If RERAs are so bad, why aren't they a part of the AHI?
Re: If RERAs are so bad, why aren't they a part of the AHI?
OK, game's back on, but let me plop this here for thought:
http://www.archbronconeumol.org/en/ahi- ... 573/#bib16
http://www.archbronconeumol.org/en/ahi- ... 573/#bib16
Re: If RERAs are so bad, why aren't they a part of the AHI?
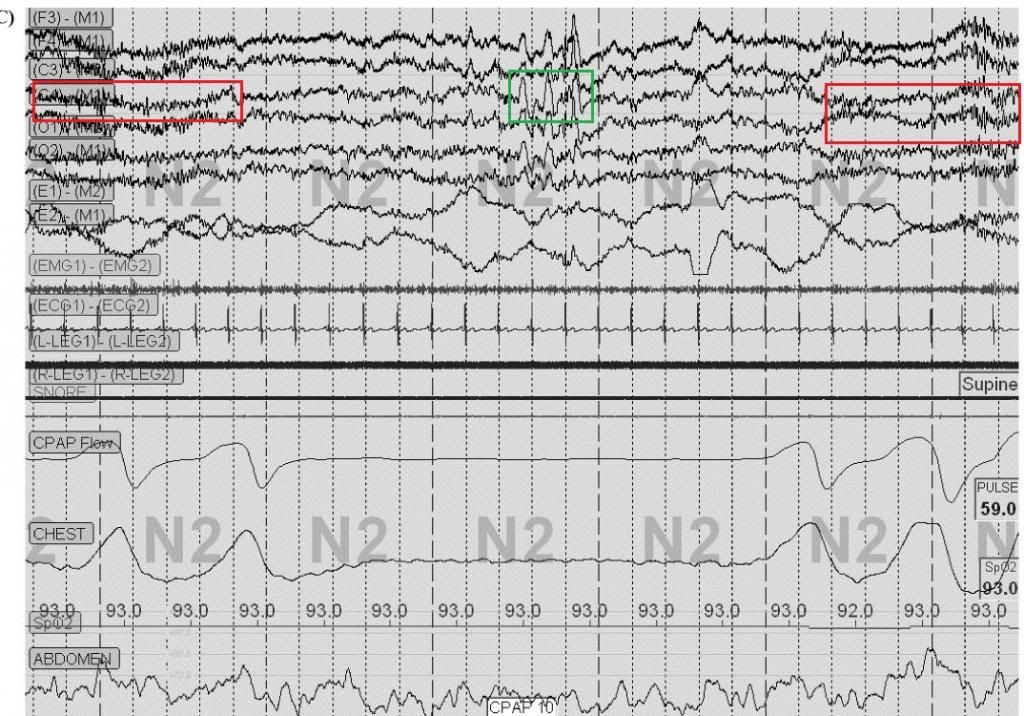
Unfortunately, it isn't "ballistocardiographic effect" this time, as much of the "expiratory intolerance" appears to be related to body motion (see movement in chin and leg leads):mollete wrote:Presently, his scheme is to use ASV. He's still touting "Expiratory Intolerance", but sheepishly says "Yeah, well could be ballistocardiographic effect", a concept he was also introduced to here.
