UARS Advice
- Jay Aitchsee
- Posts: 2936
- Joined: Sun May 22, 2011 12:47 pm
- Location: Southwest Florida
Re: UARS Advice
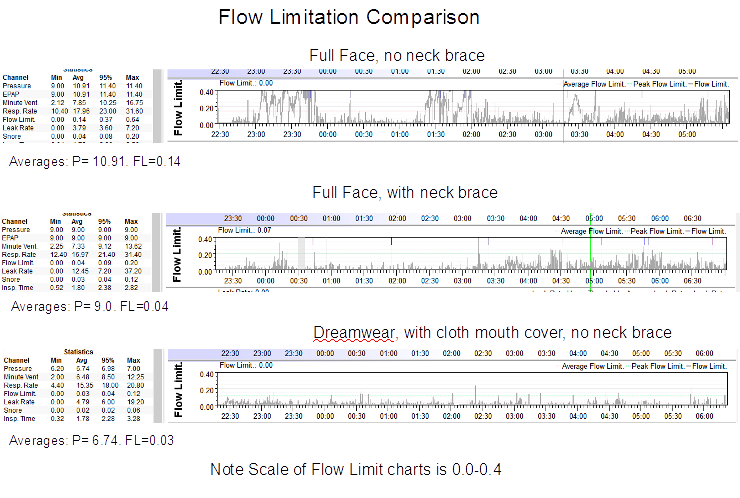
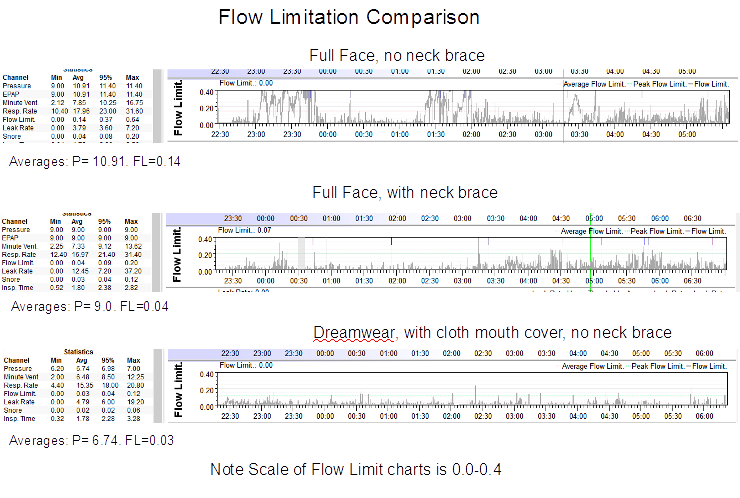
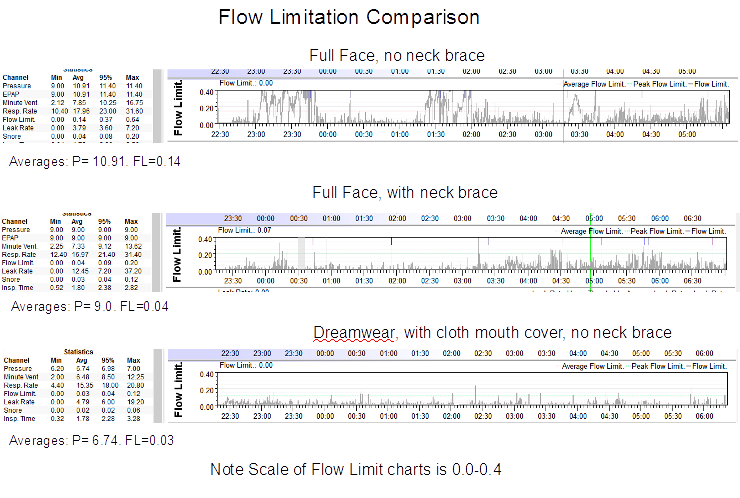
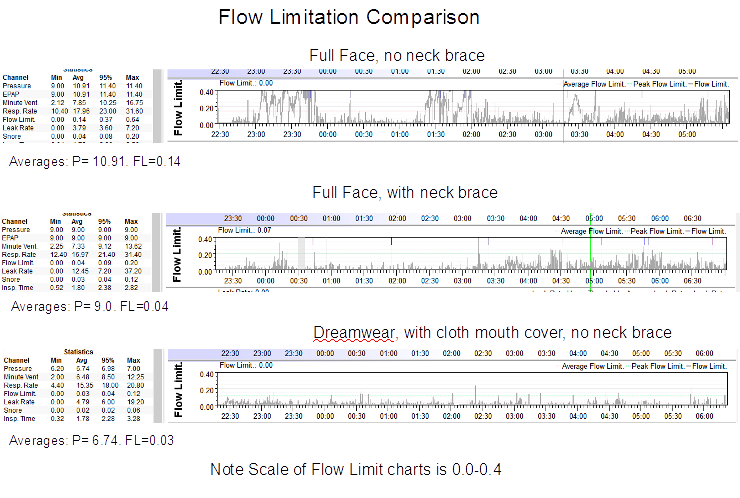
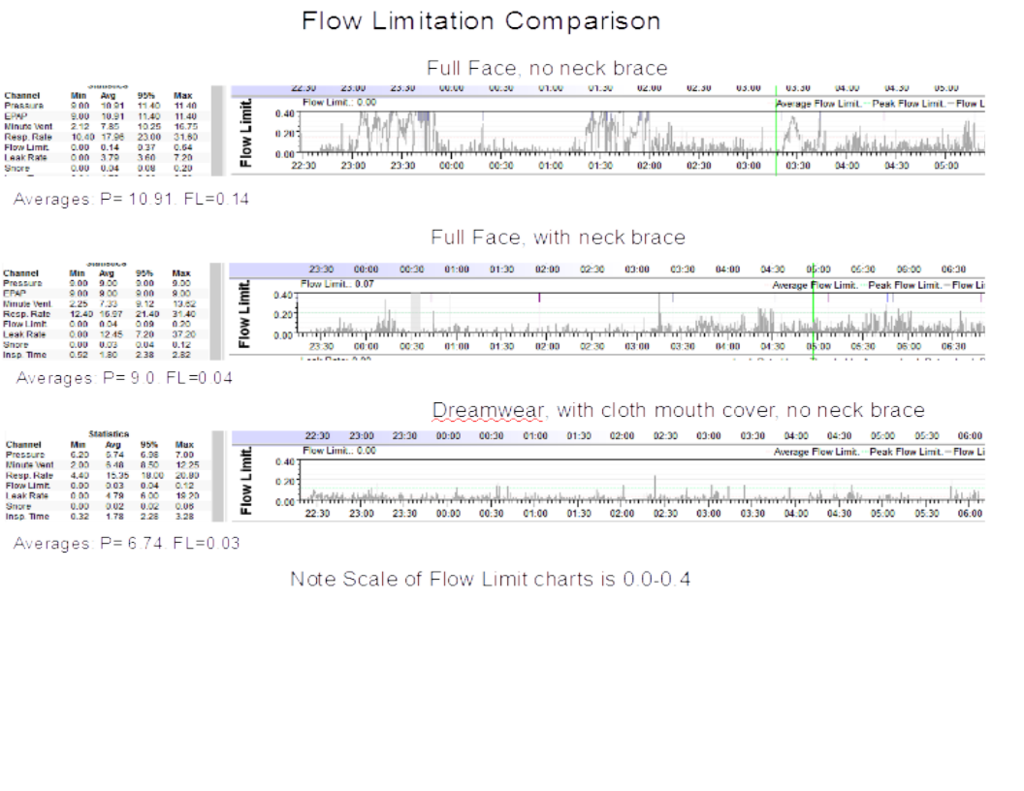
Here's some results I've had with various configurations. I am a mouth leaker and thought I could not use a nasal masks after several failed attempts over the years. However, a nerve problem with the FFM headgear forced me to change over a year ago and it has worked out quite well, I am surprised to say. The examples below are meant to be typical and all have low AHI and acceptable leak rates. Notice the reduction in P required from top to bottom. Also notice the use of cloth mouth cover instead of tape to control mouth leaks with the nasal mask. Cloth is not only more comfortable, but it also allows autonomous changes in respiratory dead space which tape does not and which I think is critical to success - a subject for another thread.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: S9 Auto, P10 mask, P=7.0, EPR3, ResScan 5.3, SleepyHead V1.B2, Windows 10, ZEO, CMS50F, Infrared Video |
Re: UARS Advice
Those are too small to read.
What do you mean by cloth mouth cover ?
What reduced the pressure and how did it effect treating other events?
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 Autoset machine; Ruby chinstrap under the mask straps; ResScan 5.6 |
- Jay Aitchsee
- Posts: 2936
- Joined: Sun May 22, 2011 12:47 pm
- Location: Southwest Florida
Re: UARS Advice
Yeah, thanks Avi. I realize they were kind of small, but the graphics are large enough to see the relative sizes in FLow Limitation Waves. I did add the average values for Pressure and Flow Limitations in larger type. 95% Leak Values in the three examples are 3.6, 7.2, and 6.0 top to bottom.
What the posting is meant to demonstrate is, for me, Flow Limitations and the Pressures required to suppress apneas and hypopneas are reduced when using soft cervical collar with a FFM. (The therapy pressure for each configuration was determined by titration. The AHI of each example is less than one).
