How Do You Know if You Need BiPap?
-
need2snooze
- Posts: 60
- Joined: Fri Apr 27, 2012 8:13 pm
How Do You Know if You Need BiPap?
In my quest to find that elusive night of wonderful, rested sleep after over four years of CPAP, I'm wondering if I'm using the right machine - S9 Autoset. My dr. has never suggested it, but I'm curious about BiPap. Is it only for people who need high pressure settings b/c of high AHI numbers? Could BiPap possibly help with the aerophagia and sleeping better through the night?
_________________
| Mask: Mirage™ FX For Her Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
Re: How Do You Know if You Need BiPap?
normally bi-level prescribe to people with OSA who non-responsive or non-tolerant of cpapneed2snooze wrote:Is it only for people who need high pressure settings b/c of high AHI numbers? Could BiPap possibly help with the aerophagia and sleeping better through the night?
nothing to do with AHI numbers but people on high pressure might find breathing out on bi-level pressure support more tolerable than cpap
pressure support can help with aerophagia as can be set higher than cpap EPR 3
Re: How Do You Know if You Need BiPap?
Hi,need2snooze wrote:...I'm curious about BiPap. Is it only for people who need high pressure settings b/c of high AHI numbers?
BiPAP is typically needed by people who have issues with pressure causing central events to happen. They get into a catch-22 where the pressure needed for treating OSA events is higher than the pressure that causes central events. By using 2 different pressure levels, the machine can get past that catch-22 situation.
BiPAP is also used by people who need a high pressure level since using a lower exhale pressure can make it a lot easier to breathe using the machine.
When I first started, I needed BiPAP because I wasn't able to get used to exhaling under the high pressure level that I needed. BiPAP ended up being very comfortable, which solved the problem. Over time, due to weight loss, I now need far lower pressure levels. I could successfully use an APAP machine at the current time, but I am so used to BiPAP that I continue to use it. I already have 2 BiPAP machines, so I continue to use them.
What pressure levels are you on, and what issues are you having? BiPAP might or might or might not help with the air ingestion issue. If you want to give it a try, ask you doctor or DME if you could borrow or rent a BiPAP for a short period of time. It is always hard to tell...it could be a goose chase, or it could be the silver bullet that fixes everything.
-john-
Re: How Do You Know if You Need BiPap?
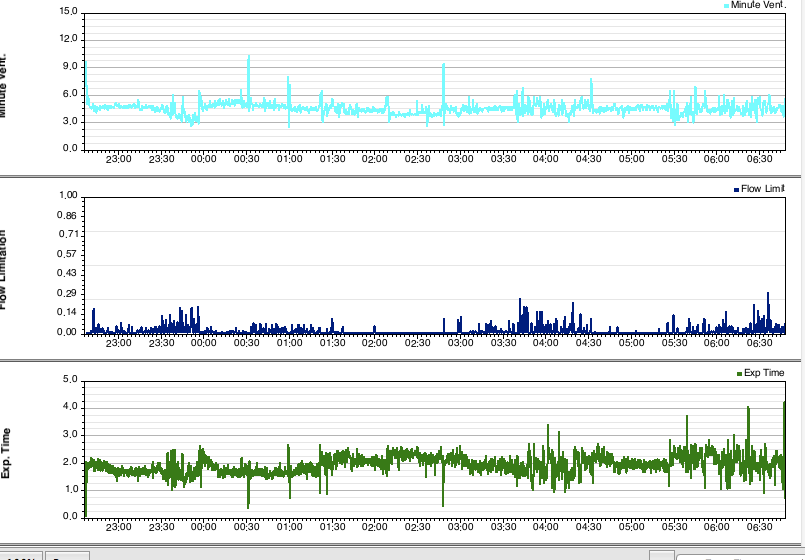
I thought I'd share here what happened with my recent switch to bipap: First screenshot is my flow limitation graph on auto CPAP with max pressure at 8.4. This is where my pressure has been set for most of the 8 months I've been on APAP:

I tried to increase my max pressure in order to reduce that flow limitation -- below is a graph from when I increased my max APAP pressure to 9.4. Better, but I got bad aerophagia at this pressure and couldn't stay there.