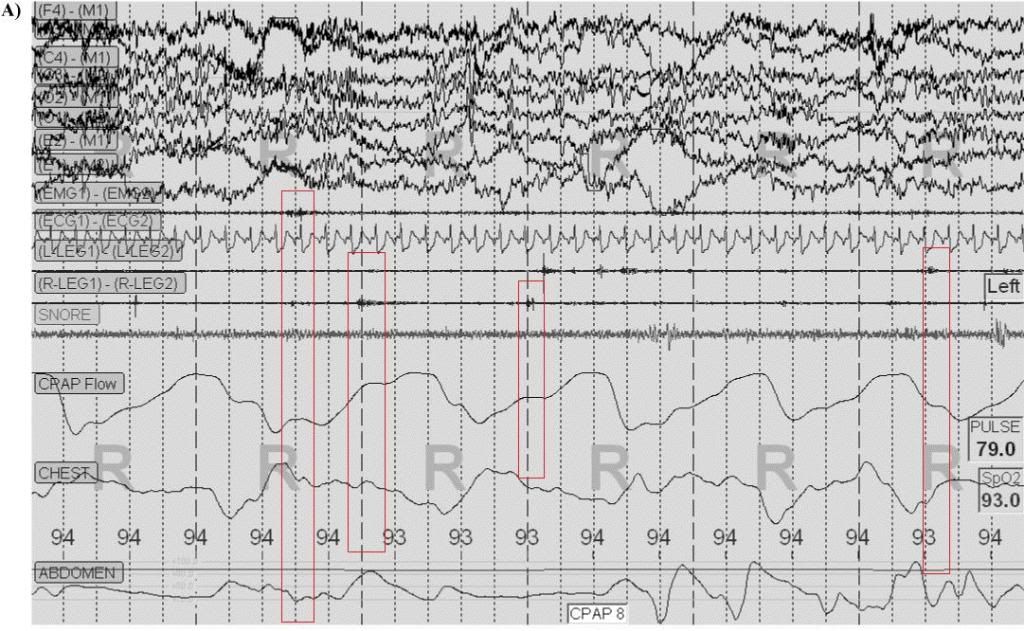
Further, that really doesn't look a lot like REM ("R"), looks more like NREM2. Or else that chin movement makes this REM Behavior Disorder. Chest belt inverted (backwards). Abdominal belt looks blown.
Ecch.
Re: If RERAs are so bad, why aren't they a part of the AHI?
Meanwhile, back at the ranch:
Bench Test Evaluation of Adaptive Servoventilation Devices for Sleep Apnea Treatment
Kaixian Zhu, M.S.1; Haissam Kharboutly, M.S.2; Jianting Ma, M.S.2; Mourad Bouzit, Ph.D.2; Pierre Escourrou, M.D., Ph.D.1, 1Department Explorations Fonctionnelles Multidisciplinaires, AP-HP Antoine-Béclère Hospital, Clamart, France; 2Assistmov SAS, Evry, France.
J Clin Sleep Med 2013;9(9):861-871.
ABSTRACT
Rationale
Adaptive servoventilation devices are marketed to overcome sleep disordered breathing with apneas and hypopneas of both central and obstructive mechanisms often experienced by patients with chronic heart failure. The clinical efficacy of these devices is still questioned.
Study Objectives
This study challenged the detection and treatment capabilities of the three commercially available adaptive servoventilation devices in response to sleep disordered breathing events reproduced on an innovative bench test.
Methods
The bench test consisted of a computer-controlled piston and a Starling resistor. The three devices were subjected to a flow sequence composed of central and obstructive apneas and hypopneas including Cheyne-Stokes respiration derived from a patient. The responses of the devices were separately evaluated with the maximum and the clinical settings (titrated expiratory positive airway pressure), and the detected events were compared to the bench-scored values.
Results
The three devices responded similarly to central events, by increasing pressure support to raise airflow. All central apneas were eliminated, whereas hypopneas remained. The three devices responded differently to the obstructive events with the maximum settings. These obstructive events could be normalized with clinical settings. The residual events of all the devices were scored lower than bench test values with the maximum settings, but were in agreement with the clinical settings. However, their mechanisms were misclassified.
Conclusion
The tested devices reacted as expected to the disordered breathing events, but not sufficiently to normalize the breathing flow. The device-scored results should be used with caution to judge efficacy, as their validity depends upon the initial settings.
- StuUnderPressure
- Posts: 1378
- Joined: Mon Jun 18, 2012 10:34 am
- Location: USA
Re: If RERAs are so bad, why aren't they a part of the AHI?
As one who has a really bad Flow Limitations graph in ResScan, but still maintaining a pretty low AHI (usually 2 or less - sometimes much less), I for one would like to be able to be told "where the source of the limiting factor is"mollete wrote:Anyway, while it may be interesting (although probably not) to look at single breaths and sort them into one of the Nine Different Types of Flow Limitations which somehow identifies where the source of the limiting factor is (Aha! The left nostril had a protuberating turbinate in the power of smegma!), in practice, one has to (or least, this one) look at a trend window of ~about 5 minutes. That said, one has to consider the monitor and resolution one has (i.e., if you're trying to do this with an iPhone, or even a GalS4 sideways, you won't see a lot).
