Now with a reduced Flex setting
Re: Now with a reduced Flex setting
Night six:
Still C-Flex+ 1.
I got to bed a fair bit later than usual.
Once more I woke up, turned off the machine, yanked off the mask, only to put everything back on again a few seconds later. I have no idea why I'm doing this.
For what I think is the second time since I switched to this Flex setting, I've seen a leak line that does not match my historical leak lines.
Still C-Flex+ 1.
I got to bed a fair bit later than usual.
Once more I woke up, turned off the machine, yanked off the mask, only to put everything back on again a few seconds later. I have no idea why I'm doing this.
For what I think is the second time since I switched to this Flex setting, I've seen a leak line that does not match my historical leak lines.
_________________
| Mask: AirFit™ P10 For Her Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Software: SleepyHead, loosely following HEAD |
Re: Now with a reduced Flex setting
Some Zeo Sleep Graphs? I ended up generating the graphs myself, using the same basic conventions as the Zeo. My offlineness lends itself to the graphs being generated by a script of my own, using the same basic conventions as the standard graphs, with some differences, such as each horizontal pixel corresponds to 30s.deltadave wrote: Can you post some Zeo Sleep Graphs?
Day 0: Last day of C-Flex+ 3


Day 1: Now at C-Flex+ 1


Day 2:


Day 3:


Day 4:


Day 5:


Day 6:


