NotMuffy wrote:OK, I have a question (or two):
What exactly do you hope to accomplish?
- Live longer
- Sleep better
- Feel better
Do you think AHI 0.0 will accomplish that goal(s)?
Well that is the $64,000 question, isn't it?
I wish I had a better and shorter answer for you: But the real scoop is that as much as I've been
thinking about this question ("What exactly do you hope to accomplish?") for the last 9 months (since the diagnosis), I don't yet have a definitive answer because the answer has changed over time.
I can tell you the "moving line" answers:
At the time of DIAGNOSIS
At the very start of this misadventure, my answer to the question "What exactly do you hope to accomplish?" literally was:
- I have to do this thing because both my PCP and the sleep doctor have told me in no uncertain terms that I need to be put on CPAP because the diagnosis was moderate OSA and there is no other viable option for treatment.
Not a particularly good reason I admit, but this is what was going through my head during August and September when I was still in the stage of accepting the diagnosis and researching the local DMEs and learning what I could about OSA and CPAP machines in general.
Near as I can remember, the PCP's rationale of
why I needed to be on CPAP was to
minimize and/or
prevent any further damage to my body from the OSA and to
prevent the OSA from becoming worse over time. A bit of
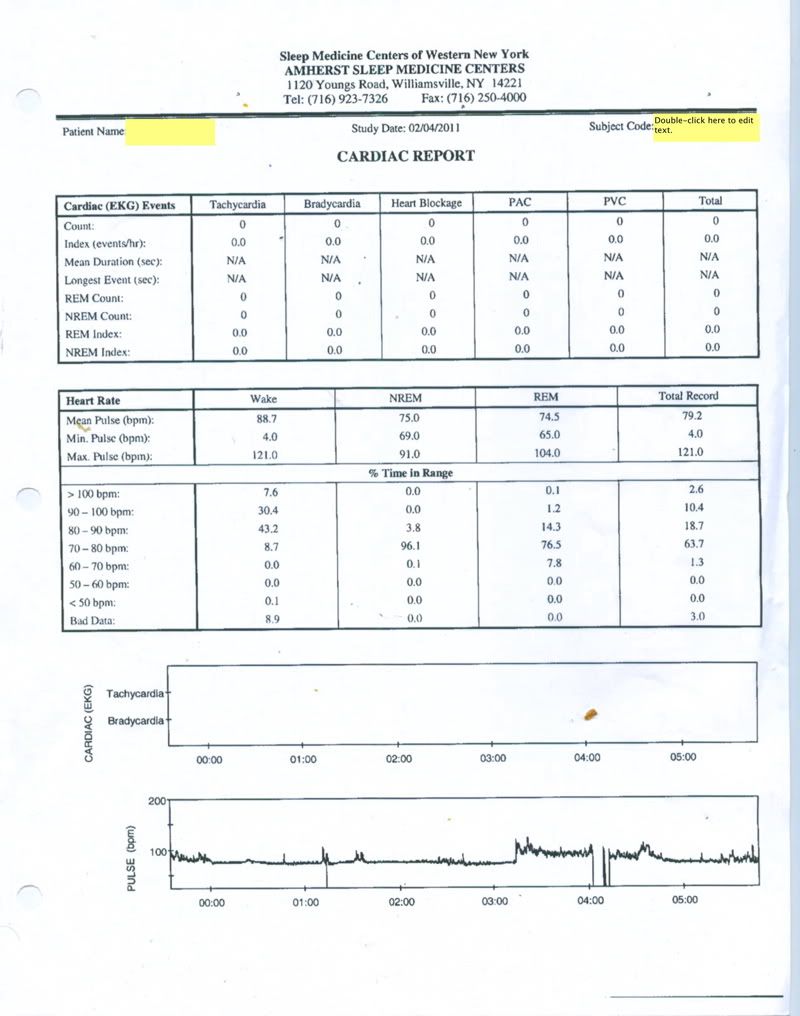
Start it now while you are still healthy instead of waiting for the OSA to get worse and start triggering real problems with your cardiovascular system and increasing your risk of strokes. if you will.
And as I've said on the other thread, the sleep doc's rationale for
why I needed to be on CPAP was a heavy dose of
You'll feel better soon with some
treating the OSA will minimize and/or prevent any further damage to my body from the OSA and prevent the OSA from becoming worse over time thrown in for good measure.
At the time of STARTING THERAPY
By the time I took delivery on the S9 Autoset and actually
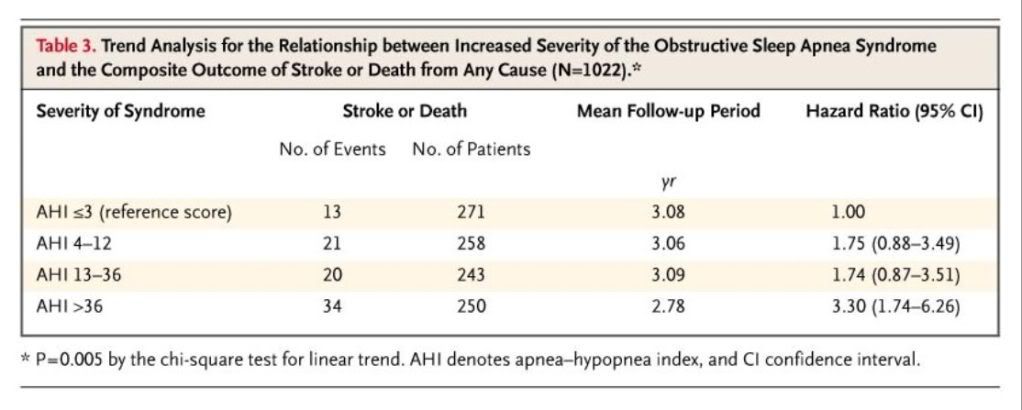
started therapy, I'd become much more knowledgeable about the long term affects of untreated OSA. Several of the co-morbidities run in my family (on both sides). In particular I have cousins, uncles, and grandparents (of both genders) who have died of heart disease, stroke, or high blood pressure or diabetes related problems before the age of 75---sometimes substantially before the age of 75. I also have grandparents who spent the last decade or more of their life suffering from long term effects of one or more of these co-morbidities before dying at an age of less than 75. So at the
start of this adventure, I'd say that MY answer to "What exactly do you hope to accomplish?" was clearly:
- Live longer and stay healthier longer by being on CPAP.