- even if that meant doing another "Sleep Study" JUST for that reason.
_________________
| Machine: AirCurve™ 10 VAuto BiLevel Machine with HumidAir™ Heated Humidifier |
| Additional Comments: Cleanable Water Tub & Respironics Premium Chinstrap |
In Windows 10 Professional 64 bit Version 22H2 - ResScan Version 7.0.1.67 - ResScan Clinician's Manual dtd 2021-02
SD Card Formatter 5.0.2 https://www.sdcard.org/downloads/format ... index.html
SD Card Formatter 5.0.2 https://www.sdcard.org/downloads/format ... index.html
Re: If RERAs are so bad, why aren't they a part of the AHI?
ENT sleep docs who specialize in sleep-related surgeries sometimes enjoy chasing that wild goose.
-
kwikwater
- Posts: 199
- Joined: Fri Jun 12, 2009 8:32 pm
- Location: NW Colorado 50 miles from nowhere
- Contact:
Re: If RERAs are so bad, why aren't they a part of the AHI?
Great topic, once we got on topic!! I'm in the middle of watching my pulse/ox in regards to RERAs to decode my poor sleep quality despite reasonable AHI #s. I think my troubles revolve around hypopnea and RERA more than OA. this is great food for thought for me as I compile data to bring to a Doc, yet to be found. Boy do I dread trying to find a Doc!! The ENT, 90 miles away, that originally prescribed CPAP sends out ALL charts and graphs to a guy 230 miles the opposite direction.. I rely on this board for good info!!!
_________________
| Machine: AirCurve™ 10 VAuto BiLevel Machine with HumidAir™ Heated Humidifier |
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Wellue O2 Ring S, Papcap, OSCAR |
Re: If RERAs are so bad, why aren't they a part of the AHI?
I'd like to ask mollete for some clarification, because the more I read summary of the paper, the more confused I become.
I get the gist of the aritcle: That the ASVs didn't really come out of the bench testing with stellar results. But the more I read the summary, the more questions I have about just what it is the authors of this paper have found when it comes to why the ASVs didn't do so well in the bench testing. Nor can I tell what it is that the authors are recommending when it comes to treating central sleep apnea in general, central and obstructive sleep apnea in patients with chronic heart failure in particular, and in how to measure efficacy of therapy, particularly if the patient self-reports things are not going well.
In particular:
But what do the authors mean when they say the devices were evaluated "with the maximum settings"? Does that mean running the ASV in full Auto mode where the EPAP is allowed to range over a large interval?? Is using a fixed EPAP pressure the only change between devices were used "with maximum settings" and devices were used "with clinical settings"?? Or is the difference something else entirely???
The phrase "The residual events of all the devices were scored lower than bench test values with the maximum settings, but were in agreement with the clinical settings" seems to mean that the devices under score events with "maximum settings". That correct??? And when the machine is run with "clinical settings", the bench test values and the device event scored values are in agreement??? So you would get more accurate device scored data using the patient's titrated EPAP pressure? Or am I completely misinterpreting what the authors are trying to say here?
The phrase "However, their mechanisms were misclassified." seems to indicate that when the device's are recording reasonably accurate data (in terms of number of apneas and hypopneas??), the device's ability to classify the events correctly are not always correct. So does the validity of the device-scored event data depend strongly on what kind of events we're talking about? In other words, are the devices more accurate at scoring apneas than hypopneas? Are they more accurate at scoring obstructive events than other forms of SDB such as flow limitations? Are they accurate in scoring apneas, but inaccurate in distinguishing between CAs and OAs?
Finally, given that the authors say, "The device-scored results should be used with caution to judge efficacy, as their validity depends upon the initial settings.", have they got any suggestions on how efficacy of therapy settings should be judged if the patient reports they are feeling worse with the initiation of therapy instead of feeling better?