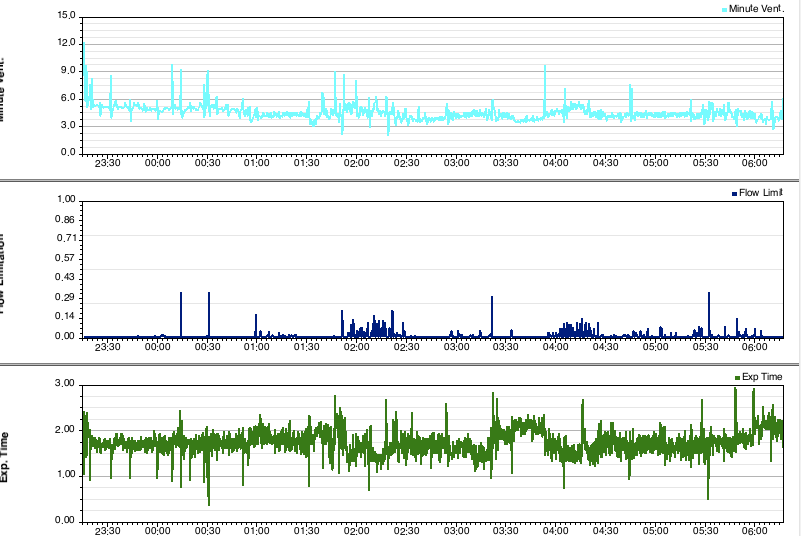
I started on bipap auto just four nights ago and the next screenshot is my flow limitation graph from last night. My max IPAP is 9.4, same as my max pressure on APAP in the screenshot above, and just 1 cm higher than the pressure in the first screenshot, but what a difference:

The reason for the switch to bipap was not because of my AHI which has always been below 1. By switching to bipap I've been able to significantly decrease that flow limitation (which I suspected was disrupting my sleep and making me feel pretty crappy) without getting aerophagia. On APAP I couldn't stay consistently above 9 without getting bad aerophagia, but no problem on bipap auto with max IPAP 9.4.
As an aside -- while it is taking some getting used to the new machine, I feel like breathing is more comfortable for me on bipap -- it's like the machine seems more sensitive to my own breathing rhythm. Hard to describe.

I tried to increase my max pressure in order to reduce that flow limitation -- below is a graph from when I increased my max APAP pressure to 9.4. Better, but I got bad aerophagia at this pressure and couldn't stay there.

I started on bipap auto just four nights ago and the next screenshot is my flow limitation graph from last night. My max IPAP is 9.4, same as my max pressure on APAP in the screenshot above, and just 1 cm higher than the pressure in the first screenshot, but what a difference:

The reason for the switch to bipap was not because of my AHI which has always been below 1. By switching to bipap I've been able to significantly decrease that flow limitation (which I suspected was disrupting my sleep and making me feel pretty crappy) without getting aerophagia. On APAP I couldn't stay consistently above 9 without getting bad aerophagia, but no problem on bipap auto with max IPAP 9.4.
As an aside -- while it is taking some getting used to the new machine, I feel like breathing is more comfortable for me on bipap -- it's like the machine seems more sensitive to my own breathing rhythm. Hard to describe.
_________________
| Machine: AirSense 10 AutoSet with Heated Humidifer + Aifit N30i Nasal Mask Bundle |
| Additional Comments: SleepyHead-now-OSCAR software on Mac OSX Ventura |
Re: How Do You Know if You Need BiPap?
In addition to cpap intolerance at higher pressures, some co-morbidities of COPD, Parkinsons's or loss of lung tissue can be helped by using the bi-pap. In some cases, COPD gas exchanges are better (exhaling carbon dioxide). With Parkinson's, the breathing mechanism within the brain is stimulated. With lung tissue loses, air is pushed further in.