I expected some adjustment problems to therapy---particularly since I didn't have any of the severe daytime symptoms that so many report here. But I also didn't expect a severe crash and burn in terms of daytime functioning either.
During the worst of the Crash and Burn period last fall
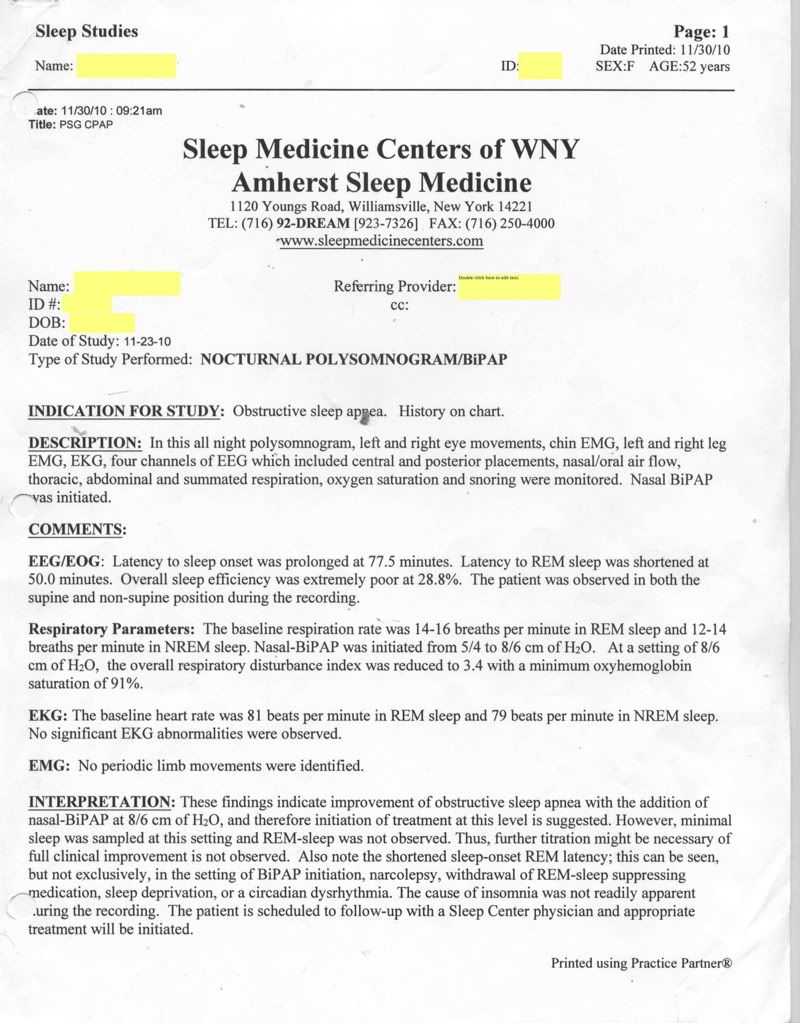
The absolute worst period during my adjustment period has been late October through early December. Before the switch to BiPAP and while the insomnia monster was starting to grow fat and large and overwhelming. During this time, my answer to "What exactly do you hope to accomplish?" was highly pragmatic on a night-to-night basis:
- Don't give in to sleeping without the mask tonight because then I'll never sleep with the mask again in my whole life regardless of what happens with the untreated OSA in the future.
Fear can be a powerful motivator and at this point, the fear that I'd never be able to use the machine if/when it became clear that my OSA had deteriorated to the point of clearly needing it was a powerful motivator to keep me masking up every single night in spite of the growing disruption to my nightly sleep and my daily life.
On a more larger scale, my goal had become more vague and less satisfying:
- (1) Stick with it LONG enough to see if I might actually get used to sleeping with the hose without it so intensely bothering me and (2) stick with it LONG enough to see it might ever do me some good in some kind of (undefined) way.