Additionally, it demonstrates that Flow Limitations and the Pressures required to suppress apneas and hypopneas are further reduced by using a Nasal mask (in this case the Dreamwear) with a soft mouth cover.
A mouth cover is used to restrict expiratory mouth flow (mouth Leaks) with a nasal mask. Many people use tape. See this for the mouth cover I am using: viewtopic.php?f=1&t=112758&st=0&sk=t&sd=a#p1086296 . It's a headband that is worn over the mouth and around the back of the head instead of around the forehead.
I'll see if I can reproduce the graphics a little larger for you.
Here: It's a little fuzzy, but maybe a little better.
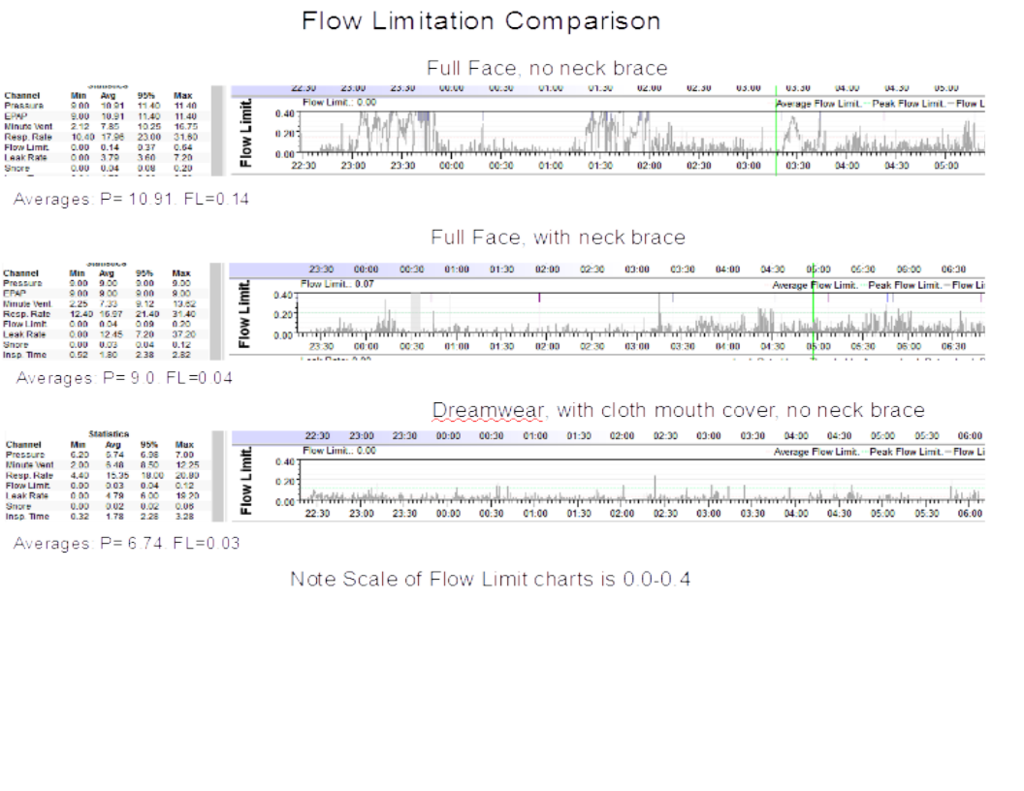
What the posting is meant to demonstrate is, for me, Flow Limitations and the Pressures required to suppress apneas and hypopneas are reduced when using soft cervical collar with a FFM. (The therapy pressure for each configuration was determined by titration. The AHI of each example is less than one).
Additionally, it demonstrates that Flow Limitations and the Pressures required to suppress apneas and hypopneas are further reduced by using a Nasal mask (in this case the Dreamwear) with a soft mouth cover.
A mouth cover is used to restrict expiratory mouth flow (mouth Leaks) with a nasal mask. Many people use tape. See this for the mouth cover I am using: viewtopic.php?f=1&t=112758&st=0&sk=t&sd=a#p1086296 . It's a headband that is worn over the mouth and around the back of the head instead of around the forehead.
I'll see if I can reproduce the graphics a little larger for you.
Here: It's a little fuzzy, but maybe a little better.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: S9 Auto, P10 mask, P=7.0, EPR3, ResScan 5.3, SleepyHead V1.B2, Windows 10, ZEO, CMS50F, Infrared Video |
Re: UARS Advice
put your glasses on!avi123 wrote:Those are too small to read.