Also, some morbidly obese ppl need a bipap to overcome the weight on the chest....ie much higher pressures are needed. I have personally got the pressure up to 27/21 for one patient.
Also, some morbidly obese ppl need a bipap to overcome the weight on the chest....ie much higher pressures are needed. I have personally got the pressure up to 27/21 for one patient.
Re: How Do You Know if You Need BiPap?
Sorry to get off of the topic but I am floored that anyone could tolerate that high of a pressure, even on bipap. And where the heck could you find a mask that doesn't leak?stage0 wrote:In addition to cpap intolerance at higher pressures, some co-morbidities of COPD, Parkinsons's or loss of lung tissue can be helped by using the bi-pap. In some cases, COPD gas exchanges are better (exhaling carbon dioxide). With Parkinson's, the breathing mechanism within the brain is stimulated. With lung tissue loses, air is pushed further in.
Also, some morbidly obese ppl need a bipap to overcome the weight on the chest....ie much higher pressures are needed. I have personally got the pressure up to 27/21 for one patient.
I guess you do what you have to do for your health but I still astonished that that could work at that high of a pressure.
49er
_________________
| Mask: SleepWeaver Elan™ Soft Cloth Nasal CPAP Mask - Starter Kit |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Use SleepyHead |
- Sheriff Buford
- Posts: 4110
- Joined: Mon Aug 09, 2010 8:01 am
- Location: Kingwood, Texas
Re: How Do You Know if You Need BiPap?
To tag on to 49er's comment: Resmed offers the EPR mode. Isn't this what a Bipap machine does? What's the difference? Sheriff
_________________
| Machine: AirSense 11 Autoset |
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
Re: How Do You Know if You Need BiPap?
EPR is slightly different than the bilevel pressures of a bilevel machine. It's close but the timing is a bit different.Sheriff Buford wrote:To tag on to 49er's comment: Resmed offers the EPR mode. Isn't this what a Bipap machine does? What's the difference? Sheriff
EPR only goes to 3 cm difference. Bilevel machines allow for a much larger difference than 3 cm between inhale and exhale.
So while similar in function by varying the inhale (IPAP) and exhale (EPAP) pressures it is a bit different. Not exactly the same thing. Though I often tell S9 users to try EPR at 3 to get a feel for what Bilvel might feel like. It's close.
I have tried my VPAP in CPAP mode with EPR of 3 cm (only place EPR is available on ResMed's bilevel machine...called VPAP) and the VPAP with Pressure support of 3 and while it feels very similar the timing is a bit different. To me the VPAP with pressure support feels like it waits better for me to breathe. A timing thing. Not a huge difference but a difference. It's really hard to describe.
Most people using bilevel machine will need/want at least 4 cm difference and in some situations much higher differences. EPR only goes to 3 cm. Also, Respironics machines with the various Flex exhale relief. Totally different animals. The amount of reduction is based upon flow so a setting of 3 is extremely unlikely to produce a 3 cm reduction. The reductions are much less and the relief is afforded by the breathing rhythm and air flow based timing of the slight reduction that is offered.
Need2snooze...
See this link for my bilevel story. Never had a problem exhaling against my pressures, never had much of an aerophagia issue yet I do sleep better on a bilevel machine. Sleeping better equates into feeling better for me. Skip over the heated hose stuff.
viewtopic/t71442/viewtopic.php?f=1&t=71 ... te#p656179
Will bilevel be better for everyone? Of course not. It's just like everything else related to cpap ...YMMV.
_________________
| Machine: AirCurve™ 10 VAuto BiLevel Machine with HumidAir™ Heated Humidifier |
| Additional Comments: Mask Bleep Eclipse https://bleepsleep.com/the-eclipse/ |
I may have to RISE but I refuse to SHINE.
- Denial Dave
- Posts: 1335
- Joined: Wed Sep 19, 2012 6:45 am
- Location: Connecticut
Re: How Do You Know if You Need BiPap?
COPD and other health issues aside
my understanding from an article from the Journal of Clinical Medicine / Sleep Study.
