I simply could NOT tolerate 9cm of pressure: Air was getting into my eyes through the tear ducts, aerophagia with a rock hard stomach was the norm (and waking me up at night), and my daytime functioning went from NORMAL to BASKETCASE within one week of trying to sleep with a pressure at 9cm. As one indication of how bad things were: My score on the Epworth sleepiness scale went from 3 or 4 (pre-CPAP) to 14 or 15 after a week of trying to sleep with the pressure set at 9cm.JDS74 wrote:RobySue:
What an extraordinary set of data on your apnea travels.
A couple of questions:
During one of your titrations, the OSA's were completely suppressed at 9 cmH20 but not below.
Your current settings have IPAP Max at 8.
How did that happen?
By the end of week 2, the PA had me start a week or two of APAP with the range wide open: 90% pressure level came in somewhere between 7.5 and 8cm, (with the 50% level between 4 and 5cm if I recall correctly.) So the PA ordered a formal reduction in pressure and a switch to APAP with a range of 4cm to 8cm. AHI increased marginally from 0.5ish at 9.0cm to 1.0--1.5ish. Aerophagia issues continued, but the rock hard stomach problem was not quite as bad. Air in the eyes largely went a way. Daytime functioning continued to deteriorate.
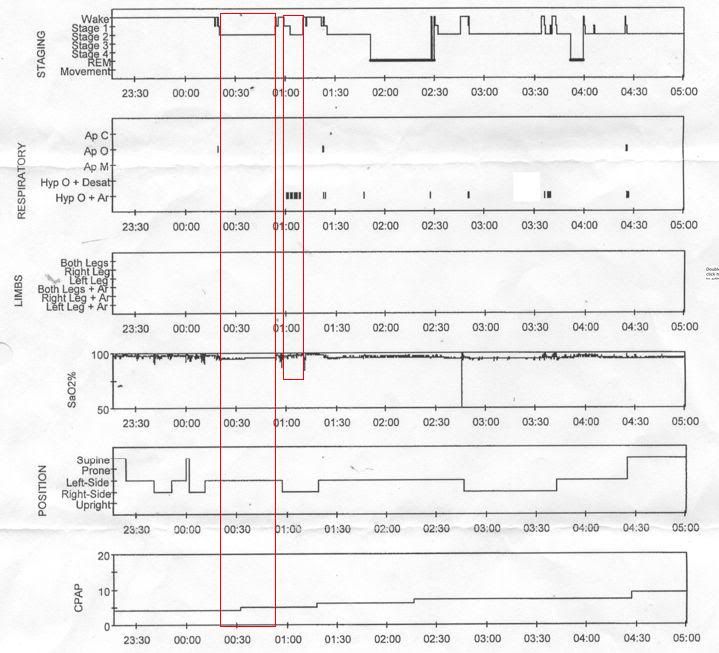
By the end of another three weeks, my daytime functioning was still deteriorating and I was having occasional nights with clusters of events and the overnight AHI were starting to bounce around some. The PA suggested the switch to bi-level and the first titration was done. Even with the flawed study (due to the insomnia), both I and the PA thought the switch would be reasonable. Best guess for titration level was 8/6 coming out of that study. By the time I got the BiPAP, the war on the insomnia had been declared and I was asked to keep a journal. AHI's with the BiPAP at 8/6 were running between 0.5 and 1.5 most nights with the occasional outliers in both directions. In the journal, it was clear that aerophagia was one of the things waking me up at nights and also making it more difficult to get back to sleep. So the PA suggested another titration study, the last one done in February. On that study, the final pressure was 7/4 and that's what the PA changed my pressure to in an effort to help the stomach cope better and help me sleep better (insomnia wise). Things were going ok (although the AHI had crept up more to 1.0 to 2.0 most nights) UNTIL the trees started pollinating and my spring allergies kickeed in. And that's when the last set of clustering of events started. As well as several nights with an AHI of 2.5 -- 3.0, with two nights in a row where the AHI was 4.+.
At which point the PA suggested switching to Auto BiPAP with my current settings. And AHIs have run from 0.5 to 2.8. My concern is that when they get on the high side of 1.5, there is usually some nasty clusters of events with as many six to eight events in a short period of time. Most days, the AHI is less than 1.5. But the day I posted thread that lead to this one, Wallowing in self pity , my overnight AHI was 2.8, there was a cluster of something like 8 events in a 30 or 40 minute period if I recall; I woke up with a migraine in the morning (and yes, I know it was a migraine since I'd woken up with the migraine aura at night); and the good sleep efficiency on the insomnia was just not enough to overcome everything else in terms of how I felt that day.
My stomach will NOT tolerate this much pressure 100% of the time without seriously aggravating the insomnia. Moreover, I have only just begun to recover from the serious crash-and-burn in daytime functioning last fall. Increasing the EPAP will likely re-create some of the same circumstances that led to my daytime problems last fall. I have thought about and talked to Keryn, my PA, about possibly going back to straight BiPAP set at 8/4 or 8/5 to see if either of these would be better (in the sense of how I feel) than my current settings. But right now there's just a bit too much going on with the insomnia and spring allergies to throw in yet another change just yet. Once I succeed in getting my sleep restricted bedtime moved from 1:30AM to 1:15AM, I may play more with the settings.Have you experimented with raising the EPAP Min up to 7 or 8 cmH20 to see what happens in the data?
