One of the key factors for me is that I do not have health insurance and have to pay every for everything out of pocket for both the heart condition and the sleep apnea—and my finances are currently somewhat limited. Because of this I have been working with a local county hospital which is a training hospital for a major university. As such the standard of care is supposed to be of average as hospitals go, but the care is hardly personal and takes forever. (I have managed to get two sleep studies by being proactive and by filling in for other’s cancellations.)
I basically diagnosed myself with SA and then had to suggest to my cardiologist that a referral for SA apnea might be appropriate (he agreed). That was in April and if I had waited for the sleep lab it would be September before anything would have happened. And the one sleep “Fellow” I have seen personally didn’t even know that positions like back sleeping can worsen SA. Also the main sleep lab nurse said they are happy is they can get a patient’s AHI to 9. And after the first sleep study the main doctor basically said just go deal with the heart condition first until I talked them into ordering the titration study. I mention these things because I don’t expect a lot of help from the hospital and it seems that I am largely on my own except for the help of this forum.
(History and sleep study reports can be skipped by going to post #2 about 3/4 down this page.)
History:
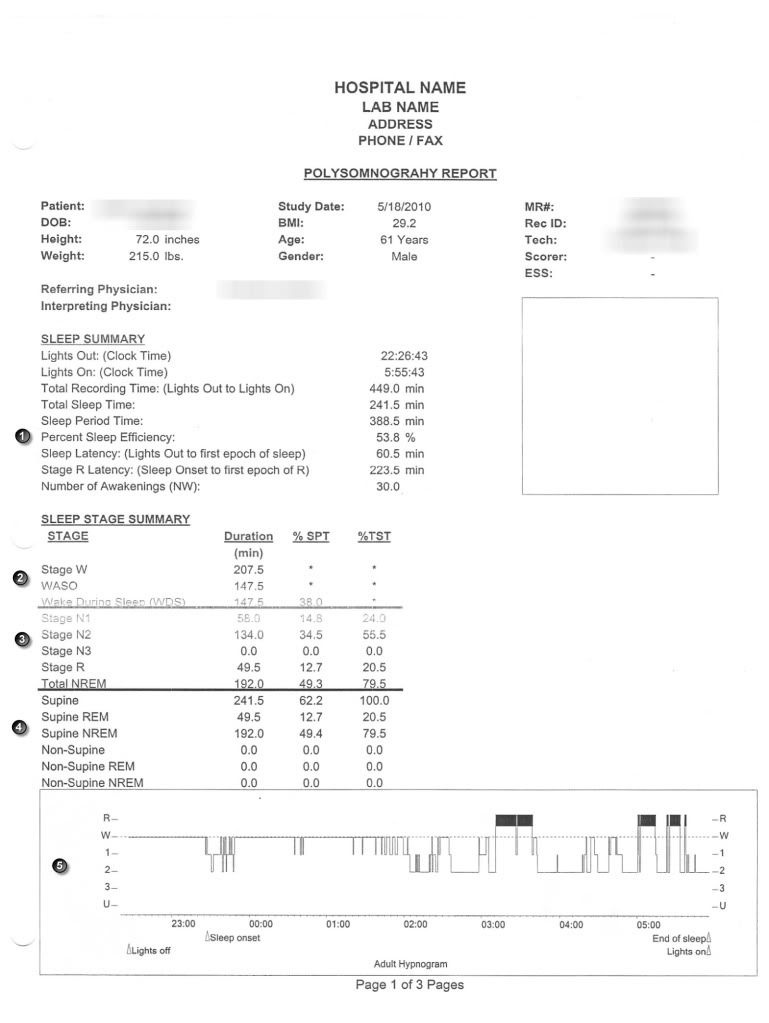
I am a male 61 years old. I am about 30 lbs overweight (6'0" 214 lbs) with a BMI of 29-30.
For the past 7 years 24/7/365 I have had atrial fibrillation with a heart rate that varies rapidly between 65-180bpm (and all points in between) averaging out to about 110 bpm. Over the 7 years this has resulted in a left ventricular ejection fraction of 20-25% which was described to me as being as low as could be measured and this means I am going into heart failure. This results in the CSR. The heart arrhythmia has greatly contributed to insomnia and disturbed sleep, which is probably the greatest debility I've had from the heart condition. I monitor my HR frequently at home with an EKG machine.
I get some shortness of breath on going up stairs and have very mild ankle edema. Now that I am getting some help from the S9 I am functioning pretty well. My data and tests look pretty bad, but most folks are surprised to hear that I have any health issue at all and say I look quite healthy. I believe this has sometimes worked against me, especially with the sleep doc, as they look at me, think I look far better than many of their patients and so minimize my case.
I have also developed mild primary hypothyroidism. And I’ve had gout, which has abated tremendously since treating the SA.
Equipment:
ResMed S9 AutoSet II with H5i humidifier and Climateline hose (Currently I don’t use the H5i.)
Mirage Quattro medium full face mask. Pad-a-Cheek anti-leak strap that I don’t currently use.
ResScan 3.11
Respironics BiPAP autoSV (original model) I own this but have not used it yet.
ResMed VPAP Adapt SV (original model) I have this on loan from a very kind gentleman, but I can purchase this if I can get it to work for me. I tried it for 3-4 days but did not do well with it.