During the sleep study / titration, the max level of CPAP is 15 cm H20. Unless the patient can has difficulties tolerating pressures above 10 cm H20
after that, BiPap is to be prescribed.
As Pugsy indicated, the minumum differential between IPAP and EPAP is 4....
If more than 2 obstructions are observed during a minimum set time period, pressures are slowly increased by 1cm.
The goal is no more than one obstruction per hour or if possible the complete elimination of them.
Dave
my understanding from an article from the Journal of Clinical Medicine / Sleep Study.
During the sleep study / titration, the max level of CPAP is 15 cm H20. Unless the patient can has difficulties tolerating pressures above 10 cm H20
after that, BiPap is to be prescribed.
As Pugsy indicated, the minumum differential between IPAP and EPAP is 4....
If more than 2 obstructions are observed during a minimum set time period, pressures are slowly increased by 1cm.
The goal is no more than one obstruction per hour or if possible the complete elimination of them.
Dave
_________________
| Mask: Mirage Quattro™ Full Face CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Started at VPAP pressure setting of 20/14.4. I've survived Stage 1 cancer and lost 80+ lbs. Pressure is now 14.5 / 11 |
if you don't know where you are going... any road will take you there.... George Harrison
- ChicagoGranny
- Posts: 15158
- Joined: Sun Jan 29, 2012 1:43 pm
- Location: USA
Re: How Do You Know if You Need BiPap?
My doctor says BiPAP is indicated for patients who require pressure of 14 cm or higher. You will find many sleep doctors following this general guideline.need2snooze wrote:In my quest to find that elusive night of wonderful, rested sleep after over four years of CPAP, I'm wondering if I'm using the right machine - S9 Autoset. My dr. has never suggested it, but I'm curious about BiPap. Is it only for people who need high pressure settings b/c of high AHI numbers? Could BiPap possibly help with the aerophagia and sleeping better through the night?
BTW, high pressure settings and high AHI numbers are not well correlated. You can have low AHI and require a high pressure or you could have AHI and only need a low pressure.
"It's not the number of breaths we take, it's the number of moments that take our breath away."
Cuando cuentes cuentos, cuenta cuántas cuentos cuentas.
Cuando cuentes cuentos, cuenta cuántas cuentos cuentas.
-
need2snooze
- Posts: 60
- Joined: Fri Apr 27, 2012 8:13 pm
Re: How Do You Know if You Need BiPap?
Thanks, everyone! Pugsy, I read your link. Very informative. I'll need to read it again when I've had more than two hours of sleep (rough night last night - don't know why). Per your suggestion, and that of others, I've been trying different setting changes over the past several months. I reset the EPR setting from 1 to 3. That seemed to help some. In looking over my Sleepyhead data over the past several months, when I had the EPR setting on 1, my Flow Limit number averaged at a higher number, 14, 18, 19. When I changed the EPR to 3, that Flow Limit number has steadily been below 10 (at the 95% level). Also, when the EPR was at 1, the Respiratory Rate number was higher, around 20; now it is 16-18. I noticed on your link that you talk about how easy it is to breathe. I just went and put my mask on to see how I really feel when I'm breathing through it, as I'm usually fumbling around getting ready to go to sleep and not thinking that much about how my breathing feels. What I noticed is that I feel more resistance trying to breathe in, as opposed to exhaling. I like the Mirage FX for Her mask, but I do feel "stuffy" with it, like I'm not getting as much air as I would like.
