After following my sleepyhead data for a week and a half now, I'm noticing that my apnea events are still pretty high during times of the night (12-15/hr). Right now, my pressure is at 8 and 10. I feel my leaks are fairly well under control now, so I think I'm getting the therapy my unit is programmed to give.
I'm thinking of increasing my pressure to see if my events come down. I have a couple questions in this respect:
1. I notice that many people have a wider range of pressures in the APAP settings. Mine are only 2 units apart. Should I widen this?
2. If I do increase the base pressure (8), how much should I go? 1/2 a unit or 1 unit?
Thanks,
Q
Should I increase my pressure?
Should I increase my pressure?
_________________
| Machine: PR System One REMStar 60 Series Auto CPAP Machine |
| Mask: Wisp Nasal CPAP Mask with Headgear - Fit Pack |
Re: Should I increase my pressure?
I would switch to CPAP mode and raise the pressure 1 cm per week from 8 cm up to 12 cm, and see if it makes a diff. Only after finding the optimal pressure in the CPAP mode I would try APAP set with the optimal pressure as maximum. BTW, APAP machines are contra indicated in medical cases of Central Sleep Apnea Syndrome (such as in heart problems), COPD, lungs hypo respiration, etc.
_________________
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 Autoset machine; Ruby chinstrap under the mask straps; ResScan 5.6 |
Last edited by avi123 on Fri Mar 29, 2013 6:51 pm, edited 1 time in total.
see my recent set-up and Statistics:
http://i.imgur.com/TewT8G9.png
see my recent ResScan treatment results:
http://i.imgur.com/3oia0EY.png
http://i.imgur.com/QEjvlVY.png
http://i.imgur.com/TewT8G9.png
see my recent ResScan treatment results:
http://i.imgur.com/3oia0EY.png
http://i.imgur.com/QEjvlVY.png
Re: Should I increase my pressure?
Can you post a recent detailed report showing the events graph please?
Are you talking about the AHI graph where it shows under the flow rate graph?
I just looked at one of your first reports from Encore and it didn't show AHI that high.
Are you talking about the AHI graph where it shows under the flow rate graph?
I just looked at one of your first reports from Encore and it didn't show AHI that high.
_________________
| Machine: AirCurve™ 10 VAuto BiLevel Machine with HumidAir™ Heated Humidifier |
| Additional Comments: Mask Bleep Eclipse https://bleepsleep.com/the-eclipse/ |
I may have to RISE but I refuse to SHINE.
Re: Should I increase my pressure?
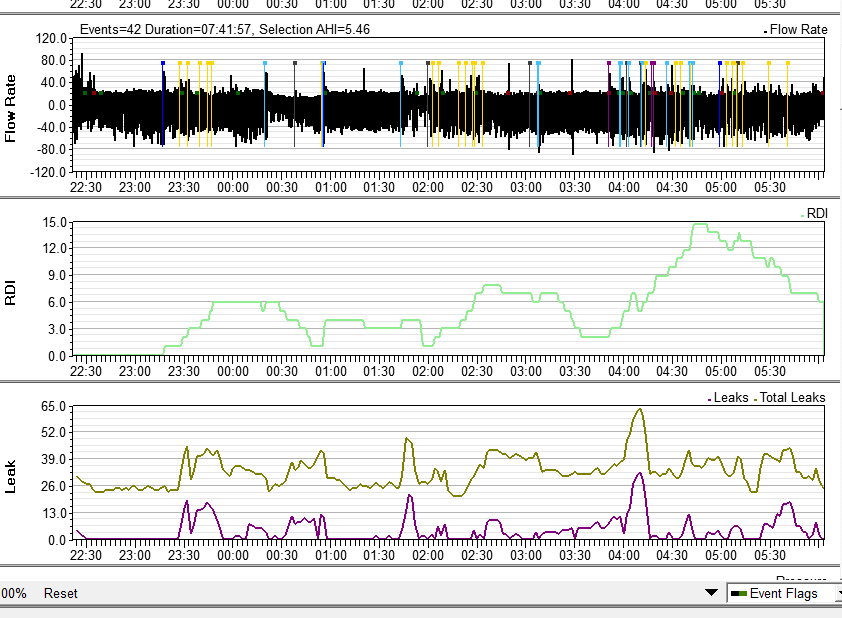
My sleep issue was with RDIs, not AHIs (just found this out after talking to a PA at my sleep Dr. office). My initial sleep study had my RHI at 31, but my AHI at only 4. I reconfigured sleephead to show RDIs and noticed that my level gets up to 15+ 2-3 times a night.Pugsy wrote:Can you post a recent detailed report showing the events graph please?
Are you talking about the AHI graph where it shows under the flow rate graph?
I just looked at one of your first reports from Encore and it didn't show AHI that high.
Here is my sleephead detail from last night. Last night was one of my better nights, with only one period where my RDI level got up to 15.
_________________
| Machine: PR System One REMStar 60 Series Auto CPAP Machine |
| Mask: Wisp Nasal CPAP Mask with Headgear - Fit Pack |
Re: Should I increase my pressure?