I get the gist of the aritcle: That the ASVs didn't really come out of the bench testing with stellar results. But the more I read the summary, the more questions I have about just what it is the authors of this paper have found when it comes to why the ASVs didn't do so well in the bench testing. Nor can I tell what it is that the authors are recommending when it comes to treating central sleep apnea in general, central and obstructive sleep apnea in patients with chronic heart failure in particular, and in how to measure efficacy of therapy, particularly if the patient self-reports things are not going well.
Care to translate some of this into more patient friendly language?mollete wrote:Meanwhile, back at the ranch:
Bench Test Evaluation of Adaptive Servoventilation Devices for Sleep Apnea Treatment
Kaixian Zhu, M.S.1; Haissam Kharboutly, M.S.2; Jianting Ma, M.S.2; Mourad Bouzit, Ph.D.2; Pierre Escourrou, M.D., Ph.D.1, 1Department Explorations Fonctionnelles Multidisciplinaires, AP-HP Antoine-Béclère Hospital, Clamart, France; 2Assistmov SAS, Evry, France.
J Clin Sleep Med 2013;9(9):861-871.
ABSTRACT
Rationale
Adaptive servoventilation devices are marketed to overcome sleep disordered breathing with apneas and hypopneas of both central and obstructive mechanisms often experienced by patients with chronic heart failure. The clinical efficacy of these devices is still questioned.
Study Objectives
This study challenged the detection and treatment capabilities of the three commercially available adaptive servoventilation devices in response to sleep disordered breathing events reproduced on an innovative bench test.
Methods
The bench test consisted of a computer-controlled piston and a Starling resistor. The three devices were subjected to a flow sequence composed of central and obstructive apneas and hypopneas including Cheyne-Stokes respiration derived from a patient. The responses of the devices were separately evaluated with the maximum and the clinical settings (titrated expiratory positive airway pressure), and the detected events were compared to the bench-scored values.
Results
The three devices responded similarly to central events, by increasing pressure support to raise airflow. All central apneas were eliminated, whereas hypopneas remained. The three devices responded differently to the obstructive events with the maximum settings. These obstructive events could be normalized with clinical settings. The residual events of all the devices were scored lower than bench test values with the maximum settings, but were in agreement with the clinical settings. However, their mechanisms were misclassified.
Conclusion
The tested devices reacted as expected to the disordered breathing events, but not sufficiently to normalize the breathing flow. The device-scored results should be used with caution to judge efficacy, as their validity depends upon the initial settings.
In particular:
Were the hypopneas that remained ones scored by the machine? Or were they ones that would have been scored on an PSG? Or both?"All central apneas were eliminated, whereas hypopneas remained. "
Meaning??? The way I read this is that the machines did a better job of normalizing the obstructive events when the EPAP pressure was set to the pressure determined in the lab. Is that a reasonably accurate interpretation? (As I read the Methods section, the bench test was using a computer-controlled piston to mimic data from a real patient; presumably the "titrated pressure" is the titrated pressure for the patient from whom the data came??)"The responses of the devices were separately evaluated with the maximum and the clinical settings (titrated expiratory positive airway pressure) ... .
and
The three devices responded differently to the obstructive events with the maximum settings. These obstructive events could be normalized with clinical settings.
But what do the authors mean when they say the devices were evaluated "with the maximum settings"? Does that mean running the ASV in full Auto mode where the EPAP is allowed to range over a large interval?? Is using a fixed EPAP pressure the only change between devices were used "with maximum settings" and devices were used "with clinical settings"?? Or is the difference something else entirely???
Does "the detected events were compared to the bench-scored values" mean the authors were testing for the accuracy of the events data as scored by the devices? Does "their validity depends upon the initial settings" mean that the device-scored data is more accurate when using the titrated (fixed?) EPAP than it is when the machine is running in auto mode? Do the many, many other settings on an ASV adversely affect the accuracy of the data?"... the detected events were compared to the bench-scored values.
and
"The residual events of all the devices were scored lower than bench test values with the maximum settings, but were in agreement with the clinical settings. However, their mechanisms were misclassified."
and
"The device-scored results should be used with caution to judge efficacy, as their validity depends upon the initial settings."