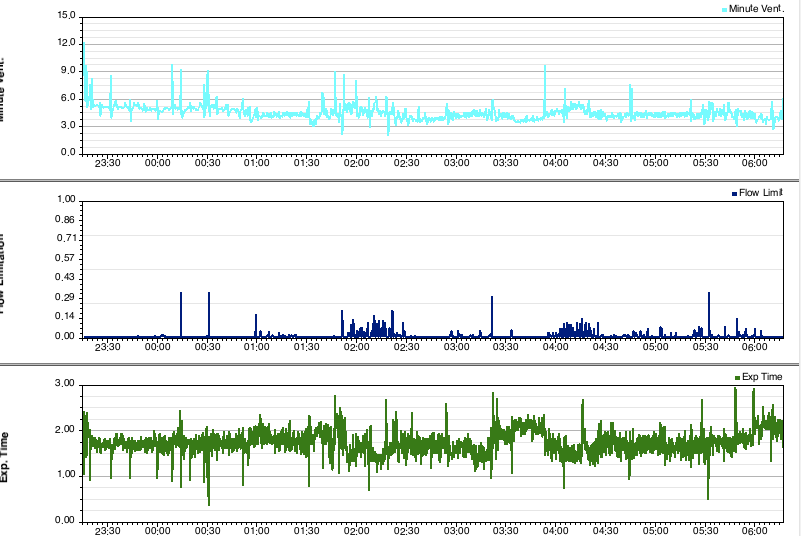
Here is a typical night for me, except that it appears I got several hours of sleep. Although the numbers may look decent, I always feel tired the next day.
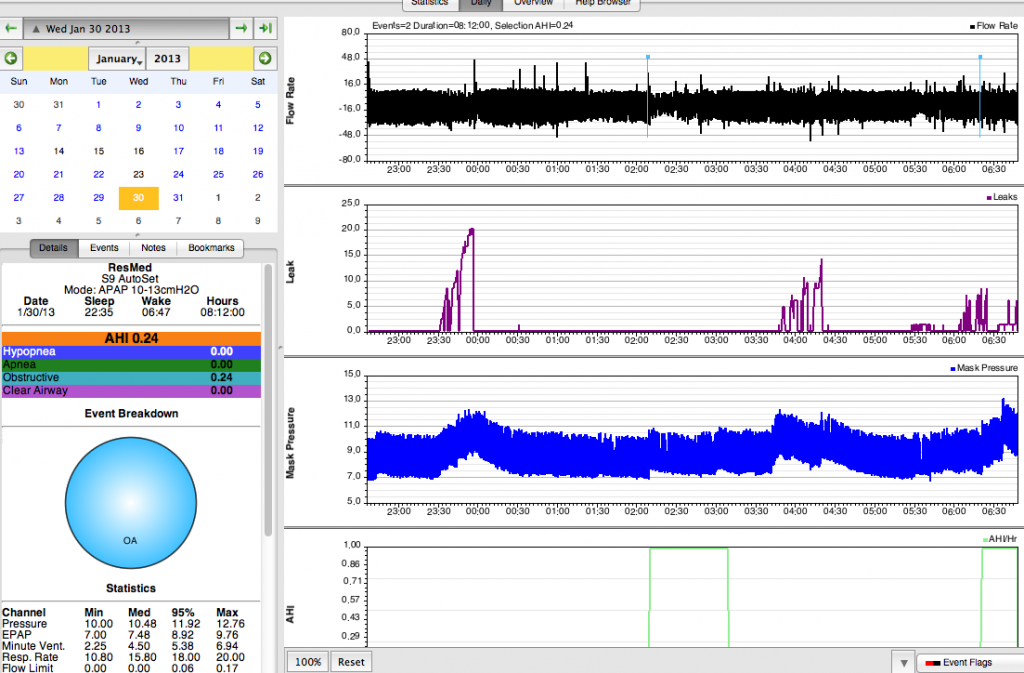
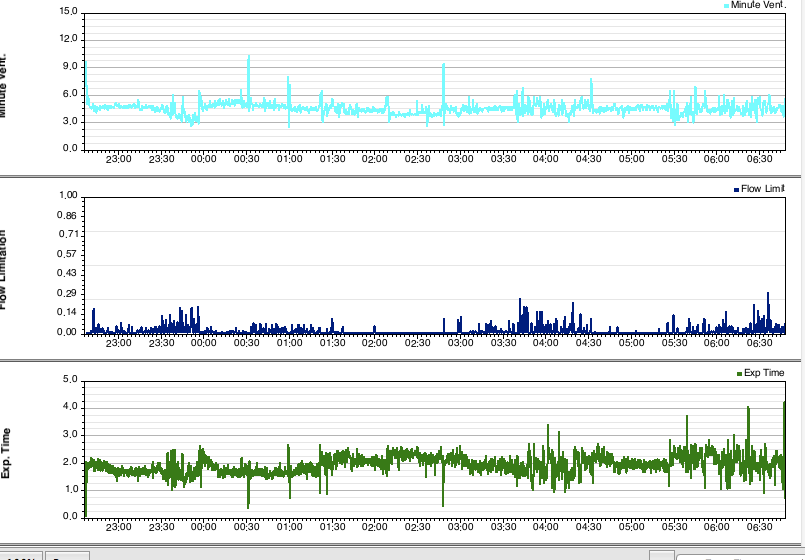
Here is a typical night for me, except that it appears I got several hours of sleep. Although the numbers may look decent, I always feel tired the next day.