Looking at a clock for establishing time of wakes is discouraged by my PA since the point of the journal is fighting the insomnia and looking at clocks tends to focus the insomniac's mind on how little sleep he/she is getting. So there is no clock visible from my side of the bed.Second, You mention a sleep diary or journal. Are you recording the times you wake up at night and correlating those times with events in your data? I found that I now have clusters of CSA's and that they correlate almost perfectly with times I wake during the night. What wakes me up are episodes of headache, a feeling of being hot, and sweating profusely. Can you identify any set of circumstances that are associated with waking up?
But---the journal is chock full of what I remember about the wakes. And prior to the reduction of pressure from 8/6 to 7/4, the number one most common why I woke up was aerophagia. Sometimes it would trigger three quarters of the total wakes. And these wakes also tended to be the ones that took a while to get back to sleep. Hence the last titration study. And once the pressure was reduced, aerophagia dropped off the list of what was triggering wakes. And stayed off the list until the switch to BiPAP Auto was made.
As for now, what pops up most often in the journal on what's waking me up is congestion, with runners up being rainout, chapped lips, active mind (possibly dreaming), aerophagia (since starting Auto BIPAP), being hot or cold, and sometimes headaches---but more often migraine aura than pain. Sweating profusely is not unheard of, but is not that common either. Sometimes the sweating is easy to attribute to our not great heater overshooting the morning heat setting and both my husband and I wake up sweating in a hot room. I can say that I'm no more prone to waking up with known apnea symptoms on the nights that I have the clusters---with the exception of a general "bleh" feeling in the morning and an increase in my "background" headache level. At no time on CPAP have I been headache free. As I stated in an earlier post in this thread, a month ago (pre spring allergies), I had started having one or two headache free mornings a week. And that may represent a major plus for xPAP. But there is also ample evidence that the migraine prophylactic I was taking at the time may have been much more effectively managing the headaches than what I am on now. Alas, I could not tolerate the other medicine's side effects.
Back when my pressure was still at 8/6 and aerophagia was a huge nighttime issue, my tendency to hit the ramp (to help the stomach) made it easy to figure out when the wake happened since my ramp went from 7/5 to 8/6 in about 30 minutes. So the ramp period was easy to see in Encore Viewer. But the "ramp" is disabled when EPAP = 4 and turning the machine off and then on is not visible in Encore Veiwer unless the off/on cycle is a minute or two in length. But I don't want to leave the machine off for two or three minutes every time I wake up: I just want to make a mental note of the wake and turn over and work immediately on getting back to sleep.
Leaks have never been a problem for me. Nice flat leak line at or below the expected leak rate in Encore Viewer night after night. With one exception: When I go to bed with a migraine, I have to set the straps on my FX ridiculously loose and I typically get one "Big bump" leak those nights. But on average, I get a "Big Bump" night maybe once or twice a month. And the biggest consequence of "Big bump" nights is very badly chapped lips, which can both wake me up that night and make it much harder to get to sleep on subsequent nights.Third, Are you having any problems with your mask? Leaks, fitting discomfort?
I agree sleep hygiene is critical: I gave up reading in bed some twenty-five to thirty years ago in some long forgotten bout with insomnia back in grad school. When hubby moved a tv into the bedroom several years ago, I threw it back out. In the past, I've always been able to tame my insomnia in the past by paying a bit more attention to my overall pretty good sleep hygiene. But this CPAP-induced/enhanced insomnia is far more entrenched than any insomnia monster I've ever had to fight in the past. And I've been working with my PA on an intensive behavior therapy approach to treating my CPAP-induced insomnia since Dec. 30. The PA has been absolutely great.Fourth, You mention episodes of insomnia. I find that I need to have a rigorous schedule for sleep preparation to avoid that. NO reading in bed, NO TV in bed. When I go to bed, it's for sleeping. Perhaps another closer look at sleep hygene will reveal some detail that will correlate with the insomnia.
For what it's worth, here's a basic description of what Keryn, the PA, has had me doing since Dec. 30: First Keryn had me move the "no caffeine after lunch" to the more stingent "no caffeine after 10 AM". And no alcohol during the evening obviously. Try to get outside in the morning. And get some exercise every day if possible, but not too late. Small supper (for the aerophagia), but don't starve myself either. Keep the sleep journal. And make the clock not visible from the bed. But the most critical aspect of the therapy has been designed to force me into getting serious about the need for a rigorous wake up/bedtime schedule. And right now, my wake up/bedtime schedule also involves intentional sleep restriction: I got to select my wake up time for seven days a week that would work for my spring schedule. I chose 7:30AM. Keryn then informed me that my bedtime was the later of 1:30AM or when I first get sleepy after 1:30: I am not allowed to spend more than six hours in bed each night. I also have to get back out of bed if I find myself angry or upset about anything related to the BiPAP machine. Or if I can't get to sleep in what I think is about 30 minutes. Or if I wake up WIDE AWAKE and find that I can't get back to sleep in a timely fashion.
The idea is to help me consolidate my sleep cycles and increase my sleep efficiency, which is defined as:
- sleep efficiency = (time asleep)/(time in bed)