Here's the description I can find of your sleep prior to all the beginnings of your sleep troubles
Prior to the onset of the insomina, you had a super-short (as in abnormally short) latency to sleep and a bathroom break, which is exceptionally unusual for a "a 25 year old male, in good shape and [who is] physically active." Those may have been night time symptoms of the UARS and the daytime fatigue in spite of getting 8 hours of seemingly uninterrupted sleep may also have been a symptom of UARS.I am certain that my sleep problems which started literally overnight were not directly caused by UARS, I am sure that I did not develop UARS overnight, UARS just popped up as an issue when I went for an overnight study due to severe insomnia concerns. If anything, those who have UARS usually feel more tired during the day due to long yet unrefreshing sleep, I am thinking back prior to insomnia problem, I always slept for 8 hours and still felt pretty tired at times, and would drop off to sleep within 1 or 2 minutes, never waking up during the night other than my regular bathroom trip around 5-6 am.
That said, let's now turn to the problem you are currently dealing with. You describe your current sleep patterns in this language:
andquitepositive wrote:The problem is that when I use CPAP at home I either cant fall asleep or still wake up several times with it, eventually giving up on it and taking it off. Lately for several past week I have been waking at around 4 am and not being able to fall back asleep for at least 4 times a week, but I do fall asleep faster than before, now takes about 10-20 minutes on average, but the sleep maintenance has gone down the drain.
First and foremost: As tough as it sounds, I think you need to address both the CPAP adjustement and the insomnia at the same time.I am hardly compliant with the machine partly because I already have issues with falling asleep and waking up too many time, and it seems that every time I try to use the machine if I do fall asleep with it for couple hours I am later awakened and cannot fall asleep with it, so I just take it off and continue without it. I still wake up while using it just like I do when I don’t use it. I should probably address my insomnia issues first and then try to implement CPAP.
Here's why: Although your insomnia problems predate starting CPAP, it seems likely to me that if you did manage to "fix" the insomnia problems while not using the CPAP for a while, just as soon as you start trying to use the CPAP, the insomnia is going to come back. So you're still going to be fighting both issues. Better to do it now and just get it done.
So how do you go about fighting both the insomnia and the CPAP at the same time? Here are some of my ideas tailored to your specifics:
1) Clonazepam and whether it positively influences your sleep efficiency: The sleep test with CPAP and clonazepam had a sleep efficiency of 80%. One question you need to ask yourself: Do you have fewer wakes and are the wakes shorter on the nights where you take the clonazepam? If so, then that's evidence that some (or all) of the wakes may indeed be triggered by ongoing anxiety issues since clonazepam is prescribed for panic attacks. If you don't know whether you sleep any better with the clonazepam than without it, you may need to keep a sleep journal and track the difference.
2) Deal with what ever triggered the insomnia in the first place. If you have not resolved the problems that lead to the emotional stress that first triggered the insomnia, you have to do that. As long as you have not come to grips with whatever happened in your life, the insomnia is likely to continue to plague you. How to deal with it, of course, depends on what the triggering event was. But do deal with it instead of allowing it to continue to fester.
3) Wake up time: Have you got a regular wake up time that you use seven days a week instead of a "week day wake up time" and a "week end/days off wake up time"? In the long run, your body will have an easier time consolidating the sleep cycles and not waking up so much if you are getting up at the same time every single day.
4) Bedtime: Have you got a regular bedtime---or at least something that passes for a regular bedtime? And are you usually sleepy at bedtime? Are you sleepy enough to mask up and get to sleep with the mask on your face at bedtime?
5) Middle of the night wakes: What happens when you find yourself awake in the middle of the night? Do you immediately start to worry, get upset, or fret about "Why am I awake?" Do you immediately look at the clock and start calculating how much (or rather how little) sleep you've been able to get since the last wake up? Do you start calculating on how little time there is before you have to get up in the morning? If these things sound like what happens to you when you wake up in the middle of the night, then part of the solution is retraining yourself to not make the wakes worse than they are.