_________________
| Mask: Mirage™ FX For Her Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
Re: How Do You Know if You Need BiPap?
Hi,
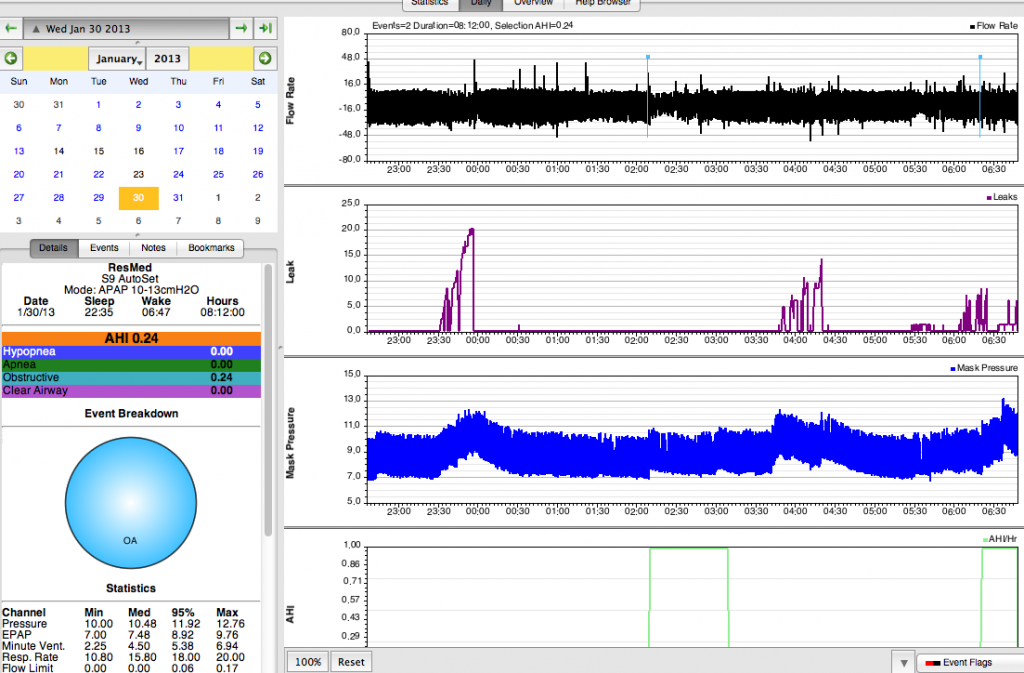
It is interesting that you are recording almost no events, yet are not sleeping well. I also see that your machine is not adjusting upwards except when you have leaks, so your machine is not seeing any issues other than the two events that were recorded. Does your sleep doctor have any ideas?
I went through that much of last year where RERA breathing (USARS) was disrupting my sleep. I would show no events, but still not sleep well. The solution was a higher fixed pressure. Due to body changes, that issue has vastly diminished. An indicator of this issue would be if you had a sleep study, and they computed an RDI index, and that RDI index was much higher than your AHI.
There are other sleep disorders out there that show up as poor sleep but few events. I wonder if it would be good to press your doctor (or a new doctor) for a follow-up sleep study to diagnose what exactly is messing up your sleep when you are using the CPAP machine.