_________________
| Mask: AirFit™ P10 For Her Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Software: SleepyHead, loosely following HEAD |
Re: Now with a reduced Flex setting
ASSESSMENT OF A WIRELESS DRY SENSOR TO DETECT SLEEP IN HEALTHY VOLUNTEERS AND SUBJECTS WITH SLEEP DISORDERS
Blake S,, Pittman SD, MacDonald MM, Sun K, Lanzi B, Clark D, Hueser L, Fabregas SE, Shambroom JR, White DP
Philips Home Healthcare Solutions (Philips Respironics), Boston, MA, USA, Sleep HealthCenters, Boston, MA, USA, Zeo, Inc (formerly Axon Labs, Inc), Newton, MA, USA
Introduction: A simple, easy-to-use portable device to detect sleep stages could have many applications in sleep research and clinical practice. We assessed a device with dry fabric sensors that require no skin preparation and are integrated into a simple headband for wireless transmission to a separate bedside monitor. Sleep stages are scored automatically by a neural network. Our aim was to compare sleep scored by the wireless system (WS) to manual scoring of concurrent polysomnography (PSG) in both healthy volunteers and subjects with sleep disorders (obstructive sleep apnea (OSA) and insomnia).
Methods: 30 subjects (10 healthy volunteers, 10 OSA patients, 10 insomniacs) participated. Each subject was setup for a standard PSG and the investigational wireless system for concurrent overnight recordings in our sleep laboratory. WS data were sampled by a 12-bit A-D for automated scoring of 30-second epochs of Wake, Light Sleep (N1+N2), Deep Sleep (N3), and REM sleep. Each PSG record was manually scored using recommended AASM criteria by 2 registered sleep technologists blinded to the results of the wireless system (M1 and M2). Sleep onset latency to 10 minutes of persistent sleep (LPS), total sleep time (TST), and sleep efficiency (SE) were derived from the records for comparison in addition to sleep stage agreement and Cohen’s κ using a confusion matrix.
Results: PSG and WS data were available for 29 subjects for a total of 24,138 epochs. Sleep staging (all subjects) agreements/κ were: WS-M1: 68%/0.50, WS-M2: 68%/0.48, M1-M2: 88%/0.79. Sleep staging (healthy volunteers, n=10) agreements/κ were WS-M1: 73%/0.58, WSM2: 72%/0.51, M1-M2: 89%/0.81. Sleep staging (sleep disordered subjects, n=19) agreements/κ were WS-M1: 65%/0.45, WS-M2: 66%/0.44, M1-M2: 88%/0.81. Mean LPSs (all subjects) were WS: 15±14, M1: 48±83, M2: 48±84 minutes. Mean TSTs (all subjects) were WS: 349±76, M1: 331±84 and M2 329±89 minutes. Mean SEs (all subjects) were WS: 86±17%, M1: 79±19% and M2: 79±20%.
Conclusion: Results for healthy volunteers were consistent with previous findings demonstrating reasonable correlation with full PSG. The device performed better on healthy volunteers than on sleep disordered subjects. The system shows promise as an easy to use wireless system for recording and scoring sleep.
Support (optional): Support for this study provided by Philips Respironics. Wireless Systems were kindly provided by Zeo, Inc (formerly Axon Labs, Inc)
Blake S,, Pittman SD, MacDonald MM, Sun K, Lanzi B, Clark D, Hueser L, Fabregas SE, Shambroom JR, White DP
Philips Home Healthcare Solutions (Philips Respironics), Boston, MA, USA, Sleep HealthCenters, Boston, MA, USA, Zeo, Inc (formerly Axon Labs, Inc), Newton, MA, USA
Introduction: A simple, easy-to-use portable device to detect sleep stages could have many applications in sleep research and clinical practice. We assessed a device with dry fabric sensors that require no skin preparation and are integrated into a simple headband for wireless transmission to a separate bedside monitor. Sleep stages are scored automatically by a neural network. Our aim was to compare sleep scored by the wireless system (WS) to manual scoring of concurrent polysomnography (PSG) in both healthy volunteers and subjects with sleep disorders (obstructive sleep apnea (OSA) and insomnia).