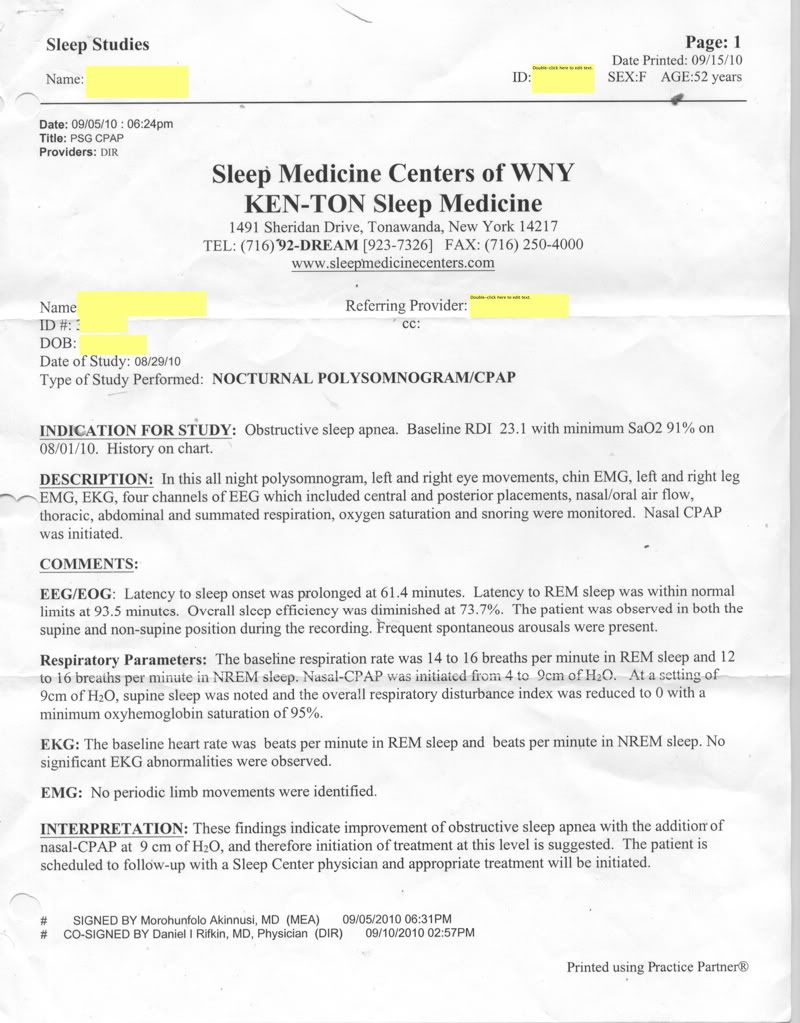
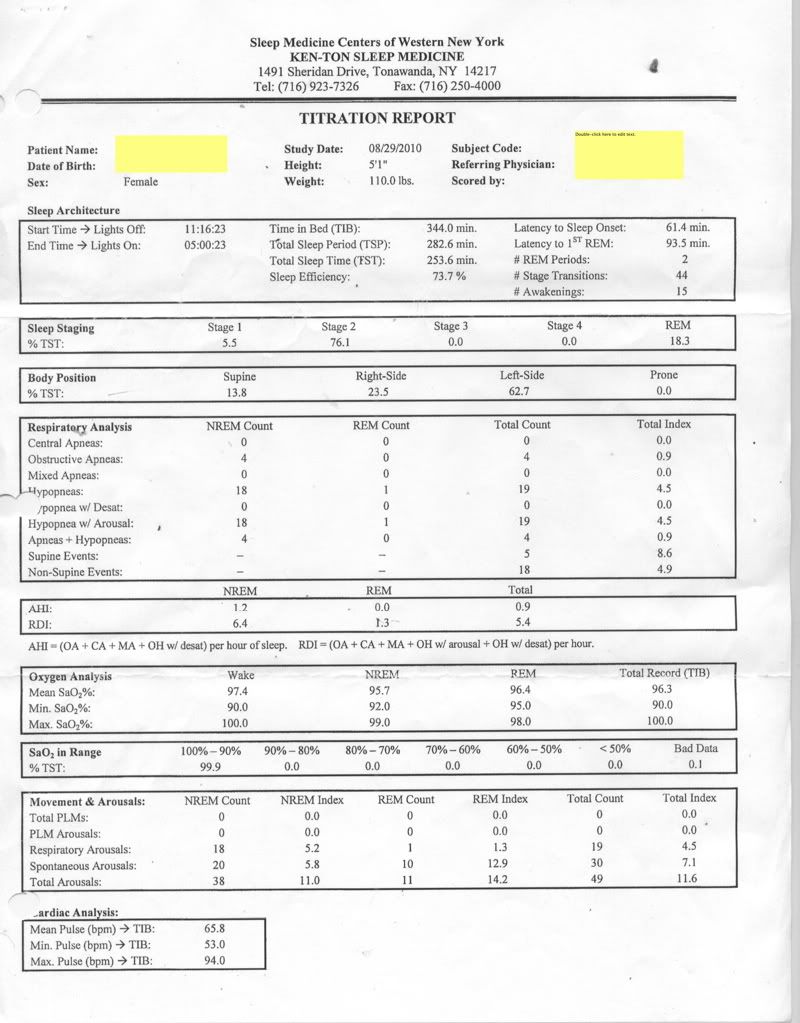
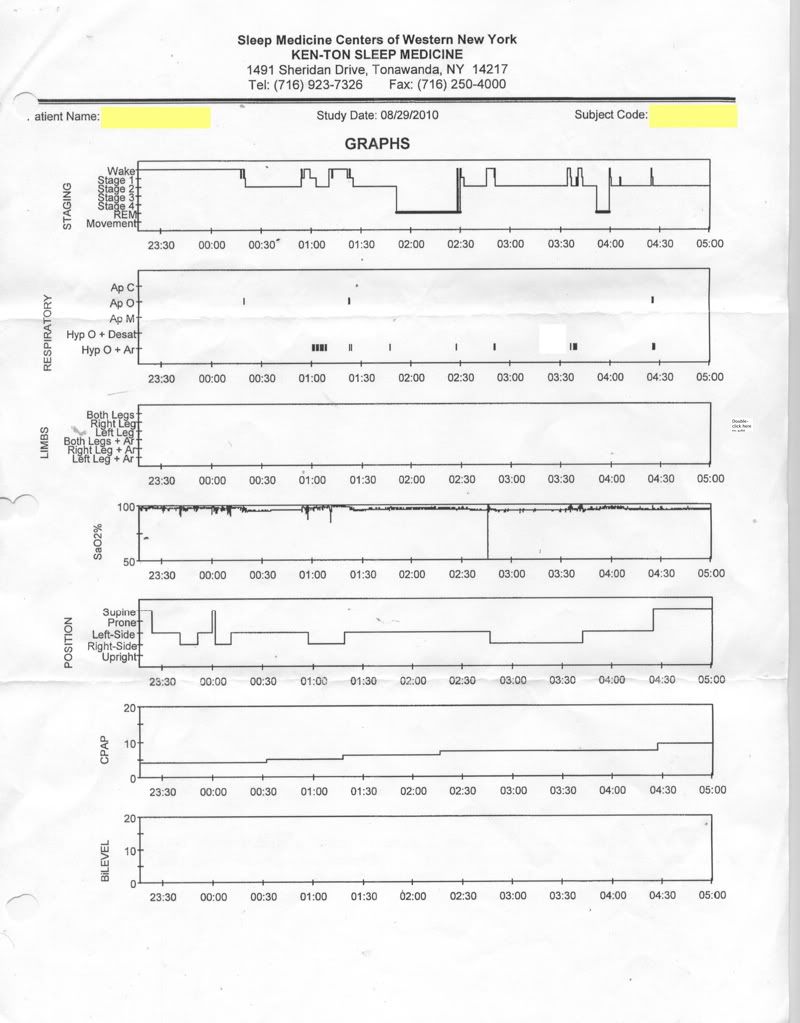
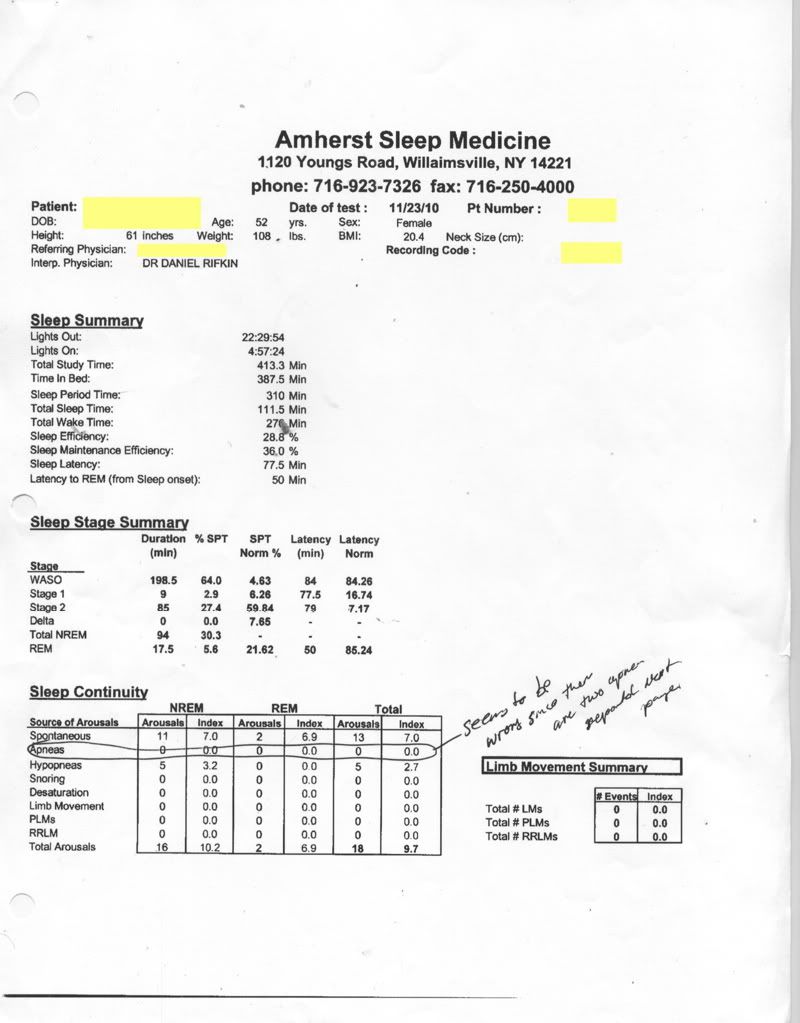
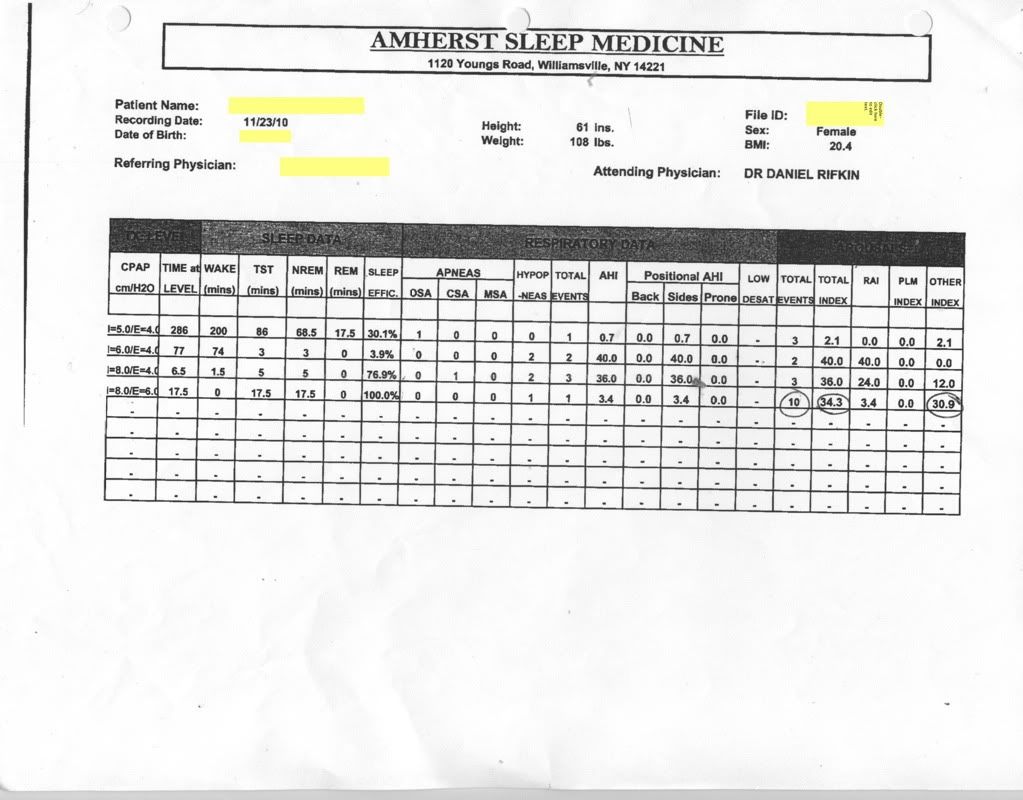
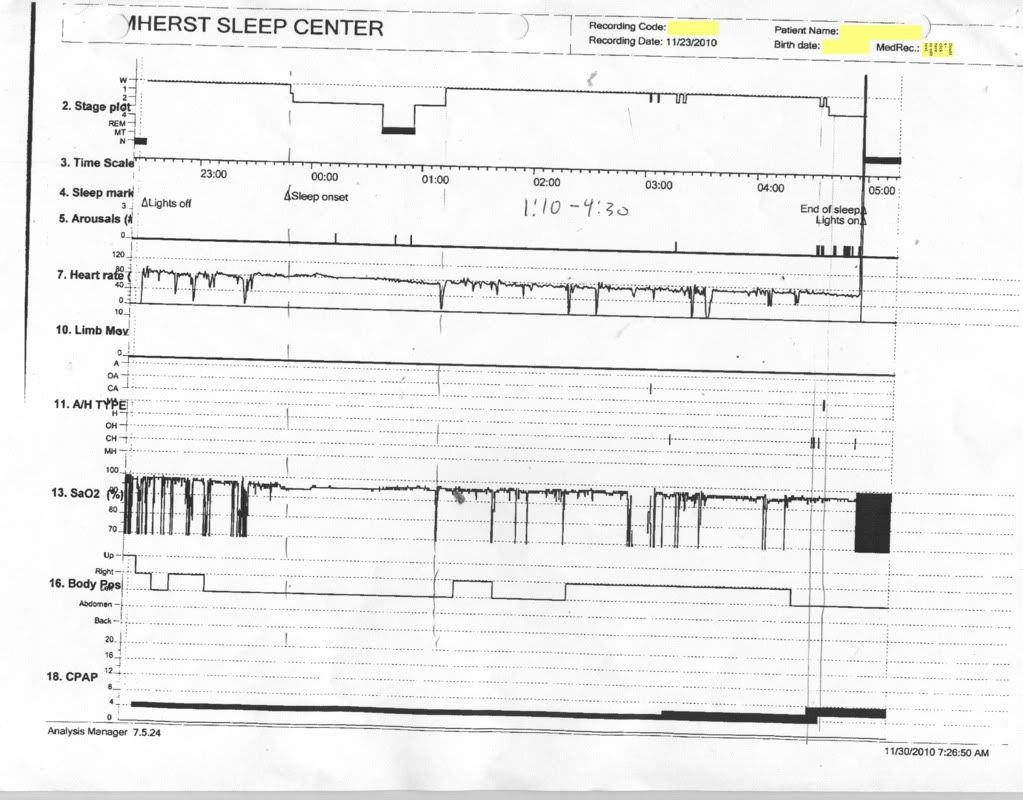
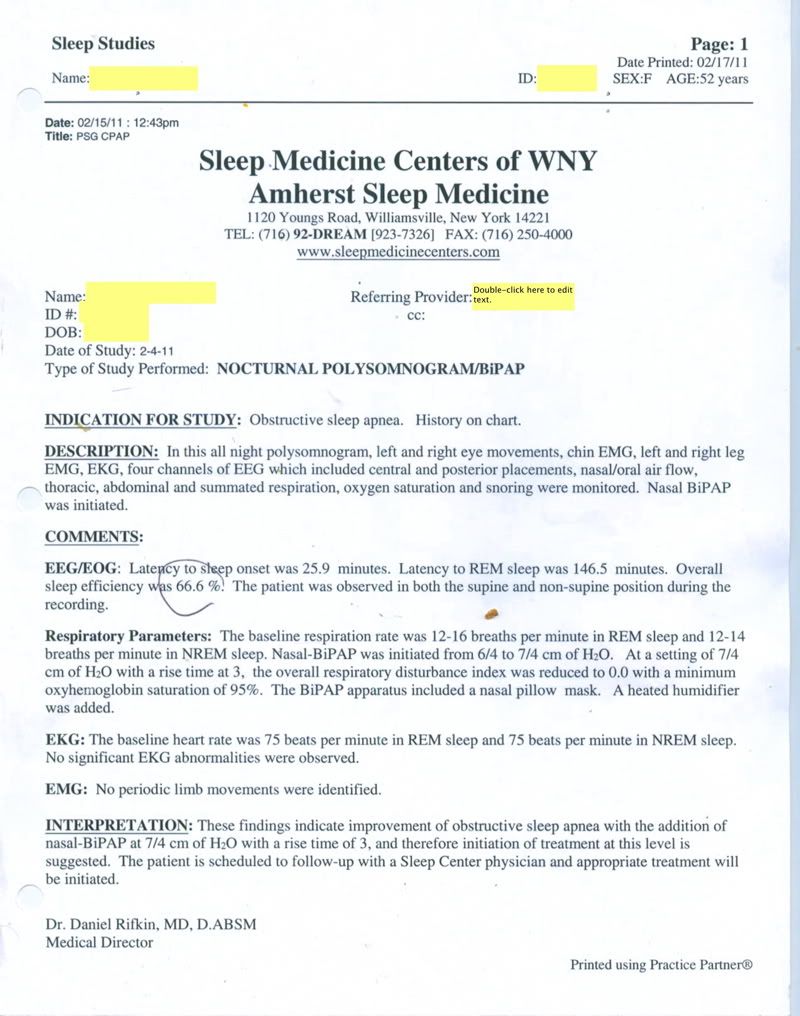
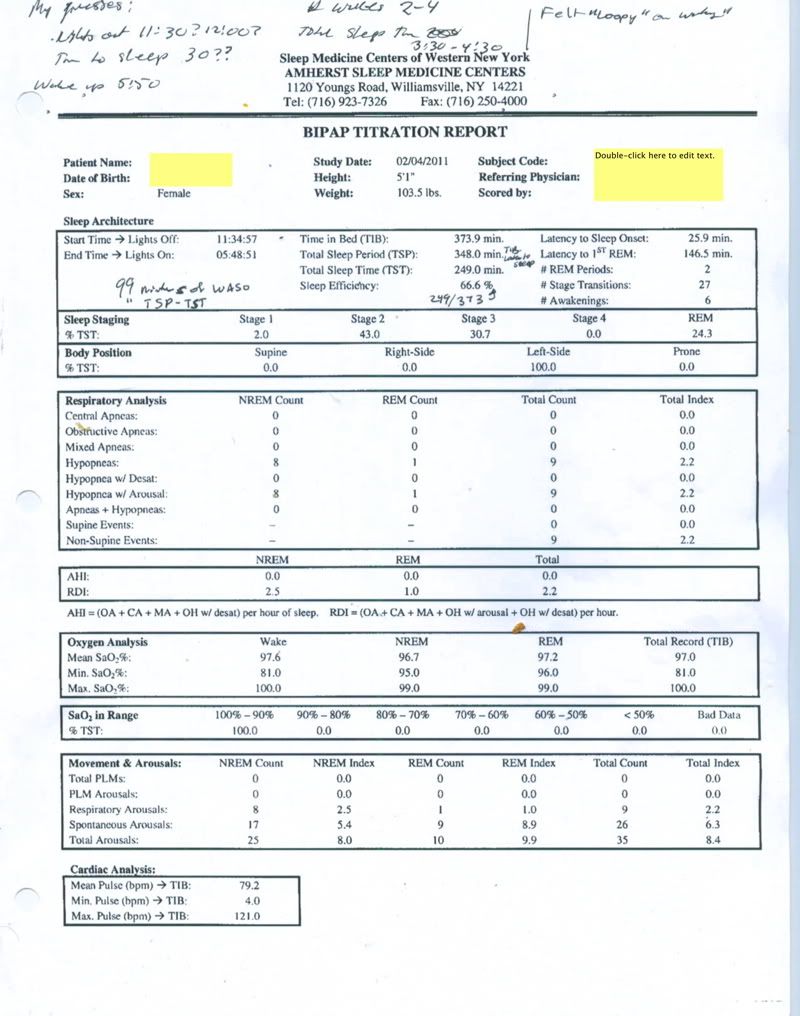