-john-
It is interesting that you are recording almost no events, yet are not sleeping well. I also see that your machine is not adjusting upwards except when you have leaks, so your machine is not seeing any issues other than the two events that were recorded. Does your sleep doctor have any ideas?
I went through that much of last year where RERA breathing (USARS) was disrupting my sleep. I would show no events, but still not sleep well. The solution was a higher fixed pressure. Due to body changes, that issue has vastly diminished. An indicator of this issue would be if you had a sleep study, and they computed an RDI index, and that RDI index was much higher than your AHI.
There are other sleep disorders out there that show up as poor sleep but few events. I wonder if it would be good to press your doctor (or a new doctor) for a follow-up sleep study to diagnose what exactly is messing up your sleep when you are using the CPAP machine.
-john-
-
need2snooze
- Posts: 60
- Joined: Fri Apr 27, 2012 8:13 pm
Re: How Do You Know if You Need BiPap?
That's interesting about the RDI index. I'll have to see if it was done when I did my sleep study. Haven't heard of it before. My doctor is not willing to order me another sleep study b/c my AHI numbers are so good. I regularly wake up after having slept four hours, regardless how tired I was when I went to sleep. I may or may not be able to go right back to sleep. Sometimes, I wake up again after another hour or two. What I want to figure out is if I am waking up because of something insomnia related, or if a breathing event is causing me to wake up, although not necessarily an OSA event. I don't know much about the Sleepyhead data to know really what I'm looking at, though. Would that show up on Flow Limitation, for instance, or somewhere else? If someone can tell me that, and I can establish a pattern with my data, then I can show my dr. and hopefully get another sleep study, or maybe a different machine will do the trick.
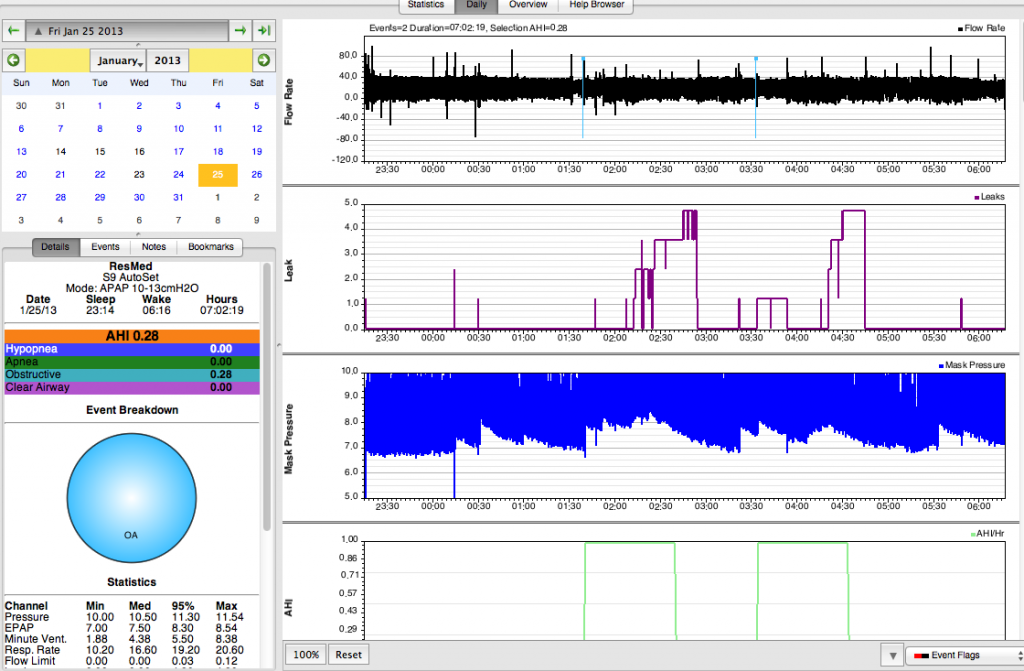
I should have posted this data earlier, as this is a more typical night's sleep for me, although some nights I may have only an hypopnea, or an obstructive, or the variety plate of three different kinds of events. Even so, my AHI rarely goes over one. Again, I wake up after about 4 hours of sleep and may or may not be able to go back to sleep quickly. This night I did go back to sleep easily. Thanks for taking a look and any suggestions you can give me.