Get OSCAR
Accounts to put on the foe list: dataq1, clownbell, gearchange, lynninnj, mper!?, DreamDiver, Geer1, almostadoctor, sleepgeek, ajack, stom, mogy, D.H., They often post misleading, timewasting stuff.
Accounts to put on the foe list: dataq1, clownbell, gearchange, lynninnj, mper!?, DreamDiver, Geer1, almostadoctor, sleepgeek, ajack, stom, mogy, D.H., They often post misleading, timewasting stuff.
- Jay Aitchsee
- Posts: 2936
- Joined: Sun May 22, 2011 12:47 pm
- Location: Southwest Florida
Re: UARS Advice
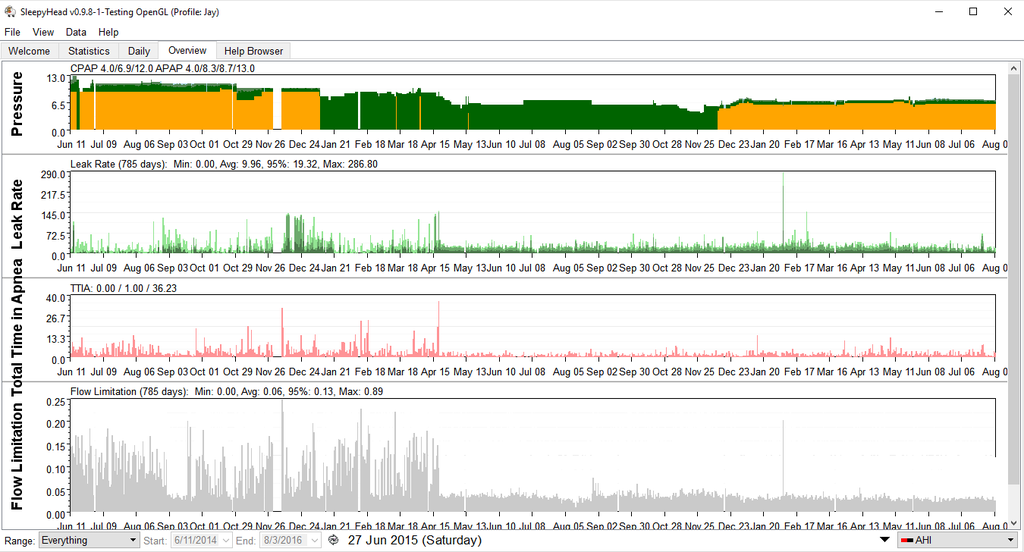
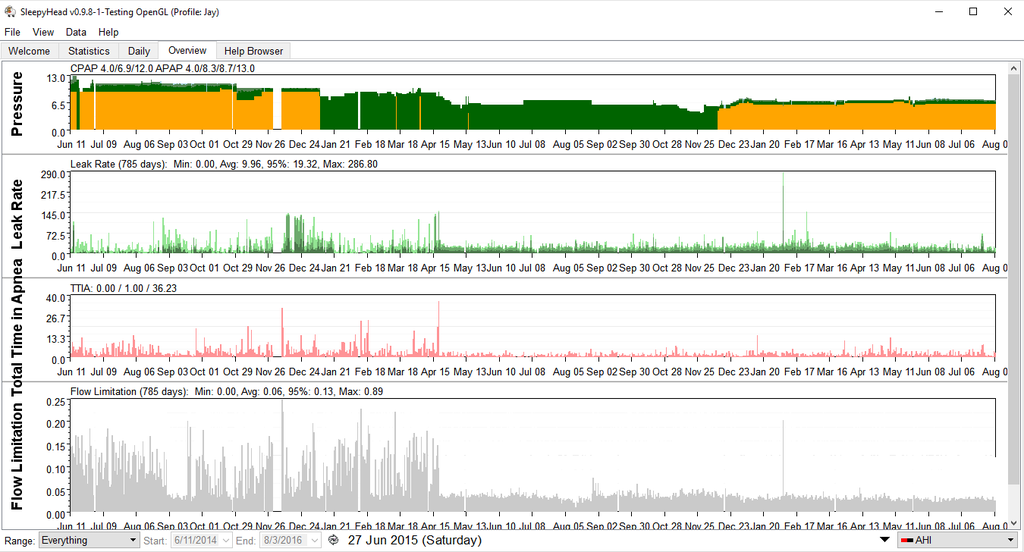
Guess when I switched to a Nasal Mask
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: S9 Auto, P10 mask, P=7.0, EPR3, ResScan 5.3, SleepyHead V1.B2, Windows 10, ZEO, CMS50F, Infrared Video |
-
dudemandude
- Posts: 9
- Joined: Thu Dec 31, 2015 9:34 pm
Re: UARS Advice
Here's yesterdays results, AHI of 2.72 and woke up every 3 hours or so and quickly fell back to sleep. I don't know if this is relevant but I've had a string of higher AHI days(1.8 +) after a string of < 1 AHI days at the same exact pressure, mostly because of increasing centrals. The only difference in actual sleep behavior was using various techniques to clear my nose and nasal strips so I think I may be getting a higher amount of centrals because of the same pressure but larger amount of airflow through the nose somehow throwing me off but I can't really know for sure. I don't feel as sleepy as I usually do but I'm fairly tired and brain fogged.