The phrase "The residual events of all the devices were scored lower than bench test values with the maximum settings, but were in agreement with the clinical settings" seems to mean that the devices under score events with "maximum settings". That correct??? And when the machine is run with "clinical settings", the bench test values and the device event scored values are in agreement??? So you would get more accurate device scored data using the patient's titrated EPAP pressure? Or am I completely misinterpreting what the authors are trying to say here?
The phrase "However, their mechanisms were misclassified." seems to indicate that when the device's are recording reasonably accurate data (in terms of number of apneas and hypopneas??), the device's ability to classify the events correctly are not always correct. So does the validity of the device-scored event data depend strongly on what kind of events we're talking about? In other words, are the devices more accurate at scoring apneas than hypopneas? Are they more accurate at scoring obstructive events than other forms of SDB such as flow limitations? Are they accurate in scoring apneas, but inaccurate in distinguishing between CAs and OAs?
Finally, given that the authors say, "The device-scored results should be used with caution to judge efficacy, as their validity depends upon the initial settings.", have they got any suggestions on how efficacy of therapy settings should be judged if the patient reports they are feeling worse with the initiation of therapy instead of feeling better?
_________________
| Machine: DreamStation BiPAP® Auto Machine |
| Mask: Swift™ FX Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: PR System DreamStation and Humidifier. Max IPAP = 9, Min EPAP=4, Rise time setting = 3, minPS = 3, maxPS=5 |
Re: If RERAs are so bad, why aren't they a part of the AHI?
Well, I think they just do fiberoptic or video laryngoscopy and then start hacking.jnk wrote:ENT sleep docs who specialize in sleep-related surgeries sometimes enjoy chasing that wild goose.
Maybe some rhinometry, if they got one hanging around.
And if the insurers don't say
xxx considers rhinomanometry, acoustic rhinometry, and optical rhinometry experimental and investigational because of a lack of clinical studies demonstrating that these tests improve clinical outcomes.
Re: If RERAs are so bad, why aren't they a part of the AHI?
You must have a voice-recognition program...robysue wrote:I'd like to ask mollete for some clarification, because the more I read summary of the paper, the more confused I become.
I get the gist of the aritcle: That the ASVs didn't really come out of the bench testing with stellar results. But the more I read the summary, the more questions I have about just what it is the authors of this paper have found when it comes to why the ASVs didn't do so well in the bench testing. Nor can I tell what it is that the authors are recommending when it comes to treating central sleep apnea in general, central and obstructive sleep apnea in patients with chronic heart failure in particular, and in how to measure efficacy of therapy, particularly if the patient self-reports things are not going well.
Care to translate some of this into more patient friendly language?mollete wrote:Meanwhile, back at the ranch:
Bench Test Evaluation of Adaptive Servoventilation Devices for Sleep Apnea Treatment
Kaixian Zhu, M.S.1; Haissam Kharboutly, M.S.2; Jianting Ma, M.S.2; Mourad Bouzit, Ph.D.2; Pierre Escourrou, M.D., Ph.D.1, 1Department Explorations Fonctionnelles Multidisciplinaires, AP-HP Antoine-Béclère Hospital, Clamart, France; 2Assistmov SAS, Evry, France.
J Clin Sleep Med 2013;9(9):861-871.
ABSTRACT
Rationale
Adaptive servoventilation devices are marketed to overcome sleep disordered breathing with apneas and hypopneas of both central and obstructive mechanisms often experienced by patients with chronic heart failure. The clinical efficacy of these devices is still questioned.
Study Objectives
This study challenged the detection and treatment capabilities of the three commercially available adaptive servoventilation devices in response to sleep disordered breathing events reproduced on an innovative bench test.
Methods
The bench test consisted of a computer-controlled piston and a Starling resistor. The three devices were subjected to a flow sequence composed of central and obstructive apneas and hypopneas including Cheyne-Stokes respiration derived from a patient. The responses of the devices were separately evaluated with the maximum and the clinical settings (titrated expiratory positive airway pressure), and the detected events were compared to the bench-scored values.
Results
The three devices responded similarly to central events, by increasing pressure support to raise airflow. All central apneas were eliminated, whereas hypopneas remained. The three devices responded differently to the obstructive events with the maximum settings. These obstructive events could be normalized with clinical settings. The residual events of all the devices were scored lower than bench test values with the maximum settings, but were in agreement with the clinical settings. However, their mechanisms were misclassified.