Software: ResScan 3.11 (only used for the S9 so far. I’ve had trouble getting the cable set up to work for downloading data from the Adapt SV
Encore Pro 2.3 (don’t yet have the card reader for downloading data)
Oximeter CMS 50F
Alternating pressure medical air mattress (helps tremendously with pressure points from sleeping restricted to side sleeping)
EKG machine.
Sleep Study I
I was less than thrilled with my initial sleep study for several reasons. First as they told me they wanted to get a couple of hours of me on my back, I tried to sleep in that position. It probably took me 4 hours or so to drop off and then really only dosed fitfully.
Also the tech saw the Cheyne-Stokes respiration and he also told me my SpO2 was about 96% so he did not bother to hook me up to a CPAP machine and ended the session an hour early. I feel he (and later the respiratory MD who read the study) just assumed this was a central apnea secondary to the heart arrhythmia Basically the respiratory MD said there is no point in treating for SA unless the arrhythmia is handled. (The MD backed off on this when I brought in information about the Adapt SV helping to improve left ventricular function and the fact I’d obtain the machine.)
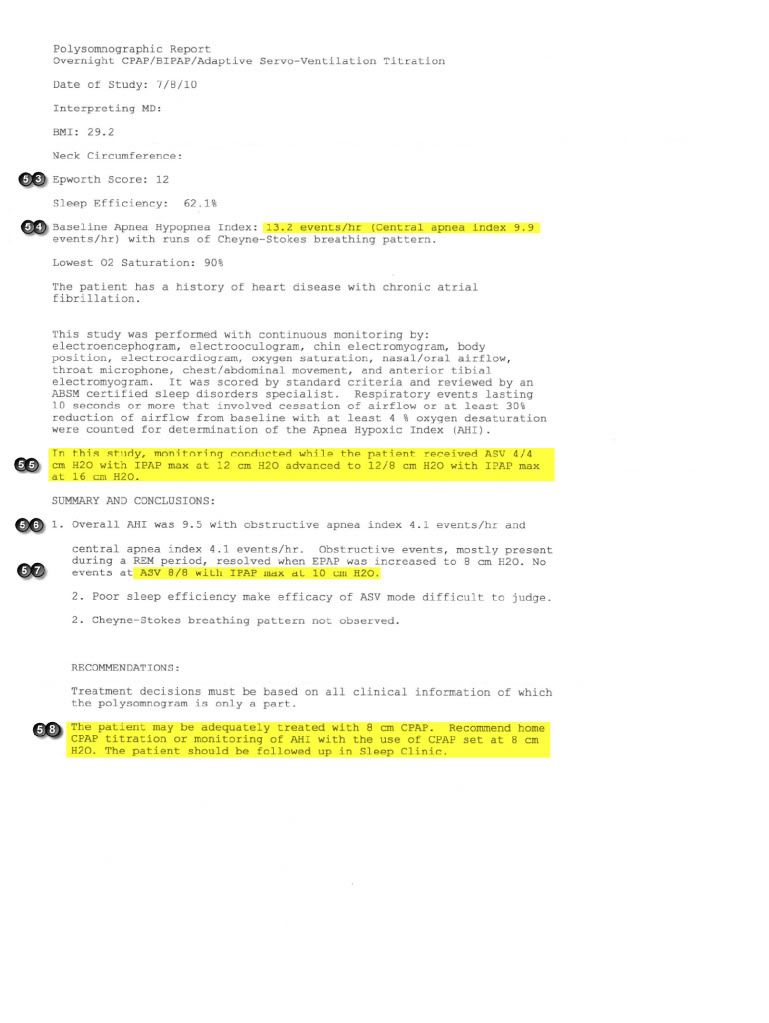
Sleep Study II Titration Study
Titration done with Respironics Omni-lab machine.
This hospital doesn’t usually do much with ASV titration as they seldom if ever prescribe ASV due to the expense of the machines that they would have to provide to many of their patients. I question (but have no firm opinion) the techs ability/experience with the ASV. They did most of the titration with me sleeping on my back (I know that’s standard procedure)—and I never sleep on my back, although I’d like to.
Apparently they had difficulty titrating me and most of the night was just trying to get the CPAP right. The ASV titration was incomplete due to lack of time. Also the tech said that on the ASV I kept getting Obstructive apneas if the Centrals were decreased. I’ve read about Centrals showing up as OA is controlled, but never the other way around. I was frustrated as the titration was supposed to be specifically to titrate me for the ASV machines that I had obtained, yet so little time went into this.
At the time of the titration study I had been using my S9 consistently for 2 months with a very positive response (according to my symptomatic response supported by the S9 data). So the S9 may have minimized my CSR and confounded the titration to some extent.
Also a couple of times since this study, I have tried CPAP at 8.0 and also the APAP set to range to 7 to 9. During these times the pressure has seemed to be too much and each time my AHI was relatively high for me. And to be fair, I didn't try this multiple days running so maybe I didn't give it long enough.