This is what my graphs looked like for a few days ago at the same exact pressure but no nasal optimization. AHI is .80

This set of graphs looks a lot better but the fact of the matter is I felt absolutely awful the day after. I've sometimes found that higher AHI is a good sign for me and I've attributed it to getting deeper sleep and higher AHI in REM but I don't really know whats up.
Seeing these results would you try higher pressures or lower ones with the same nasal optimization? I'm somewhat inclined to try lower straight pressure to try to reduce centrals but I don't really have a good idea of what to try next.

This is what my graphs looked like for a few days ago at the same exact pressure but no nasal optimization. AHI is .80

This set of graphs looks a lot better but the fact of the matter is I felt absolutely awful the day after. I've sometimes found that higher AHI is a good sign for me and I've attributed it to getting deeper sleep and higher AHI in REM but I don't really know whats up.
Seeing these results would you try higher pressures or lower ones with the same nasal optimization? I'm somewhat inclined to try lower straight pressure to try to reduce centrals but I don't really have a good idea of what to try next.
- ChicagoGranny
- Posts: 15451
- Joined: Sun Jan 29, 2012 1:43 pm
- Location: USA
Re: UARS Advice
This is normal sleep. Don't obsess over awakenings with quick return to sleep.dudemandude wrote:woke up every 3 hours or so and quickly fell back to sleep
Of more concern is:
dudemandude wrote:fairly tired and brain fogged.
- Jay Aitchsee
- Posts: 2936
- Joined: Sun May 22, 2011 12:47 pm
- Location: Southwest Florida
Re: UARS Advice
Dude, I agree with Granny. Don't obsess over any aspect of sleep. You are worrying about things without cause and worry will ruin sleep.
The first thing you need to do is understand and practice good sleep hygiene. I'm sure Granny will post her summary list of do's and don'ts. But Google it anyway.
Next you have to understand what the data is telling you. You have minimal Flow Limitations with a few centrals and a few OA's mostly in the evening and morning where you are probably awake or drifting in and out of sleep. Events that occur while you are awake don't count! Events that occur while you are awake don't count! The machine doesn't know if you are awake or asleep. It assumes, if the blower is on, you are asleep and reports events that occur. But...events that occur while you are awake don't count.
Ordinary CPAP is designed to prevent obstructive apnea by applying pressure to stent open the airway. Obstructive apnea occurs because your airway is blocked, likely by your tongue falling back into it. The pressure overcomes the blockage.
CA, on the other hand, means that you have stopped trying to breathe. The airway is open but you are not drawing a breath. The brain is not telling the muscles of the chest and diaphragm to act to draw in a breath. There is no blockage, therefore increasing the pressure will not treat CA.
Since most of your events during the night were CA, you now should be able to answer the question of should you increase the pressure to improve your AHI. But, in case you can't, the answer is no. Increased pressure will not treat CA and may, if fact, make it worse.
A few CA are normal. A few CA are normal. You roll over, hold your breath, the machine scores a CA. Normal. You wake briefly, hold your breath, the machine scores a CA, normal. A few CA are normal. Waking a few times in the night and easily falling back to sleep is normal.
Stop worrying about things you don't have. Learn and understand what the data is telling you. Practice good sleep hygiene. Stop worrying. If fatigue continues after your apnea is controlled (as it appears to be) and you are practicing good sleep hygiene, see your doctor.
Edit: I see where Granny did post her checklist early in this thread, but I didn't see where you acknowledged it. Until you can honestly say you have taken care of everything on the list you are just grasping at straws and wasting your time trying to treat a condition (like UARS) that you may or may not have. Lots of things can cause fatigue: deficiencies, lifestyle, meds, and a myriad other things, chief among them is depression.
The first thing you need to do is understand and practice good sleep hygiene. I'm sure Granny will post her summary list of do's and don'ts. But Google it anyway.
Next you have to understand what the data is telling you. You have minimal Flow Limitations with a few centrals and a few OA's mostly in the evening and morning where you are probably awake or drifting in and out of sleep. Events that occur while you are awake don't count! Events that occur while you are awake don't count! The machine doesn't know if you are awake or asleep. It assumes, if the blower is on, you are asleep and reports events that occur. But...events that occur while you are awake don't count.