Conclusion
The tested devices reacted as expected to the disordered breathing events, but not sufficiently to normalize the breathing flow. The device-scored results should be used with caution to judge efficacy, as their validity depends upon the initial settings.
In particular:Were the hypopneas that remained ones scored by the machine? Or were they ones that would have been scored on an PSG? Or both?"All central apneas were eliminated, whereas hypopneas remained. "
Meaning??? The way I read this is that the machines did a better job of normalizing the obstructive events when the EPAP pressure was set to the pressure determined in the lab. Is that a reasonably accurate interpretation? (As I read the Methods section, the bench test was using a computer-controlled piston to mimic data from a real patient; presumably the "titrated pressure" is the titrated pressure for the patient from whom the data came??)"The responses of the devices were separately evaluated with the maximum and the clinical settings (titrated expiratory positive airway pressure) ... .
and
The three devices responded differently to the obstructive events with the maximum settings. These obstructive events could be normalized with clinical settings.
But what do the authors mean when they say the devices were evaluated "with the maximum settings"? Does that mean running the ASV in full Auto mode where the EPAP is allowed to range over a large interval?? Is using a fixed EPAP pressure the only change between devices were used "with maximum settings" and devices were used "with clinical settings"?? Or is the difference something else entirely???
Does "the detected events were compared to the bench-scored values" mean the authors were testing for the accuracy of the events data as scored by the devices? Does "their validity depends upon the initial settings" mean that the device-scored data is more accurate when using the titrated (fixed?) EPAP than it is when the machine is running in auto mode? Do the many, many other settings on an ASV adversely affect the accuracy of the data?"... the detected events were compared to the bench-scored values.
and
"The residual events of all the devices were scored lower than bench test values with the maximum settings, but were in agreement with the clinical settings. However, their mechanisms were misclassified."
and
"The device-scored results should be used with caution to judge efficacy, as their validity depends upon the initial settings."
The phrase "The residual events of all the devices were scored lower than bench test values with the maximum settings, but were in agreement with the clinical settings" seems to mean that the devices under score events with "maximum settings". That correct??? And when the machine is run with "clinical settings", the bench test values and the device event scored values are in agreement??? So you would get more accurate device scored data using the patient's titrated EPAP pressure? Or am I completely misinterpreting what the authors are trying to say here?
The phrase "However, their mechanisms were misclassified." seems to indicate that when the device's are recording reasonably accurate data (in terms of number of apneas and hypopneas??), the device's ability to classify the events correctly are not always correct. So does the validity of the device-scored event data depend strongly on what kind of events we're talking about? In other words, are the devices more accurate at scoring apneas than hypopneas? Are they more accurate at scoring obstructive events than other forms of SDB such as flow limitations? Are they accurate in scoring apneas, but inaccurate in distinguishing between CAs and OAs?
Finally, given that the authors say, "The device-scored results should be used with caution to judge efficacy, as their validity depends upon the initial settings.", have they got any suggestions on how efficacy of therapy settings should be judged if the patient reports they are feeling worse with the initiation of therapy instead of feeling better?
Re: If RERAs are so bad, why aren't they a part of the AHI?
For all those guys who said "Oh yeah, I can titrate any CompSAS patient with a BiPAP S/T. Don't need no ASV."
But how long does it last?
But how long does it last?
Randomized controlled trial of noninvasive positive pressure ventilation (NPPV) versus servoventilation in patients with CPAP-induced central sleep apnea (complex sleep apnea).
Dellweg D, Kerl J, Hoehn E, Wenzel M, Koehler D.
Kloster Grafschaft, Pulmonary Medicine I, Home Mechanical Ventilation Unit and Sleep Laboratory, Schmallenberg, Germany.
Sleep. 2013 Aug 1;36(8):1163-71.
STUDY OBJECTIVES:
To compare the treatment effect of noninvasive positive pressure ventilation (NPPV) and anticyclic servoventilation in patients with continuous positive airway pressure (CPAP)-induced central sleep apnea (complex sleep apnea).