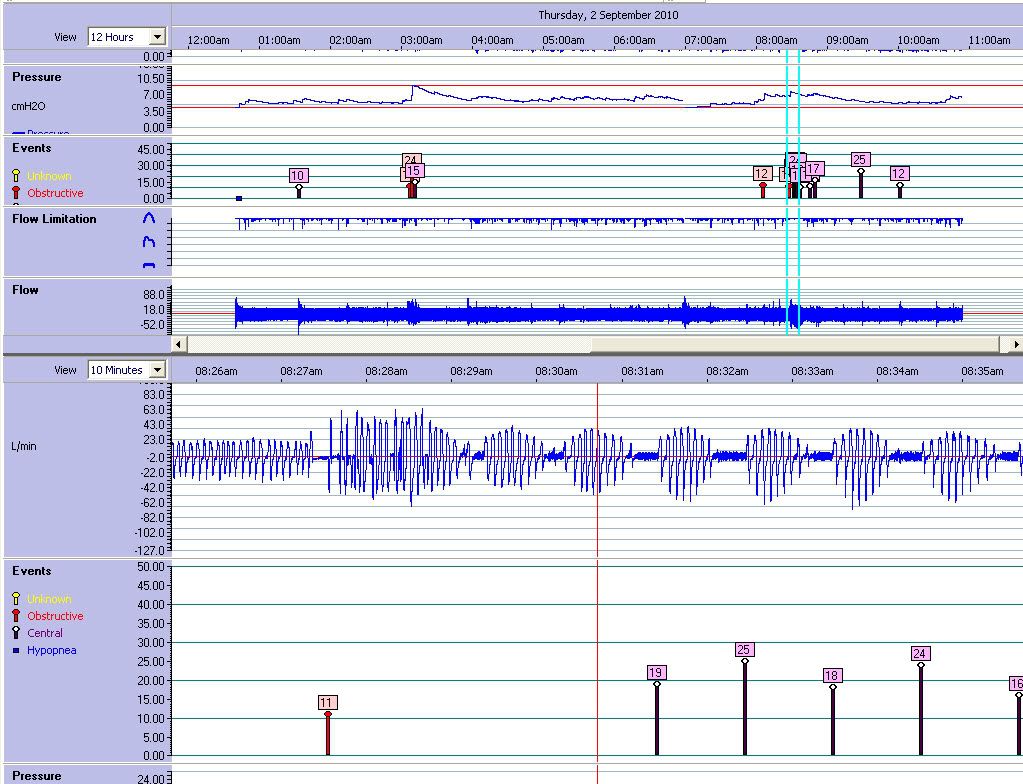
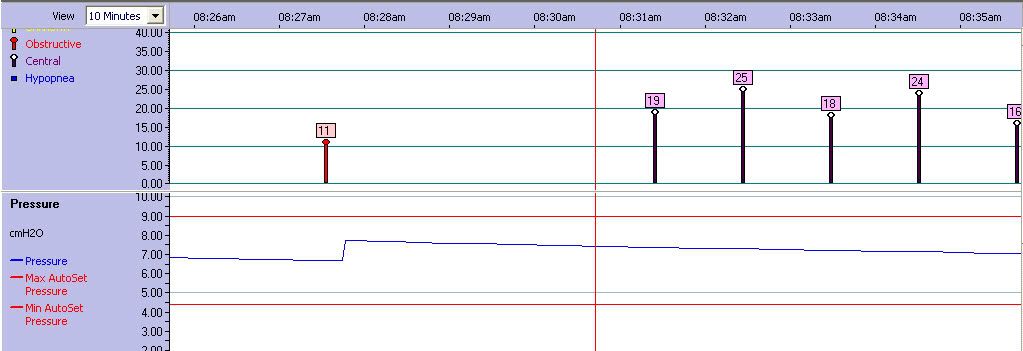
(Note: I have annotated the various screenshots with reference numbers to facilitate identification for questions.)
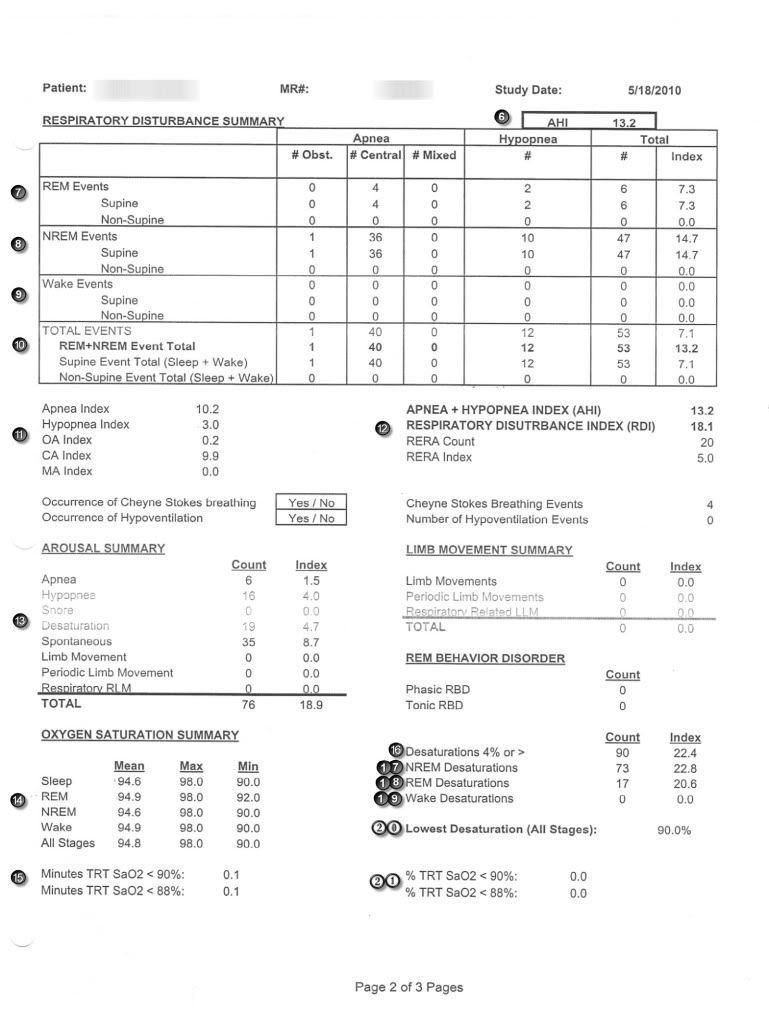
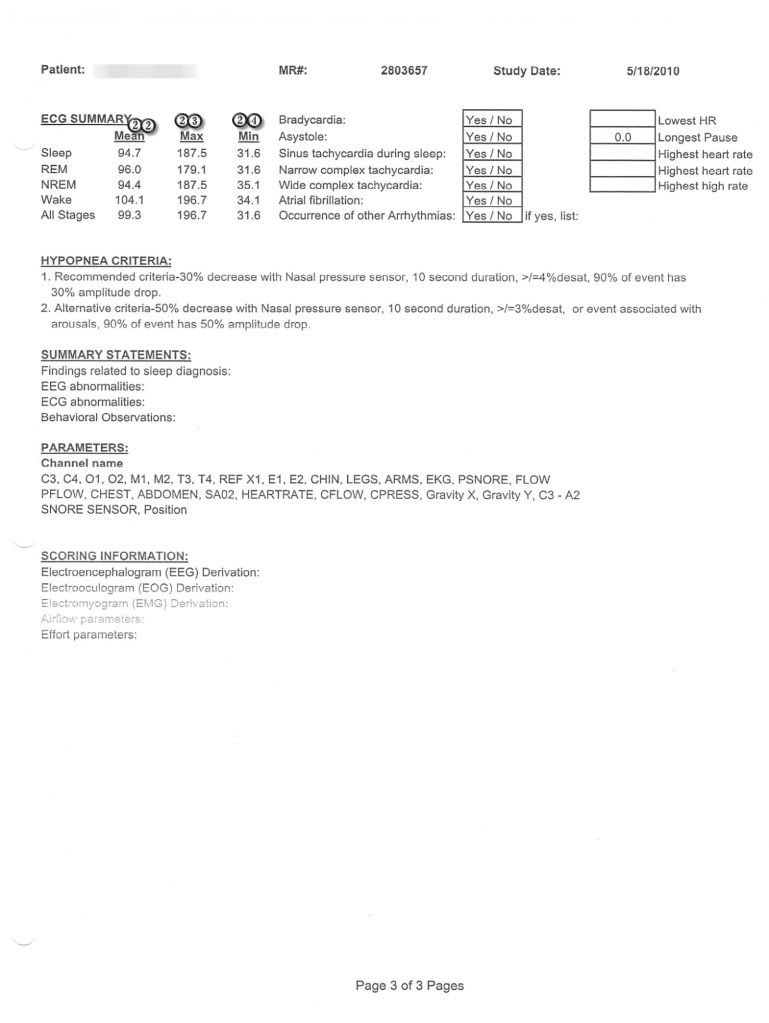
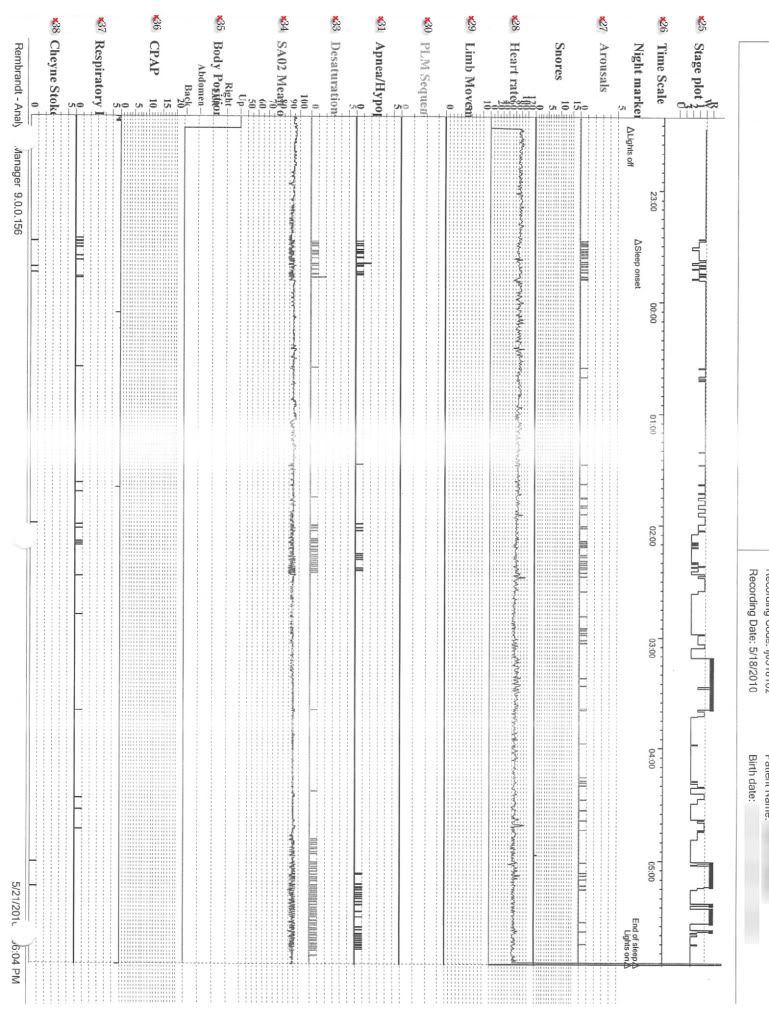
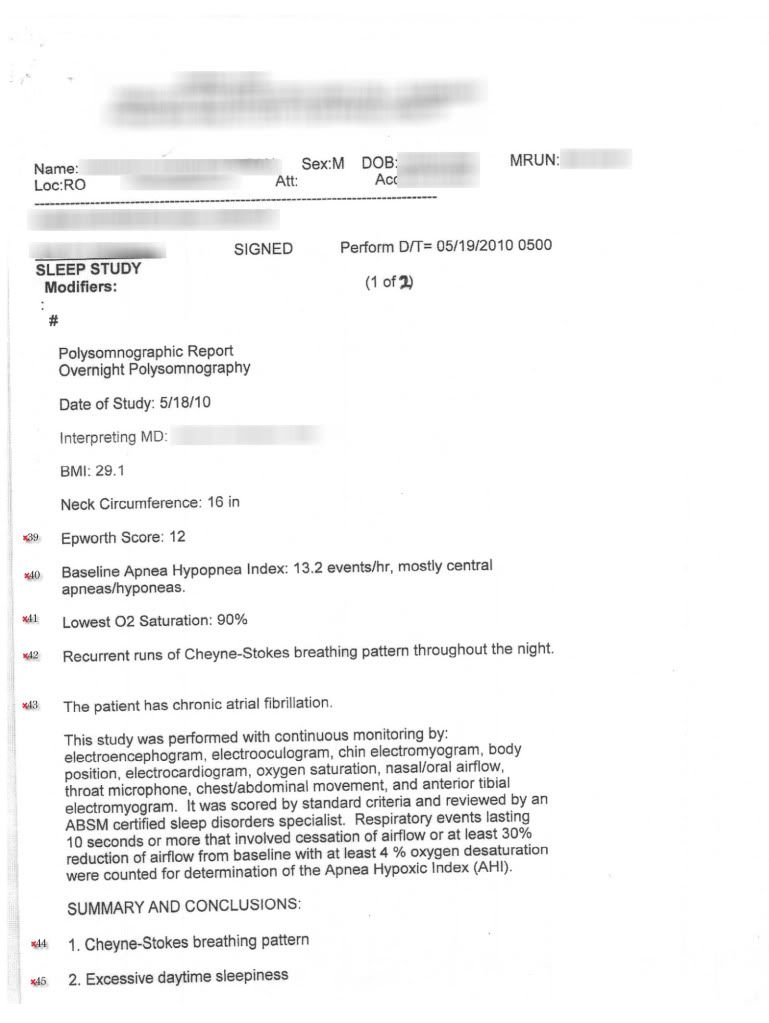
Sleep Study Initial 5/18/2010 (Pages 1-6)
Page 1
Page 2
Page 3
Page 4
Page 5
Page 6
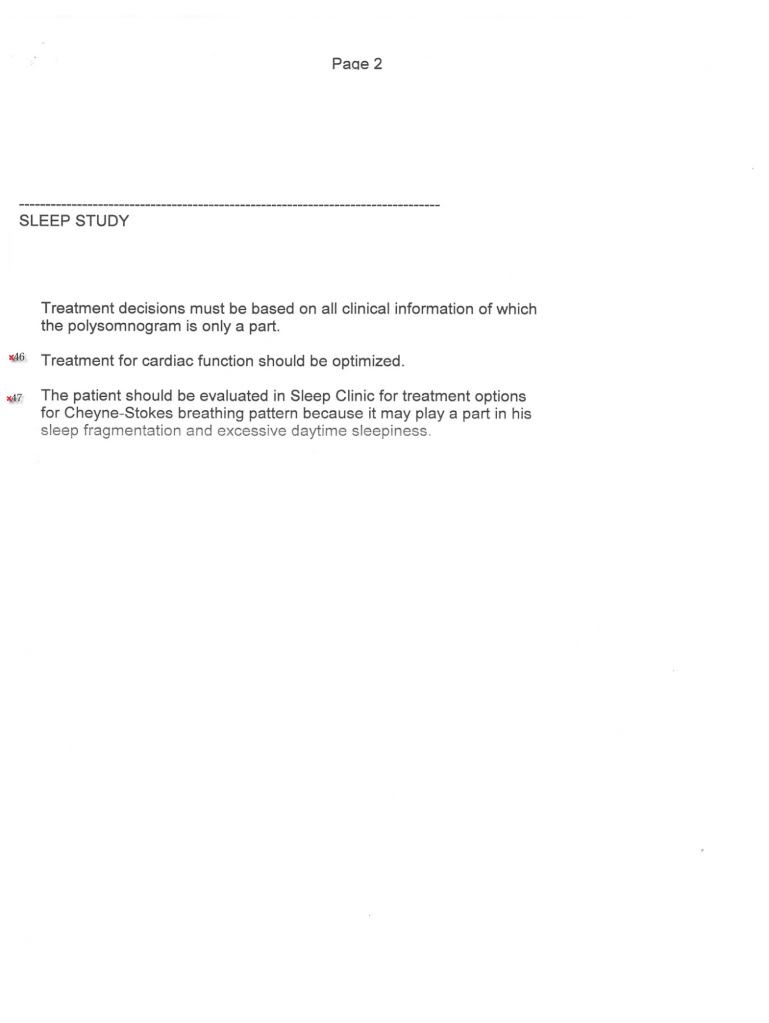
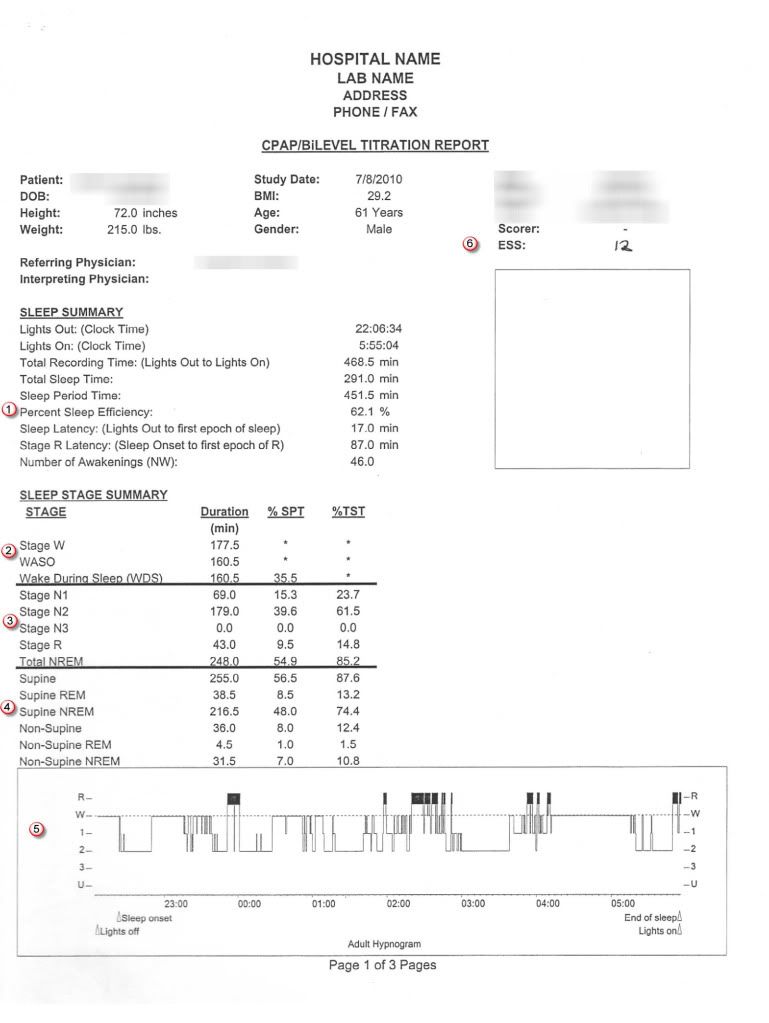
