnea syndrome is characterized by many obstructive events of a given length (greater than 10 seconds in the adult). The repetitive waxing and waning of ventilation in obstructive sleep apnea–hypopnea syndrome is initiated and sustained by a respiratory control (e.g., neural) system. Short-term potentiation of ventilation, or ventilatory after-discharge, is a phenomenon that can be evoked by brief hypoxia exposure, promotes ventilatory stability, and protects against dysrhythmic breathing. An absence of short-term potentiation is reported for patients with obstructive sleep apnea–hypopnea syndrome or for patients with congestive heart failure who have recurrent central sleep apnea—Cheyne–Stokes respiration. Finally, central and obstructive apneas may occur in the same patient over a night indicating that the neural tendency to cycle is the fundamental event and that upper airway obstruction is not essential for the development of recurrent neural apneas.
Periodic breathing is subject to fundamental analysis. Sleep, increased time delay, and decreased damping of the system are known to promote respiratory instability through "loop gain". Mathematical models predict a correlation between the incidence of periodic breathing and hypoxic sensitivity; indeed, Cheyne–Stokes respiration (periodic breathing) during sleep occurs more frequently in those with congestive heart failure and higher peripheral chemosensitivity. In the case of obstructive sleep apnea, added effects of reflex responses to airway occlusion and/or the arousal needed to open an occluded airway serve to create an "overshoot" in ventilatory drive and make it more likely to cycle. Hence, neural factors produce and can either amplify or attenuate the probability of having the repetitive events that lead to sleep apnea syndrome.
In summary, obstructive sleep apnea is precipitated and maintained by neural events. Our focus should be on optimizing neural drive to muscles that maintain upper airway patency during sleep and on preventing the next apnea though stabilization of respiratory control. In essence, the therapeutic goal is to keep the airway awake and let the brain sleep.

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Yeah, But What Exactly Is Hereditary...
StillAnotherGuest wrote:I wouldn't even go so far as to say that that's interesting. Those guys go through all the trouble to get matched study sets but severity in the proband sibs is only 25% of that of the probands (AHI 43.2 +/- 26.3 vs 11.8 +/- 16.6).split_city wrote:Talking about family members and OSA, here's an interesting paper by Richard Schwab.
All I see is a loose weight relationship:
(I'm such a Mango.)
Running around with a tape measure while you're awake is all well and good, but it's all about what happens when you go to sleep:
SAGCon: Sleep Apnea Is Not an Anatomic Disorder
Kingman P. Strohl, M.D., Center for Sleep Disorders Research, Louis Stokes Cleveland DVA Medical Center, Case Western Reserve University, Cleveland, Ohio
The most fundamental argument for neural events as initiating obstructive sleep apnea is the fact that closure of the pharyngeal airway occurs during sleep. In sleep, there is a reorganization of cortical (e.g., neural) control that includes changes in direct cortical drive to and peripheral reflex control of the muscles of the chest wall and upper airway and ventilation. The disease-defining event is state-related, requiring sleep in the presentation of the disease-obstructive sleep apnea–hypopnea syndrome. The presence of an anatomic encroachment of the upper airway by itself does not produce an obstruction. Obesity, tonsillar hypertrophy, neuromuscular disease, and a craniopharyngeal anomaly are risk factors present during wakefulness but do not invariably produce obstructive sleep apnea. Apparent anatomic predispositions require greater levels of upper airway muscle activity to maintain an open airway during wakefulness. With sleep onset, however, this neural compensation is reduced, thus providing the fundamental cause.
In the original analysis as well as in peer-reviewed published records by others, electromyographic recordings of patients with obstructive sleep apnea consistently inform me that respiratory muscle activity declines before and with the onset of the first obstructive breath. (The main limitation of using these studies is that they are contaminated with state changes. Increased upper airway muscle activity with arousal as well as the "startle"-like effect that Horner talks about could create an illusion that upper airway activity is decreased and that that is why apnea occurs. The timing data, however, are more compelling. Upper airway activity begins before pump muscles. This is observed not only in the genioglossus muscle but also in other muscles of the upper airway, including the alae nasi, a muscle loaded by intrapharyngeal events. Even if phasic activity is observed, preceding the obstruction or early in the obstructive event there is a reduction or reversal in the interval between the onset of activation of pharyngeal muscles and either the onset of inspiratory flow or chest wall muscle activation. In contrast, those individuals without sleep apnea exhibit a consistent (100–200 milliseconds) interval of preactivation before the events of inspiration, an interval that is more apparent at sleep onset and with sleep than during wakefulness. Furthermore, individuals with evidence of inspiratory flow limitation (individuals without apnea who snore) are dependent on their ventilatory motor output to preserve upper airway patency during sleep. In such individuals, mild hypoxia or mild hypocapnia is needed to precipitate occlusion—findings that indicate the critical role of respiratory control in the determination of sleep apnea. Therefore, for one obstructive apnea to occur there is an attenuation of neuromuscular activation in both amount and coordination that permits the airway to close. Once closed, other neural events, such as motor coordination, inertia in the control system, and/or arousal from sleep, determine apnea length. The main point is that to close a nasopharynx during sleep a deactivation of neuromuscular drive is required, and then to reopen the air passage another set of neural events acts to determine duration and recovery of the obstruction.
One apnea is not enough. Obstructive sleep apnea–hypopnea syndrome is characterized by many obstructive events of a given length (greater than 10 seconds in the adult). The repetitive waxing and waning of ventilation in obstructive sleep apnea–hypopnea syndrome is initiated and sustained by a respiratory control (e.g., neural) system. Short-term potentiation of ventilation, or ventilatory after-discharge, is a phenomenon that can be evoked by brief hypoxia exposure, promotes ventilatory stability, and protects against dysrhythmic breathing. An absence of short-term potentiation is reported for patients with obstructive sleep apnea–hypopnea syndrome or for patients with congestive heart failure who have recurrent central sleep apnea—Cheyne–Stokes respiration. Finally, central and obstructive apneas may occur in the same patient over a night indicating that the neural tendency to cycle is the fundamental event and that upper airway obstruction is not essential for the development of recurrent neural apneas.
Periodic breathing is subject to fundamental analysis. Sleep, increased time delay, and decreased damping of the system are known to promote respiratory instability through "loop gain". Mathematical models predict a correlation between the incidence of periodic breathing and hypoxic sensitivity; indeed, Cheyne–Stokes respiration (periodic breathing) during sleep occurs more frequently in those with congestive heart failure and higher peripheral chemosensitivity. In the case of obstructive sleep apnea, added effects of reflex responses to airway occlusion and/or the arousal needed to open an occluded airway serve to create an "overshoot" in ventilatory drive and make it more likely to cycle. Hence, neural factors produce and can either amplify or attenuate the probability of having the repetitive events that lead to sleep apnea syndrome.
In summary, obstructive sleep apnea is precipitated and maintained by neural events. Our focus should be on optimizing neural drive to muscles that maintain upper airway patency during sleep and on preventing the next apnea though stabilization of respiratory control. In essence, the therapeutic goal is to keep the airway awake and let the brain sleep.