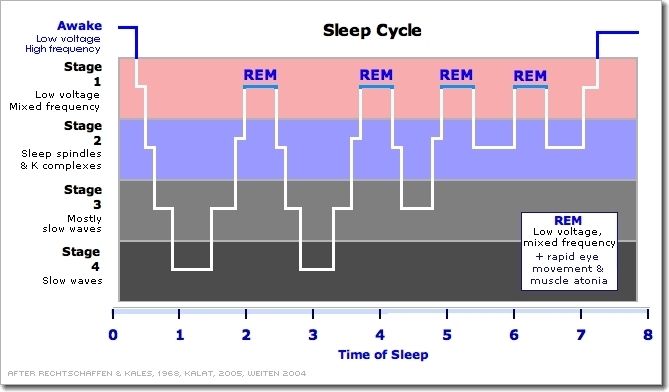
It's important to realize that even "normal" people---those without sleep disordered breathing and those without insomnia often wake up a few times during the night. These wakes are often right after coming out of REM, and they're considered "normal". But a non-insomniac typically doesn't remember these post-REM wakes because they wake up briefly, establish that everything is ok and there's no need to be awake, and quickly settle back down and go back to sleep, usually in less than 5 minutes. But many insomniacs' reaction to finding themselves awake in the middle of the night prolong the middle-of-the-night wakes and that in turn makes them much more disruptive to the overall sleep architecture.
So---if your first response to finding yourself awake in the middle of the night is to look at the clock and start calculating or worrying about how little sleep you've gotten, you need to turn the clock around and not watch it. If you get over anxious in the middle of the night just because you're awake, you need to work on trying to undo the anxiety feedback loop. (Yes, I know that's hard to do.)
6) The troublesome 4am wake in particular. You need to analyze what's triggering this particular wake. Are the garbage trucks on a new schedule and waking you up? A neighbor's dog barking at 4am? Does the heater kick on about that time every night? In other words, see if there is some external trigger for the wake. You might not be able to do anything about it, but if you can figure out that there's an external trigger, then that reduces the anxiety and that in turn may make it easier to get back to sleep: In my case it's a lot easier to get back to sleep after thinking "Darn the snowplow went by again" at 4:00AM than it is to get back to sleep after thinking "Why can't I just get one night's sleep without waking up at 4:00AM?"
If there are no apparent external triggers for the 4:00AM wake, then it's time to start thinking about what you can do to get back to sleep quickly instead of tossing and turning and worrying about the wake. It may be that the easiest thing to do is just get out of bed for a few minutes. Go to the bathroom (even if you don't think you need to.) Get a drink of water. Maybe read for a bit (outside of the bedroom). And go back to bed after you start feeling sleepy again. And don't look at the clock when you are out of bed. Looking at the clock feeds the anxiety.
7) Adjusting to CPAP at the same time as working on the insomnia. The trick here is to teach your body and brain to make a deep triple association:
- Time in Bed = Time to Sleep = Time to Mask Up
- At the beginning of the night, you need to mask up. If you can't get to sleep in 20 minutes OR if you find yourself getting very anxious or mad at the CPAP, it's time to get out of bed and do something else to get your mind off the CPAP. Go back to bed only when you are calm enough and sleepy enough to face masking up again.
- If you wake up without the mask on, don't worry about it[/i]. Just calmly put the mask back on and try to get back to sleep. We can't control our unconsciousness and it happens to some people.
- If you wake up and feel as though you can't stand to have the mask on any more, take the mask off and get out of bed. Go do something soothing and calming. Make yourself a cup of sleepytime tea or read a boring book for a while. When you are both sleepy enough and calm enough to face masking up, go back to bed and try again.
In my case, I had to deal with serious aerophagia and I also had to figure out a way to prevent my lips from getting badly chapped and to keep my arms and chest from feeling the exhaust flow from the mask among other things. The help from people here was critical in solving those problems.