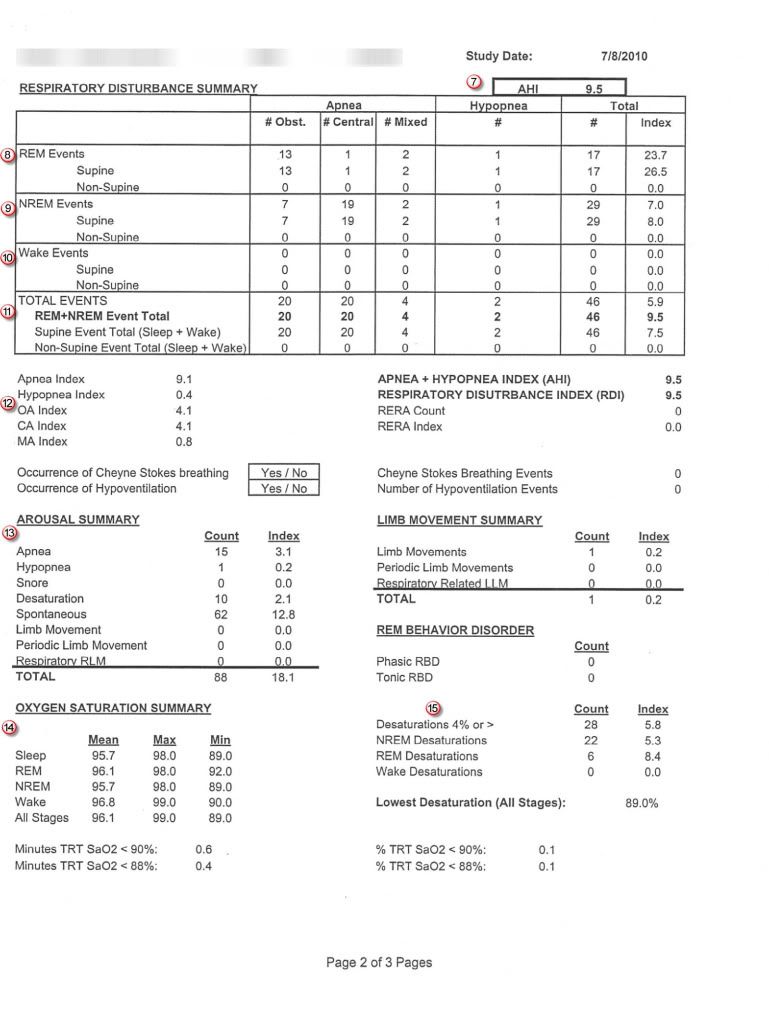
Sleep Study II Titration 07/08/2010 (6 Pages)
Page 1
Page 2
Page 3
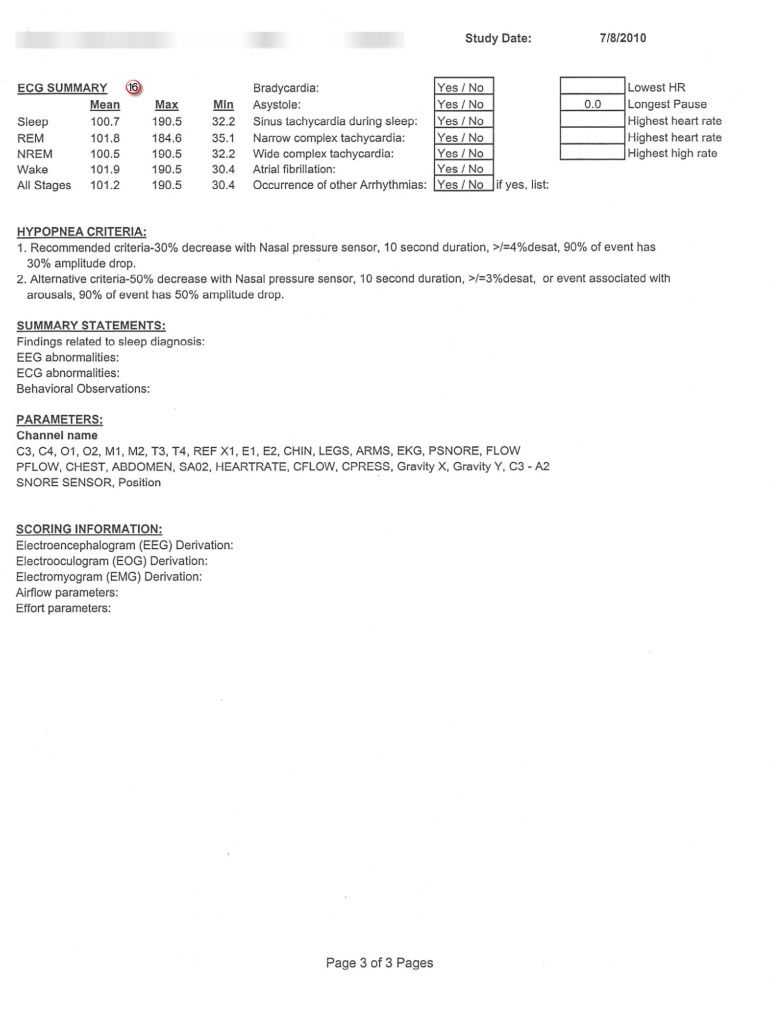
Page 4

Page 5
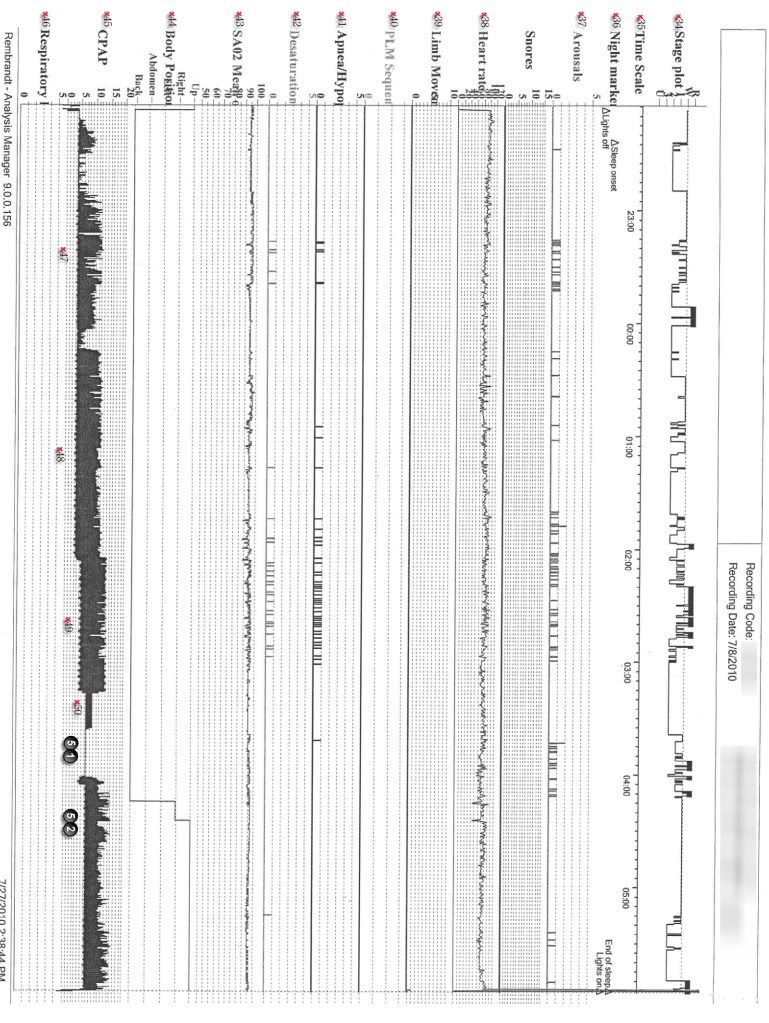
Page 6
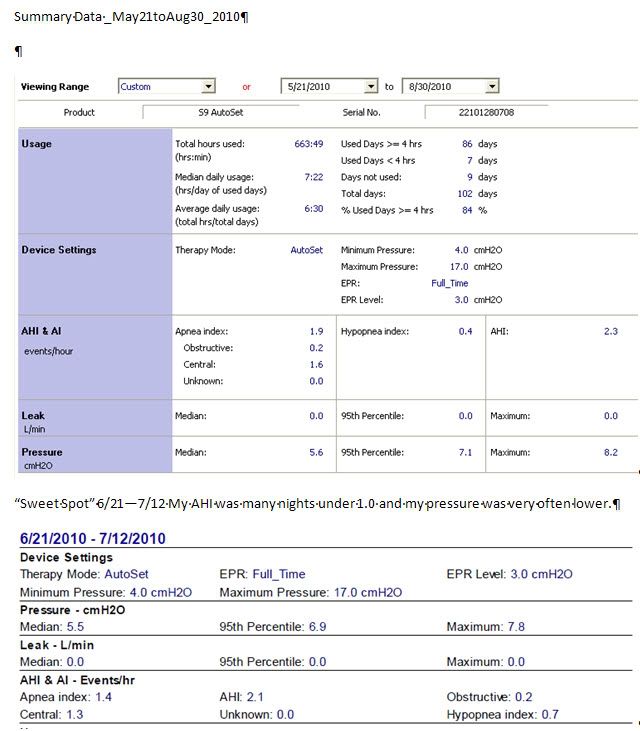
S9 Therapy Response:
Overall, I feel I have had a very positive response to therapy even though the S9 is not supposed to be the best machine for my condition. I am feeling much more rested, don’t get up 4 times a night to urinate, have greater mental clarity and my heart function has improved.