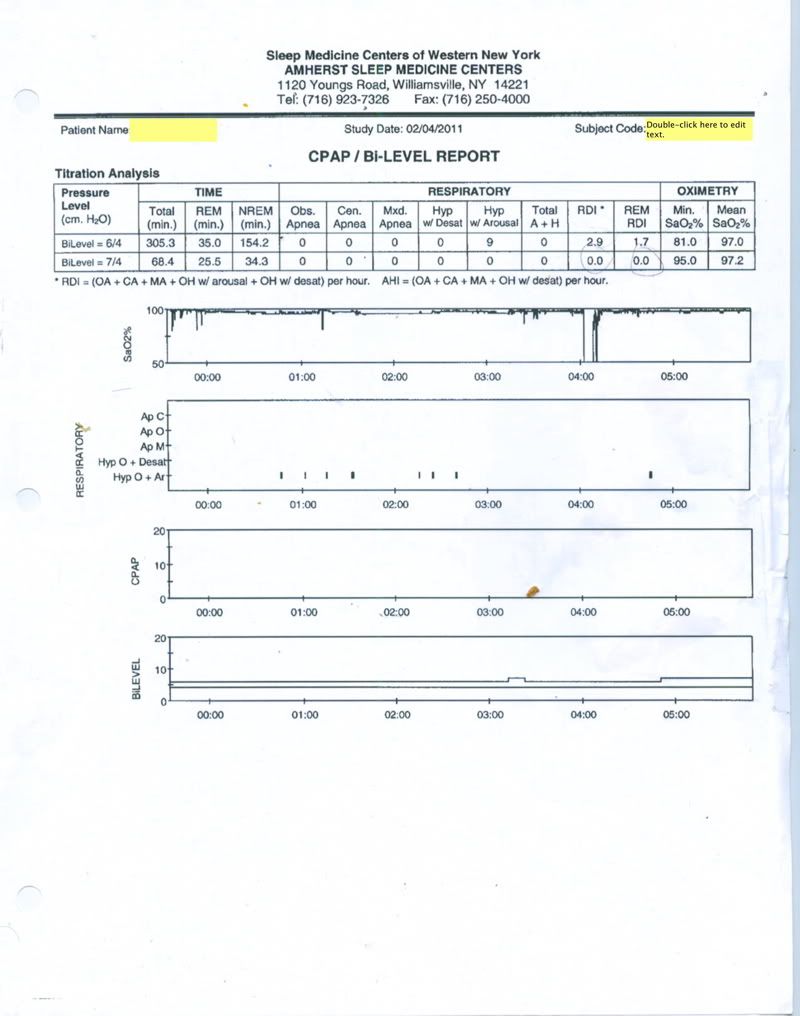
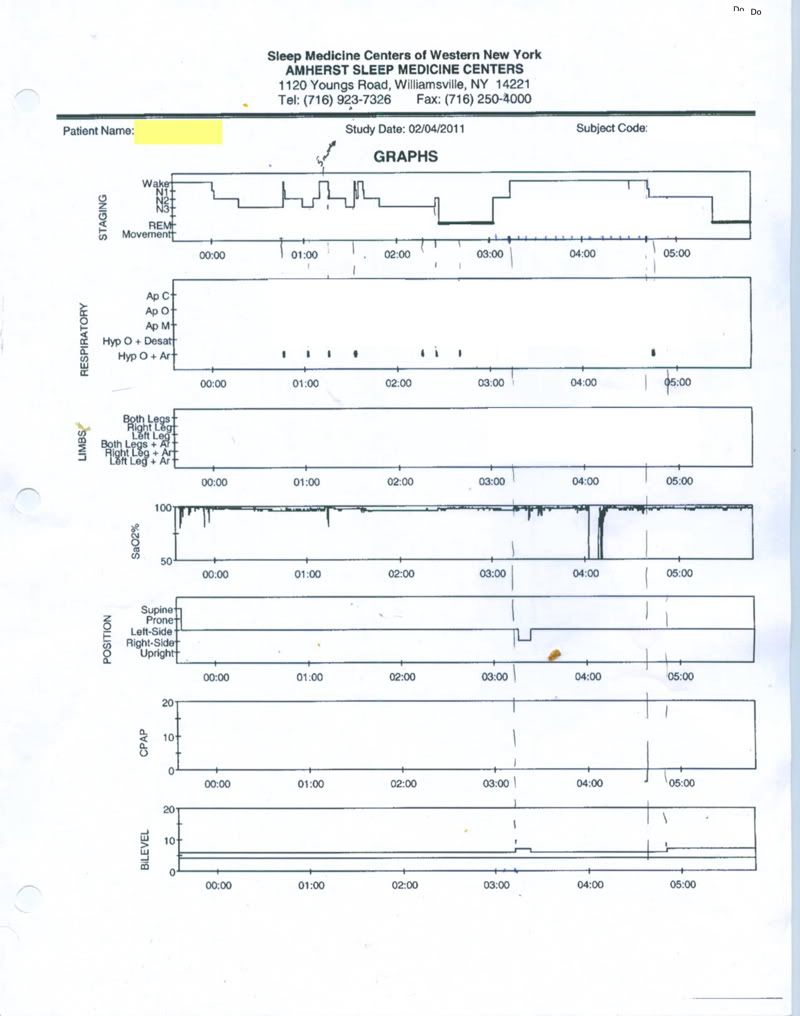
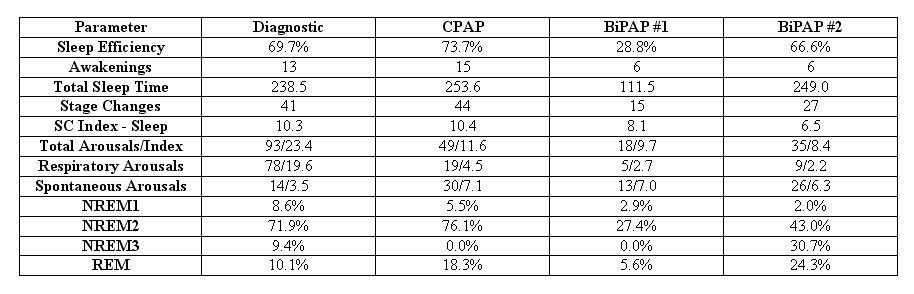
The change to BiPAP seemed to make major progress towards my getting used to actually sleeping with the hose---as the stage 3 and REM percentages in that Feb. 4 titration study show.
By the END of January and beginning of February
At the time of the second bi-level titration study, the answer to "What exactly do you hope to accomplish?" had definitely started to change to:
- Live longer and stay healthy longer AND feel better NOW in some subtle, but important ways!
Where did this change in my goal come from? Well by late January, as the worst of the crash and burn symptoms began to lift with the positive work on taming the insomnia monster, a subtle,
unexpected, but important shift started to occur in the sleep logs I was keeping as part of the war on insomnia:
The low grade, but almost constant pain in my hands and feet had all but disappeared! And on some mornings I was waking up with significantly less headache pain. Now you have to understand: Back before CPAP, the hand/foot pain had been around for several years---I'd even had an x-ray or two done to confirm low grade, minor arthritis in my hands and feet. PCP said it was nothing to worry about and to simply take OTC ibuprofen when the pain was really bothersome. [Such as when cold wet weather aggravated it.]