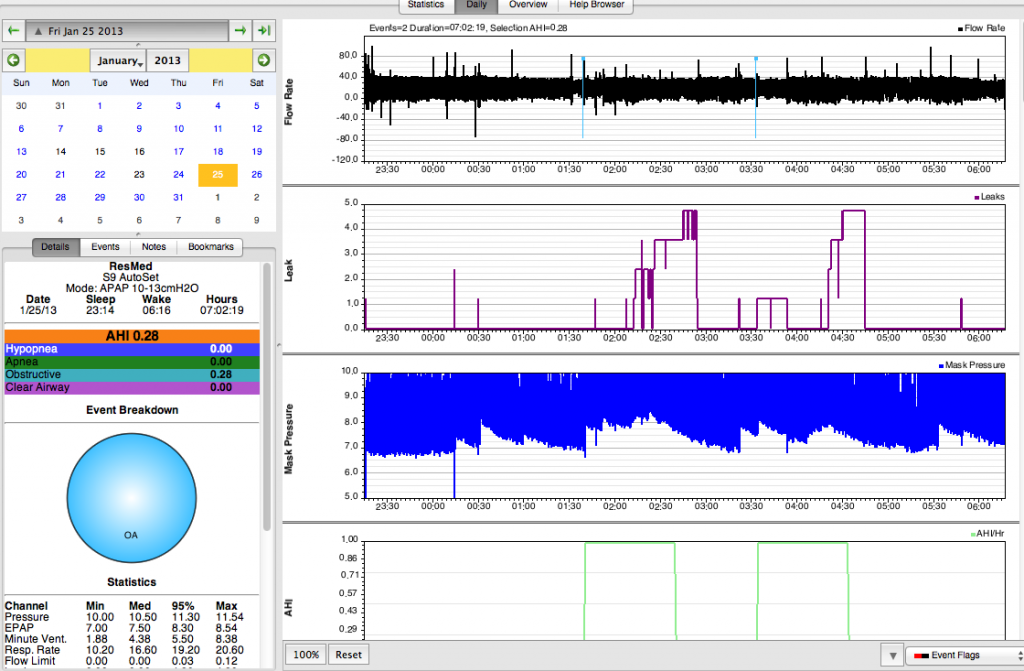
I should have posted this data earlier, as this is a more typical night's sleep for me, although some nights I may have only an hypopnea, or an obstructive, or the variety plate of three different kinds of events. Even so, my AHI rarely goes over one. Again, I wake up after about 4 hours of sleep and may or may not be able to go back to sleep quickly. This night I did go back to sleep easily. Thanks for taking a look and any suggestions you can give me.
_________________
| Mask: Mirage™ FX For Her Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
Re: How Do You Know if You Need BiPap?
You can try creating some sort of break in the therapy line when you wake up so you can look for something maybe happening just prior to the awakening. If you wake up then reach over and turn the machine off and then back on again. That way you have a break in the therapy line. Maybe be able to zoom in and see some sort of pattern.need2snooze wrote:What I want to figure out is if I am waking up because of something insomnia related, or if a breathing event is causing me to wake up, although not necessarily an OSA event.
Though you know it might just be sleep maintenance insomnia that is totally unrelated to sleep apnea.
Do you take any meds that might mess with sleep architecture?
Any pain issues?
Your leak line is so good I am green with envy. I don't know enough about what the Flow limitation graphs on the ResMed machine might mean in terms of FLs being present in such a fashion as to cause a wake up.
_________________
| Machine: AirCurve™ 10 VAuto BiLevel Machine with HumidAir™ Heated Humidifier |
| Additional Comments: Mask Bleep Eclipse https://bleepsleep.com/the-eclipse/ |
I may have to RISE but I refuse to SHINE.