Settings: S9 Settings: Initially I started on autoset 4-20 cmH2O and slowly migrated to my current settings of 4.4-9 cm H2O EPR 3, Ramp None. Over time I’ve watched that I spend a fair amount of time with my pressure under 5.0 and very rarely have gone above 9.0.
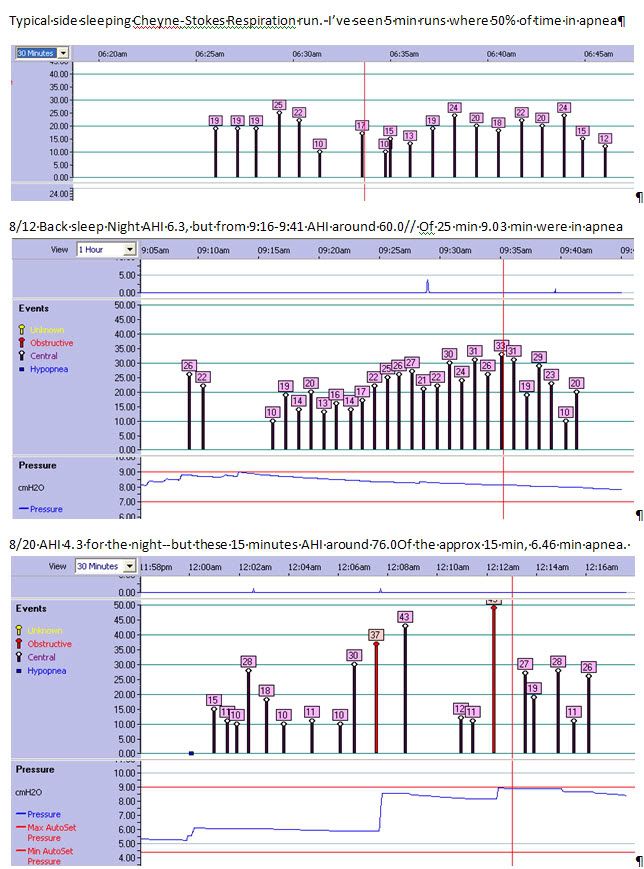
Positional Apnea:
Using the S9 and data reports, I quickly saw how sleeping on my back greatly increased my Centrals. So I very, very seldom have slept on my back since. I have tried a few times to sleep on my back but each time I do I get very high AHI (see example below).
