On the night of the diagnostic study, the patient's sleep efficiency was low
at 79.8%. The patient had 37 awakenings and 177 arousals. The degree of sleep
fragmentation and disruption of sleep architecture places the patient at risk for
cognitive impairments and metabolic seguelae including hypertension, cardiovascular
disease, diabetes, and the metabolic syndrome.
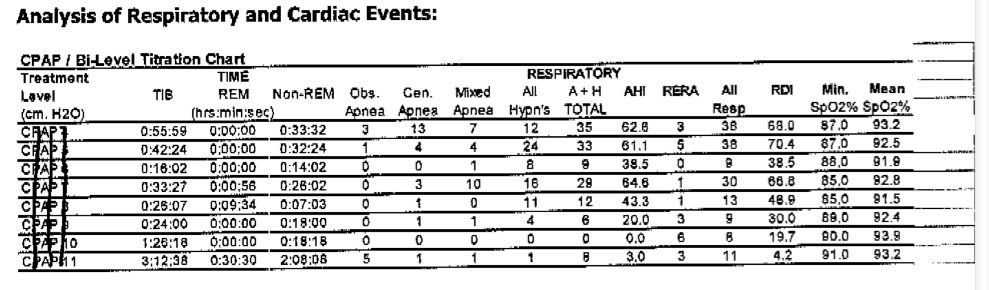
I was prescribed the S9 ASV described below with directions that: "the patient should be maintained on nasal PAP at the final setting of the following: Min PS (Pressure Support) of 3 cm ii20, Max PS of 15 cm H20, and EEP (End Expiratory Pressure) of 5 cm H
the patient should be maintained on nasal PAP at the final setting of the following: Min PS (Pressure Support) of 3 cm H20, Max PS of 15 cm H20, and EEP (End Expiratory Pressure) of 5 cm H2O
The patient should return for download of treatment data every 2. months, etc.
After two weeks on the machine, including a missed night with a very bad cold, I can respectfully submit the following Sleepyhead data thanks to our resident genius Breathe Jimbo!

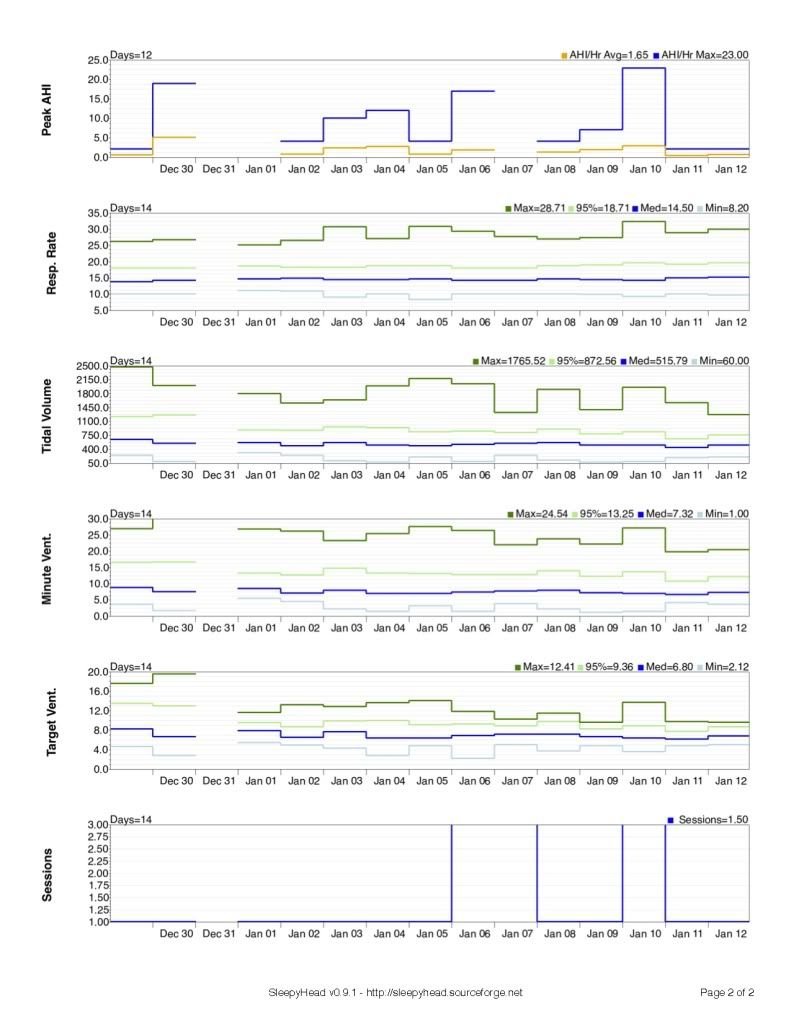
Since this is all new to me, now I would be grateful to hear from our resident experts as to what does this all mean? Should I be happy, discouraged and/or patient with these early results?
Edit/ Forgot the lead page:

Edit 1/14/12 1:36AM to correct "Nocturmal premature ventrical contractions; Nocturmal premature ventrical contractions" to:
"Nocturmal premature ventrical contractions; Nocturmal premature atrial contractions."