DESIGN:
Randomized controlled trial.
SETTING:
Sleep center.
PATIENTS:
Thirty patients who developed complex sleep apnea syndrome (CompSAS) during CPAP treatment.
INTERVENTIONS:
NPPV or servoventilation.
MEASUREMENTS AND RESULTS:
Patients were randomized to NPPV or servo-ventilation. Full polysomnography (PSG) was performed after 6 weeks. On CPAP prior to randomization, patients in the NPPV and servoventilator arm had comparable apnea-hypopnea indices (AHI, 28.6 ± 6.5 versus 27.7 ± 9.7 events/h (mean ± standard deviation [SD])), apnea indices (AI,19 ± 5.6 versus 21.1 ± 8.6 events/h), central apnea indices (CAI, 16.7 ± 5.4 versus 18.2 ± 7.1 events/h), oxygen desaturation indices (ODI,17.5 ± 13.1 versus 24.3 ± 11.9 events/h). During initial titration NPPV and servoventilation significantly improved the AHI (9.1 ± 4.3 versus 9 ± 6.4 events/h), AI (2 ± 3.1 versus 3.5 ± 4.5 events/h) CAI (2 ± 3.1 versus 2.5 ± 3.9 events/h) and ODI (10.1 ± 4.5 versus 8.9 ± 8.4 events/h) when compared to CPAP treatment (all P < 0.05). After 6 weeks we observed the following differences: AHI (16.5 ± 8 versus 7.4 ± 4.2 events/h, P = 0.027), AI (10.4 ± 5.9 versus 1.7 ± 1.9 events/h, P = 0.001), CAI (10.2 ± 5.1 versus 1.5 ± 1.7 events/h, P < 0.0001)) and ODI (21.1 ± 9.2 versus 4.8 ± 3.4 events/h, P < 0.0001) for NPPV and servoventilation, respectively. Other sleep parameters were unaffected by any form of treatment.
CONCLUSIONS:
After 6 weeks, servoventilation treated respiratory events more effectively than NPPV in patients with complex sleep apnea syndrome.
Re: If RERAs are so bad, why aren't they a part of the AHI?
Robysue,
I think mollete's main point is that there is little objective evidence to suggest ASV as the best approach for treating UARS/RERAs, despite what Dr. K suggests in one of his aspiring protocols.
Thing is, I personally don't think Dr. K cares a rat's tail what the objective evidence suggests--other than maybe having some sort of paper or some squiggly lines to point to in his efforts to get insurance to pay for nonstandard protocols, which, in my opinion, is a worthy endeavor, possibly touching on the heroic, when speaking of a doc who mostly deals with people who haven't done so well when the standard protocols were used.
I don't think Dr. K is much of a 'thinking inside the box' kinda guy. He seems to be one of those who refuses to acknowledge that there even is a box. He just wants to help people who haven't been helped, yet, by all the other more standard stuff out there. And, well, I don't think he wants to be doing it for free, naturally.
But that's just my take as another opinionated guy spouting off about stuff on the Internet, whether I know much about it or not.
I think mollete's main point is that there is little objective evidence to suggest ASV as the best approach for treating UARS/RERAs, despite what Dr. K suggests in one of his aspiring protocols.
Thing is, I personally don't think Dr. K cares a rat's tail what the objective evidence suggests--other than maybe having some sort of paper or some squiggly lines to point to in his efforts to get insurance to pay for nonstandard protocols, which, in my opinion, is a worthy endeavor, possibly touching on the heroic, when speaking of a doc who mostly deals with people who haven't done so well when the standard protocols were used.
I don't think Dr. K is much of a 'thinking inside the box' kinda guy. He seems to be one of those who refuses to acknowledge that there even is a box. He just wants to help people who haven't been helped, yet, by all the other more standard stuff out there. And, well, I don't think he wants to be doing it for free, naturally.
But that's just my take as another opinionated guy spouting off about stuff on the Internet, whether I know much about it or not.
Re: If RERAs are so bad, why aren't they a part of the AHI?
None of the last several very technical posts do anything to dispel the notion that it's somewhat futile to go chasing better RERA numbers by adjusting pressures on a home machine once one's AHI is satisfactory, do they?