Sleep fragmentation:
Restricting myself to side sleeping only has proved problematic. I get a lot of hip pressure point soreness and pain which results in me waking often many times a night. When I don’t have as much pain I awaken much less. I seldom can sleep without consciously waking for more than about 2-3 hours and sometimes it is every 1 ½ hrs. I’ve lessened, but not eliminated, the pain by getting an alternating pressure medical air mattress.
ResScan Screenshots
But there are still some problems with the S9 therapy, hence my interest in getting titrated with an ASV machine.
Summary Data
Apnea Events Examples: CSR and Back Sleeping
ASV Trial Experience
I did try the Resmed Adapt SV for about 3 or 4 days. I set the minimum pressure as 4.0 (since on the S9 I spent a lot of time at this very low pressure). I set the pressure support minimum to 3 and I think the maximum 10. I believe the rest of the settings were on "Auto". I slept only on my sides for this trial. I did fine with the somewhat odd pressure changes, in fact I fell asleep quite easily. The only immediate problem was some aerophagia that I had never experienced before. And my leaks were well controlled. But I woke up progressively more tired. I seemed to regress and after 3 days it was almost as bad as before I started certainly with the S9 and maybe even the chin strap. It was also very disconcerting to feel so badly and not have any data to provide feedback/calibration. I felt like I was flying blind (especially coming from all the data of the S9/ResScan 3.11. So after these days I discontinued with the Adapt SV and went back to the S9.