Ordinary CPAP is designed to prevent obstructive apnea by applying pressure to stent open the airway. Obstructive apnea occurs because your airway is blocked, likely by your tongue falling back into it. The pressure overcomes the blockage.
CA, on the other hand, means that you have stopped trying to breathe. The airway is open but you are not drawing a breath. The brain is not telling the muscles of the chest and diaphragm to act to draw in a breath. There is no blockage, therefore increasing the pressure will not treat CA.
Since most of your events during the night were CA, you now should be able to answer the question of should you increase the pressure to improve your AHI. But, in case you can't, the answer is no. Increased pressure will not treat CA and may, if fact, make it worse.
A few CA are normal. A few CA are normal. You roll over, hold your breath, the machine scores a CA. Normal. You wake briefly, hold your breath, the machine scores a CA, normal. A few CA are normal. Waking a few times in the night and easily falling back to sleep is normal.
Stop worrying about things you don't have. Learn and understand what the data is telling you. Practice good sleep hygiene. Stop worrying. If fatigue continues after your apnea is controlled (as it appears to be) and you are practicing good sleep hygiene, see your doctor.
Edit: I see where Granny did post her checklist early in this thread, but I didn't see where you acknowledged it. Until you can honestly say you have taken care of everything on the list you are just grasping at straws and wasting your time trying to treat a condition (like UARS) that you may or may not have. Lots of things can cause fatigue: deficiencies, lifestyle, meds, and a myriad other things, chief among them is depression.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: S9 Auto, P10 mask, P=7.0, EPR3, ResScan 5.3, SleepyHead V1.B2, Windows 10, ZEO, CMS50F, Infrared Video |
Last edited by Jay Aitchsee on Fri Aug 05, 2016 3:35 pm, edited 1 time in total.
-
dudemandude
- Posts: 9
- Joined: Thu Dec 31, 2015 9:34 pm
Re: UARS Advice
These events occurred when I was asleep, right now my sleep schedule is kinda screwed but it is fairly consistent(3 am to 11-12ish or so) I was told by the specialist in my clinic who deals with delayed sleep phase syndrome that that kind of schedule should not be the cause of my symptoms, although I'll probably have to change it when I start working. I am however beginning to work on setting it back and have got most of Granny's list of things down, although not all, I am working on that. I am not worried about CA or my AHI in general, I did ask whether i should LOWER my pressure in case someone thought the CA was relevant, in general I have found little correlation between my AHI and how I feel and I only included that data in case someone else thought it was relevant. I have ruled out all of the other typical causes of fatigue through blood work and doctor consultation. The reason im "grasping at straws with UARS" is because I'm fairly certain I have it, I went to one of the best ENT specialists for UARS after I made this post and he said I met all of the diagnostic criteria after examining me and looking at my sleep study. In addition while in Pittsburgh for college, I had a consultation with doctors at UPMC sleep center who saw my stats and suspected it as well. As far as I can understand, UARS is about optimizing your therapy in ways that people with regular apnea do not often have to do because there is a suspected nervous system component that makes you very susceptible to even some of the more minute problems with breathing. This is why my ENT recommended I first try various ways to just optimize my nasal breathing because something as simple as that sometimes helps the CPAP actually work for people with UARS, even though I am a good candidate for surgery(really large tonsils). If you look at Tan's case, his final treatment that worked was not all that different then the treatments he was trying with APAP before, especially with regards to AHI, even though it made a world of difference with regard to how he is feeling. There are many cases in this forums history of people with UARS having to "grasp at straws" even though their sleepyhead data looked great from a typical apnea perspective before they could get the treatment that helped them. This is why I'm trying to see if there's anyone who can help me understand my graphs to give me a hint on how I might be able to further optimize my treatment.Jay Aitchsee wrote:Dude, I agree with Granny. Don't obsess over any aspect of sleep. You are worrying about things without cause and worry will ruin sleep.
The first thing you need to do is understand and practice good sleep hygiene. I'm sure Granny will post her summary list of do's and don'ts. But Google it anyway.
Next you have to understand what the data is telling you. You have a few centrals and a few OA's mostly in the evening and morning where you are probably awake or drifting in and out of sleep. Events that occur while you are awake don't count! Events that occur while you are awake don't count! The machine doesn't know if you are awake or asleep. It assumes, if the blower is on, you are asleep and reports events that occur. But...events that occur while you are awake don't count.
Ordinary CPAP is designed to prevent obstructive apnea by applying pressure to stent open the airway. Obstructive apnea occurs because your airway is blocked, likely by your tongue falling back into it. The pressure overcomes the blockage.