Gottcha. You know that pattern looks suspiciously like a REM stage sleep pattern.
If it were me and I was in your situation I would increase the minimum 1 cm and the max I would increase maybe 2 or 3 cm. I don't think you are going to need much more maximum but I think a little more minimum would likely do a better job of preventing things rather than trying to play catch up. I believe in your situation (as with most people really) the minimum is likely going to be more critical.
You could probably open up the range more but I don't think you are going to need it...on the Encore report you just didn't max out 10 cm for any huge amount of time. If you wanted to do the standard 4 cm range that a lot of people like to do it probably would never reach the max. It's a good modest range that I suspect would work well though.
The minimum is the main issue though and not the maximum. With a good effective minimum it's very likely that the pressure won't need to range very much.
See this link and the hypnogram on the right (scroll down just a little) and you will see what I mean about REM stage sleep pattern. It's common for people to have more tendency to have the airway collapse and/or need a wee bit more pressure during REM stage sleep.
Also for supine sleeping but your RDI clusters look a lot like REM pattern to me.
http://en.wikipedia.org/wiki/Sleep
If it were me and I was in your situation I would increase the minimum 1 cm and the max I would increase maybe 2 or 3 cm. I don't think you are going to need much more maximum but I think a little more minimum would likely do a better job of preventing things rather than trying to play catch up. I believe in your situation (as with most people really) the minimum is likely going to be more critical.
You could probably open up the range more but I don't think you are going to need it...on the Encore report you just didn't max out 10 cm for any huge amount of time. If you wanted to do the standard 4 cm range that a lot of people like to do it probably would never reach the max. It's a good modest range that I suspect would work well though.
The minimum is the main issue though and not the maximum. With a good effective minimum it's very likely that the pressure won't need to range very much.
See this link and the hypnogram on the right (scroll down just a little) and you will see what I mean about REM stage sleep pattern. It's common for people to have more tendency to have the airway collapse and/or need a wee bit more pressure during REM stage sleep.
Also for supine sleeping but your RDI clusters look a lot like REM pattern to me.
http://en.wikipedia.org/wiki/Sleep
_________________
| Machine: AirCurve™ 10 VAuto BiLevel Machine with HumidAir™ Heated Humidifier |
| Additional Comments: Mask Bleep Eclipse https://bleepsleep.com/the-eclipse/ |
I may have to RISE but I refuse to SHINE.
Re: Should I increase my pressure?
Thanks Pugsy! Very good reference info.
I'll mess with my pressures here tonight and see how things play out the next couple days.
Q
I'll mess with my pressures here tonight and see how things play out the next couple days.
Q
_________________
| Machine: PR System One REMStar 60 Series Auto CPAP Machine |
| Mask: Wisp Nasal CPAP Mask with Headgear - Fit Pack |
Re: Should I increase my pressure?
Dynamic CO2 therapy in periodic breathing: a modeling study to determine optimal timing and dosage regimes
Yoseph Mebrate, Keith Willson, Charlotte H. Manisty, Resham Baruah, Jamil Mayet, Alun D. Hughes, Kim H. Parker and Darrel P. Francis
J Appl Physiol 107:696-706, 2009. First published 23 July 2009; doi: 10.1152/japplphysiol.90308.2008
Link: http://www.ncbi.nlm.nih.gov/pubmed/19628721
Gilmartin G, McGeehan B, Vigneault K, Daly RW, Manento M, Weiss JW, Thomas RJ.
Treatment of positive airway pressure treatment-associated respiratory instability with enhanced expiratory rebreathing space (EERS).
Source: J Clin Sleep Med. 2010 Dec 15;6(6):529-38. Division of Pulmonary, Critical Care and Sleep Medicine, Beth Israel Deaconess Medical Center, Boston, MA, USA.
Link: http://www.ncbi.nlm.nih.gov/pubmed/21206741
Yoseph Mebrate, Keith Willson, Charlotte H. Manisty, Resham Baruah, Jamil Mayet, Alun D. Hughes, Kim H. Parker and Darrel P. Francis
J Appl Physiol 107:696-706, 2009. First published 23 July 2009; doi: 10.1152/japplphysiol.90308.2008
Link: http://www.ncbi.nlm.nih.gov/pubmed/19628721
Gilmartin G, McGeehan B, Vigneault K, Daly RW, Manento M, Weiss JW, Thomas RJ.
Treatment of positive airway pressure treatment-associated respiratory instability with enhanced expiratory rebreathing space (EERS).
Source: J Clin Sleep Med. 2010 Dec 15;6(6):529-38. Division of Pulmonary, Critical Care and Sleep Medicine, Beth Israel Deaconess Medical Center, Boston, MA, USA.
Link: http://www.ncbi.nlm.nih.gov/pubmed/21206741
May any shills trolls sockpuppets or astroturfers at cpaptalk.com be like chaff before the wind!