And as for my long, long history of headache pain: Was is a daytime symptom of OSA that I didn't recognize because it was just my normal "I feel OK but not great" way of dealing with it or something else? I don't know. And I suspect the answer is complex: From the time I was a small child, I've had headaches---and of numerous types and kinds. Like many a chronic headache sufferer, I can describe subtle differences in different types of headaches and even describe a particular headache in terms of different sub-types.
Migraines are clearly one of my well defined headaches: I was officially diagnosed with migraines back in my twenties when I had a classic "migraine with full aura" standing at the kitchen sink one sunny afternoon. And there is a strong family history of them. Moreover the topamax and lamictral both reduced the frequency and intensity of my (almost) daily headaches. But the side affects of these medications were not tolerable.
Sinus headaches in spring, summer, and fall have always been issues. The pollen filter helped alleviate some of my fall ragweed symptoms last fall, but the cost (in terms of Crash and Burn) was not worth it. And at this point, there's the nagging question of "how much pressure" do I need to deal with the sinus congestion that seems to be driving up the snoring (increasing the EPAP and IPAP both) and for all I know increasing the A's in the AHI's.
Tension headaches are an almost constant companion when I'm under stress. To the point where the neurologist's PA thinks they are actually migraines in disguise.
Food headaches, needing to drink water headaches, out in the sun too long headaches, noise-triggered headaches, and yes, "I can't sleep headaches" have all been part of my daily life. So it's not at all unreasonable to assume some of these headaches were related to the untreated OSA. And while I cannot say that using the BiPAP has eliminated any headaches, I can at this point say that by the end of January, throughout most of February, and during the first half of March, I had started waking up head ache free once or twice a week.
And at PRESENT?
And how do I answer "What exactly do you hope to accomplish?"
TODAY? Well it's definitely a combination of:
- (Feel better NOW with Sleeping better as a subset of (Feeling better NOW)) and (Live longer and stay healthy longer)
where the change in order and the parentheses are both important in establishing my meaning. And by
Feel better NOW, I mean the following:
- No more joint pain in the hands and feet. This has been an unexpected blessing that I genuinely can't attribute to anything BUT the use of CPAP/BiPAP. As my PA has explained it to me, OSA can apparently cause low grade inflammation throughout the body. And that, of course, can easily show up as joint pain. And I've done absolutely NOTHING to expressly address the hand and foot pain since starting xPAP. Ergo, it is quite reasonable to credit the use of xPAP with the reduction (rather---the near elimination) of my day-to-day joint pain. And the reduction in joint pain is well worth the hassle of using the BiPAP as long as the stomach problems don't become more painful than the joint pain was and the insomnia can be tamed. But alas, as spring allergies kick in, the joint pain may be coming back. I wonder if it's a hystamine related thing: The allergies trigger a hystamine reaction. Does the hystamine reaction increase the inflammation? And is the increase in inflammation leading to the seeming need for an increase in EPAP, which is so problematic for my stomach?
Some headache relief. I don't expect xPAP to be a magic bullet for my headaches. But there had been a reduction in them during Februrary. It's too hard to tease out what is migraine and what is OSA for me to know anything yet though. And with the change to depakote, the headaches are returning. The vertigo less so, but there's also been an uptick in that too. *sigh*
Sleeping (much) better now than I was last fall and (subjectively) sleeping at least as well as I did pre-CPAP. My goal for sleeping better now is twofold and hopefully modest in expectations: (1) Making sure the BiPAP does not interfere with taming the insomnia beast (so far so good, except for stomach problems) and (2) hoping the BiPAP will continue to help me get more restful sleep---in the sense of not kicking the covers off, not whacking my husband quite so often, not turning over in bed so frequently, not waking my husband up with my snoring, as well as in the more traditional sense of waking up feeling reasonably rested and willing to get up and (sometimes) face the day with the aid of coffee. As the insomnia resolves itself, I am finding that the best mornings now are definitely a bit better than the best days pre-CPAP in terms of waking up feeling refreshed and rested. There's just not enough of them (yet) and I'm greedy. The way I *feel* on one of the average mornings now is pretty definitely about the same as the way I felt on the average so-so mornings I had for the last three or four years pre-CPAP. Subjectively, if those best mornings were to increase in frequency they'd make xPAP worth it. But at their present level, I'm not sure I've reached the break even point yet.
Functioning in the daytime once again at pre-CPAP levels. I want to be able to once again get up in the morning and by the time I finish breakfast be able to concentrate on teaching, grading, committee meetings, etc. without falling asleep or feeling like I'm going to falling asleep. I want to find my once superb memory for details and the ability to manage a complex calendar for the whole family instead of struggling just to keep my own commitments straight. I want to have the energy to recover my not very high level of organization that went AWOL last fall and in the process find the floor to my office. Not yet there. And seeming no progress in site. Maybe there will be some progress once I'm sleeping longer, I don't know.
My current frustration is that the
Feel better NOW end of things has hit a "one step backwards" stage I think. I know I just need to work my way through it but still, that is part of the current angst. And I try to remind myself that this too shall pass. But in the meantime, the combination of (migraine, vertigo, lack of sleep, an unresolved anger/angst) makes for a potent and negative mixture to deal with on a weekend. Fortunately, things seem to be much better today.