CA, on the other hand, means that you have stopped trying to breathe. The airway is open but you are not drawing a breath. The brain is not telling the muscles of the chest and diaphragm to act to draw in a breath. There is no blockage, therefore increasing the pressure will not treat CA.
Since most of your events during the night were CA, you now should be able to answer the question of should you increase the pressure to improve your AHI. But, in case you can't, the answer is no. Increased pressure will not treat CA and may, if fact, make it worse.
A few CA are normal. A few CA are normal. You roll over, hold your breath, the machine scores a CA. Normal. You wake briefly, hold your breath, the machine scores a CA, normal. A few CA are normal. Waking a few times in the night and easily falling back to sleep is normal.
Stop worrying about things you don't have. Learn and understand what the data is telling you. Practice good sleep hygiene. Stop worrying. If fatigue continues after your apnea is controlled (as it appears to be) and you are practicing good sleep hygiene, see your doctor.
Edit: I see where Granny did post her checklist early in this thread, but I didn't see where you acknowledged it. Until you can honestly say you have taken care of everything on the list you are just grasping at straws and wasting your time trying to treat a condition (like UARS) that you may or may not have. Lots of things can cause fatigue: deficiencies, lifestyle, meds, and a myriad other things, chief among them is depression.
- Jay Aitchsee
- Posts: 2936
- Joined: Sun May 22, 2011 12:47 pm
- Location: Southwest Florida
Re: UARS Advice
Dude, Re your last: Good.
To answer your earlier questions directly: I did not see anything in your sleep reports to optimize. In my opinion, it is always better to try lowering the pressure, first.
"Fixing" sleep often takes a very methodical and disciplined approach, eliminating possible problems one a time. It does sound like you do understand that and are trying to take a disciplined approach, I wish you the best and good luck with your quest.
.
To answer your earlier questions directly: I did not see anything in your sleep reports to optimize. In my opinion, it is always better to try lowering the pressure, first.
"Fixing" sleep often takes a very methodical and disciplined approach, eliminating possible problems one a time. It does sound like you do understand that and are trying to take a disciplined approach, I wish you the best and good luck with your quest.
.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: S9 Auto, P10 mask, P=7.0, EPR3, ResScan 5.3, SleepyHead V1.B2, Windows 10, ZEO, CMS50F, Infrared Video |
Re: UARS Advice
I am under impression that he does, and not only UARS. Here is what he wrote in his initial post:Jay Aitchsee wrote: Edit: I see where Granny did post her checklist early in this thread, but I didn't see where you acknowledged it. Until you can honestly say you have taken care of everything on the list you are just grasping at straws and wasting your time trying to treat a condition (like UARS) that you may or may not have
Which leaves some 15 events an hour to something else.Naturally, I went to a sleep doctor and got a sleep study which revealed that while my AHI was around 2.5, I had an average of 37.4 arousals per hour, 21.7 of them respiratory and, according to the report
Also, it would be good to see the summary stats from the left part of a typical daily SleepyHead screenschot (min, max, pressures and other). I disagree that wakening every 3 hours is normal, but this could certainly be normalized with a good sleep hygiene
_________________
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
Re: UARS Advice
Please demonstrate the left part of your SleepyHead screenshot.dudemandude wrote:These events occurred when I was asleep, right now my sleep schedule is kinda screwed but it is fairly consistent(3 am to 11-12ish or so) I was told by the specialist in my clinic who deals with delayed sleep phase syndrome that that kind of schedule should not be the cause of my symptoms, although I'll probably have to change it when I start working. I am however beginning to work on setting it back and have got most of Granny's list of things down, although not all, I am working on that. I am not worried about CA or my AHI in general, I did ask whether i should LOWER my pressure in case someone thought the CA was relevant, in general I have found little correlation between my AHI and how I feel and I only included that data in case someone else thought it was relevant. I have ruled out all of the other typical causes of fatigue through blood work and doctor consultation. The reason im "grasping at straws with UARS" is because I'm fairly certain I have it, I went to one of the best ENT specialists for UARS after I made this post and he said I met all of the diagnostic criteria after examining me and looking at my sleep study. In addition while in Pittsburgh for college, I had a consultation with doctors at UPMC sleep center who saw my stats and suspected it as well. As far as I can understand, UARS is about optimizing your therapy in ways that people with regular apnea do not often have to do because there is a suspected nervous system component that makes you very susceptible to even some of the more minute problems with breathing. This is why my ENT recommended I first try various ways to just optimize my nasal breathing because something as simple as that sometimes helps the CPAP actually work for people with UARS, even though I am a good candidate for surgery(really large tonsils). If you look at Tan's case, his final treatment that worked was not all that different then the treatments he was trying with APAP before, especially with regards to AHI, even though it made a world of difference with regard to how he is feeling. There are many cases in this forums history of people with UARS having to "grasp at straws" even though their sleepyhead data looked great from a typical apnea perspective before they could get the treatment that helped them. This is why I'm trying to see if there's anyone who can help me understand my graphs to give me a hint on how I might be able to further optimize my treatment.Jay Aitchsee wrote:Dude, I agree with Granny. Don't obsess over any aspect of sleep. You are worrying about things without cause and worry will ruin sleep.