In my case it seems to be a bit of a trade-off. Up to the point where I am now my AHI numbers have actually improved with lower pressures (which as a layman I attribute to a much better leak profile) but my RERAs have increased slightly. I feel about the same through the day.
In my case it seems to be a bit of a trade-off. Up to the point where I am now my AHI numbers have actually improved with lower pressures (which as a layman I attribute to a much better leak profile) but my RERAs have increased slightly. I feel about the same through the day.
_________________
| Machine: ResMed AirSense™ 10 AutoSet™ CPAP Machine with HumidAir™ Heated Humidifier |
| Mask: DreamWear Full Face CPAP Mask with Headgear (Small and Medium Frame Included) |
| Additional Comments: Pressure 11.0 Min-->14.0 Max EPR 2 |
Re: If RERAs are so bad, why aren't they a part of the AHI?
It is possible that increasing pressure on a CPAP will make some patients feel better because of further airway stabilization, regardless of what the numbers reported by the home treatment machine are.
The trade-off equation, as far as sleep and pressure choices are concerned for tweaking our own pressures, is generally a matter of comfort vs. stabilization. Discomfort can ruin sleep just as easily as an unstable airway. Personal tweaking is the process of finding one's personal sweet spot--lowest trending numbers, most comfort, best sleep. The machine-reported RERA numbers may, or may not, help with that process. It is a highly individual thing, in my opinion.
Breathing can only be corrected so far with PAP, and that's OK. If the imperfect breathing, in the form of home-treatment-machine-reported hypopneas and RERAs, isn't destroying sleep, then it isn't worth worrying about. On the other hand, if sleep still isn't refreshing, trying a slightly higher pressure is worth a try. If it doesn't seem to help anything, just do what is most comfortable. IMO.
Dr. K often ends up with the people who have disturbed sleep from personal pressure issues and discomfort. For them, trying bilevel or ASV or whatever may pan out for them. But there are plenty of other things that are more sleep-related than breathing-related that could be much more likely to pan out for them.
There is more to sleep than just breathing.
mollete taught me that.
The trade-off equation, as far as sleep and pressure choices are concerned for tweaking our own pressures, is generally a matter of comfort vs. stabilization. Discomfort can ruin sleep just as easily as an unstable airway. Personal tweaking is the process of finding one's personal sweet spot--lowest trending numbers, most comfort, best sleep. The machine-reported RERA numbers may, or may not, help with that process. It is a highly individual thing, in my opinion.
Breathing can only be corrected so far with PAP, and that's OK. If the imperfect breathing, in the form of home-treatment-machine-reported hypopneas and RERAs, isn't destroying sleep, then it isn't worth worrying about. On the other hand, if sleep still isn't refreshing, trying a slightly higher pressure is worth a try. If it doesn't seem to help anything, just do what is most comfortable. IMO.
Dr. K often ends up with the people who have disturbed sleep from personal pressure issues and discomfort. For them, trying bilevel or ASV or whatever may pan out for them. But there are plenty of other things that are more sleep-related than breathing-related that could be much more likely to pan out for them.
There is more to sleep than just breathing.
mollete taught me that.
Re: If RERAs are so bad, why aren't they a part of the AHI?
Well then why, may I ask, does he continue to try to present "objective evidence" that it does?jnk wrote:Thing is, I personally don't think Dr. K cares a rat's tail what the objective evidence suggests...
Is it because his technical "help" is poor and he's getting bad advice?
And if what you're saying is true, then that just makes him another "dial winger".
I would also offer another variable that might serve to explain improvement/adherence/compliance or whatever it exactly is that's going on here. You apply 40 hours of Basic and/or Intensive Support to anyone who's doing poorly and they're going to do better in selected parameters. As you have noted:
and Barry is certainly an excellent PTSD man.jnk wrote:Dr. K often ends up with the people who have disturbed sleep from personal pressure issues and discomfort. For them, trying bilevel or ASV or whatever may pan out for them. But there are plenty of other things that are more sleep-related than breathing-related that could be much more likely to pan out for them.
There is more to sleep than just breathing.