The first thing you need to do is understand and practice good sleep hygiene. I'm sure Granny will post her summary list of do's and don'ts. But Google it anyway.
Next you have to understand what the data is telling you. You have a few centrals and a few OA's mostly in the evening and morning where you are probably awake or drifting in and out of sleep. Events that occur while you are awake don't count! Events that occur while you are awake don't count! The machine doesn't know if you are awake or asleep. It assumes, if the blower is on, you are asleep and reports events that occur. But...events that occur while you are awake don't count.
Ordinary CPAP is designed to prevent obstructive apnea by applying pressure to stent open the airway. Obstructive apnea occurs because your airway is blocked, likely by your tongue falling back into it. The pressure overcomes the blockage.
CA, on the other hand, means that you have stopped trying to breathe. The airway is open but you are not drawing a breath. The brain is not telling the muscles of the chest and diaphragm to act to draw in a breath. There is no blockage, therefore increasing the pressure will not treat CA.
Since most of your events during the night were CA, you now should be able to answer the question of should you increase the pressure to improve your AHI. But, in case you can't, the answer is no. Increased pressure will not treat CA and may, if fact, make it worse.
A few CA are normal. A few CA are normal. You roll over, hold your breath, the machine scores a CA. Normal. You wake briefly, hold your breath, the machine scores a CA, normal. A few CA are normal. Waking a few times in the night and easily falling back to sleep is normal.
Stop worrying about things you don't have. Learn and understand what the data is telling you. Practice good sleep hygiene. Stop worrying. If fatigue continues after your apnea is controlled (as it appears to be) and you are practicing good sleep hygiene, see your doctor.
Edit: I see where Granny did post her checklist early in this thread, but I didn't see where you acknowledged it. Until you can honestly say you have taken care of everything on the list you are just grasping at straws and wasting your time trying to treat a condition (like UARS) that you may or may not have. Lots of things can cause fatigue: deficiencies, lifestyle, meds, and a myriad other things, chief among them is depression.
Also, the only issues with APAP were it didn't provide sufficient EPR and its cycle/trigger couldn't be set to "very sensitive", but it's not necessary the same in your case.
What are the other non-respiratory events from your sleep study reports?
What do you mean by "inclined to try to lower straight pressure"? Are you not using EPR? (hence my request above to show your stats on the left of SH screenshot)
_________________
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
-
dudemandude
- Posts: 9
- Joined: Thu Dec 31, 2015 9:34 pm
Re: UARS Advice
Here it is for yesterdays data. 
For the second set of data we have

I currently have EPR set at 3 but I honestly can't tell the difference between EPR 0 or 3 at this point I just have it at three because I've read that UARS people often require larger pressure differentials. I had 21.7 resp arousals and 15.7 spontaneous arousals. My RERA index was 21.9 an hour and my general RDI was 24 an hour.
By inclined to try lower pressures I meant lower my pressure while keeping the same EPR, I had tried lower pressures before but not while optimizing nasal breathing. Also again thanks so much for your help!

For the second set of data we have

I currently have EPR set at 3 but I honestly can't tell the difference between EPR 0 or 3 at this point I just have it at three because I've read that UARS people often require larger pressure differentials. I had 21.7 resp arousals and 15.7 spontaneous arousals. My RERA index was 21.9 an hour and my general RDI was 24 an hour.
By inclined to try lower pressures I meant lower my pressure while keeping the same EPR, I had tried lower pressures before but not while optimizing nasal breathing. Also again thanks so much for your help!
Re: UARS Advice
why is the pressure fixed?
I feel a lot different with EPR=3 (easier) and EPR=0 (harder).
I feel a lot different with EPR=3 (easier) and EPR=0 (harder).
_________________
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
-
dudemandude
- Posts: 9
- Joined: Thu Dec 31, 2015 9:34 pm
Re: UARS Advice
I haven't really noticed any difference between EPR 3 and EPR 0 but I've kept it at EPR 3 because why not and I've heard it helps some people. There's no particular reason that I have it at a fixed pressure as opposed to a variable one, I thought it'd make it easier for me to find the right pressure for me but I've had my CPAp on APAP ranges before as well.