Methods: 30 subjects (10 healthy volunteers, 10 OSA patients, 10 insomniacs) participated. Each subject was setup for a standard PSG and the investigational wireless system for concurrent overnight recordings in our sleep laboratory. WS data were sampled by a 12-bit A-D for automated scoring of 30-second epochs of Wake, Light Sleep (N1+N2), Deep Sleep (N3), and REM sleep. Each PSG record was manually scored using recommended AASM criteria by 2 registered sleep technologists blinded to the results of the wireless system (M1 and M2). Sleep onset latency to 10 minutes of persistent sleep (LPS), total sleep time (TST), and sleep efficiency (SE) were derived from the records for comparison in addition to sleep stage agreement and Cohen’s κ using a confusion matrix.
Results: PSG and WS data were available for 29 subjects for a total of 24,138 epochs. Sleep staging (all subjects) agreements/κ were: WS-M1: 68%/0.50, WS-M2: 68%/0.48, M1-M2: 88%/0.79. Sleep staging (healthy volunteers, n=10) agreements/κ were WS-M1: 73%/0.58, WSM2: 72%/0.51, M1-M2: 89%/0.81. Sleep staging (sleep disordered subjects, n=19) agreements/κ were WS-M1: 65%/0.45, WS-M2: 66%/0.44, M1-M2: 88%/0.81. Mean LPSs (all subjects) were WS: 15±14, M1: 48±83, M2: 48±84 minutes. Mean TSTs (all subjects) were WS: 349±76, M1: 331±84 and M2 329±89 minutes. Mean SEs (all subjects) were WS: 86±17%, M1: 79±19% and M2: 79±20%.
Conclusion: Results for healthy volunteers were consistent with previous findings demonstrating reasonable correlation with full PSG. The device performed better on healthy volunteers than on sleep disordered subjects. The system shows promise as an easy to use wireless system for recording and scoring sleep.
Support (optional): Support for this study provided by Philips Respironics. Wireless Systems were kindly provided by Zeo, Inc (formerly Axon Labs, Inc)
...other than food...
Re: Now with a reduced Flex setting
Anyway...
Most often, even bad sleepers will put together long stretches of continuous sleep, and "IMHO", the WS algorithm will have a very high degree of accuracy in correctly identifying sleep stages during those periods.
Further, if the "2 registered sleep technologists" agreement is only 88%, I'm kinda lookin' at that with a little bit of suspicalism (i.e., if SS Agreement was more like the 92%+ it should be, then that 65-66% would be lookin' real bad).
Anyway...
So if the stretches of continuous sleep have near 100% accuracy, then that would mean that one would have basically a 50-50 shot of being correct in disturbed sleep, and looking at Zeo graphs in disturbed sleep should not be taken as The Gospel.
Most often, even bad sleepers will put together long stretches of continuous sleep, and "IMHO", the WS algorithm will have a very high degree of accuracy in correctly identifying sleep stages during those periods.
Further, if the "2 registered sleep technologists" agreement is only 88%, I'm kinda lookin' at that with a little bit of suspicalism (i.e., if SS Agreement was more like the 92%+ it should be, then that 65-66% would be lookin' real bad).
Anyway...
So if the stretches of continuous sleep have near 100% accuracy, then that would mean that one would have basically a 50-50 shot of being correct in disturbed sleep, and looking at Zeo graphs in disturbed sleep should not be taken as The Gospel.
...other than food...
Re: Now with a reduced Flex setting
Also, you look like you're on a REM-wrecking drug. Which is it?
...other than food...
Re: Now with a reduced Flex setting
All I'm taking is iron, which is not currently low, nor was it low during any of my sleep studies. It was a touch low a year ago, and I'm hoping to get off it soon.deltadave wrote:Also, you look like you're on a REM-wrecking drug. Which is it?
_________________
| Mask: AirFit™ P10 For Her Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Software: SleepyHead, loosely following HEAD |
Re: Now with a reduced Flex setting
Normal REM Latency should be about 90 minutes. Given the NPSG Latencies (333.5 minutes and 172.0 minutes) and if we are to give Zeo any credibility, that certainly is an area that deserves exploring.tetragon wrote:All I'm taking is iron, which is not currently low, nor was it low during any of my sleep studies. It was a touch low a year ago, and I'm hoping to get off it soon.deltadave wrote:Also, you look like you're on a REM-wrecking drug. Which is it?
Returning to Architecture 101:

Sleep progresses from Wake, through light sleep (Stage 1 and 2), followed by deep sleep (Stages 3 & 4, now collectively referred to as NREM3 or SWS)(I gotta build a new graph one of these days), and finally a REM period. This is one Sleep Cycle and takes about 90 minutes to complete. There are usually 4-6 Sleep Cycles per night. Most deep or delta sleep occurs in the first Sleep Cycle. The duration of REM periods increase as the night goes on.
...other than food...
Re: Now with a reduced Flex setting
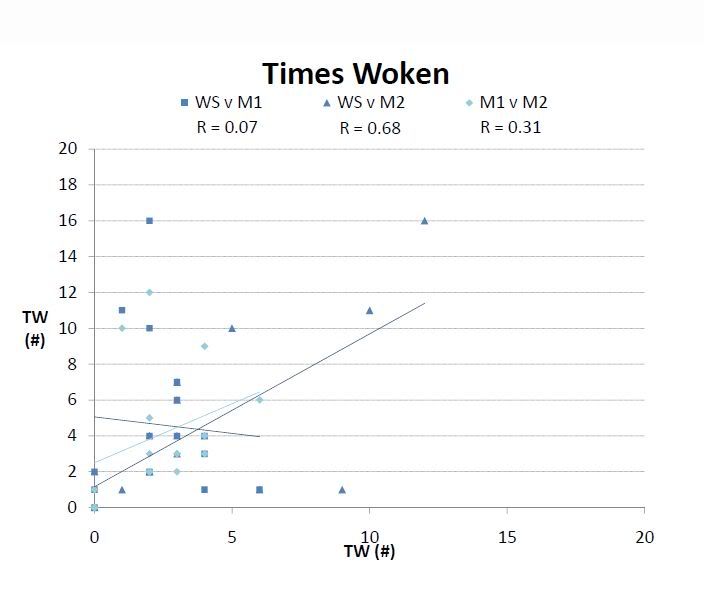
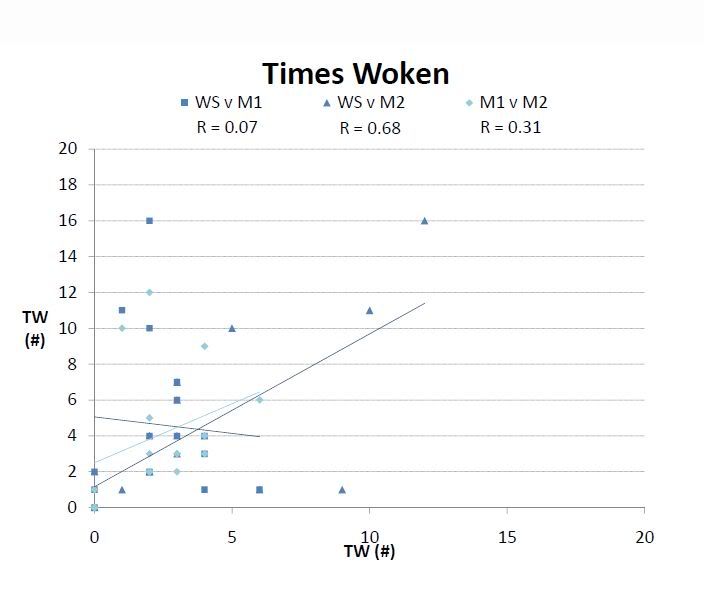
And boy, I tell ya, in
http://www.myzeo.com/sleep/sites/defaul ... poster.pdf
determining Times Woken, ya might as well just throw darts:
http://www.myzeo.com/sleep/sites/defaul ... poster.pdf
determining Times Woken, ya might as well just throw darts:
...other than food...
Re: Now with a reduced Flex setting
Night 7:
C-Flex+ 1.
Nothing terribly interesting about that night. Sure it was a bit shorter than usual, but it was for the same reason as night six: my friends have horrible taste in when to meet up. I have also realized that my non-work life still revolves around coffee shops and espresso bars, even though I no longer drink the stuff on an everyday basis.
Over the past week, I've gone from being uncomfortable in the morning to not noticing any consequences to the setting of C-Flex+ 1. Now to decide what to do with that setting for the next week. Will I keep it the same or see what the older C-Flex feels like?
C-Flex+ 1.
Nothing terribly interesting about that night. Sure it was a bit shorter than usual, but it was for the same reason as night six: my friends have horrible taste in when to meet up. I have also realized that my non-work life still revolves around coffee shops and espresso bars, even though I no longer drink the stuff on an everyday basis.
Over the past week, I've gone from being uncomfortable in the morning to not noticing any consequences to the setting of C-Flex+ 1. Now to decide what to do with that setting for the next week. Will I keep it the same or see what the older C-Flex feels like?
_________________
| Mask: AirFit™ P10 For Her Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Software: SleepyHead, loosely following HEAD |
Re: Now with a reduced Flex setting
So, my REM may not be what it should, and if it is screwed up it's probably not what I'm taking?deltadave wrote:Normal REM Latency should be about 90 minutes. Given the NPSG Latencies (333.5 minutes and 172.0 minutes) and if we are to give Zeo any credibility, that certainly is an area that deserves exploring.tetragon wrote:All I'm taking is iron, which is not currently low, nor was it low during any of my sleep studies. It was a touch low a year ago, and I'm hoping to get off it soon.deltadave wrote:Also, you look like you're on a REM-wrecking drug. Which is it?
_________________
| Mask: AirFit™ P10 For Her Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Software: SleepyHead, loosely following HEAD |
Re: Now with a reduced Flex setting
I do not understand the question.tetragon wrote:So, my REM may not be what it should, and if it is screwed up it's probably not what I'm taking?
...other than food...
Re: Now with a reduced Flex setting
It is what happens if I forget to think, and re-read a couple minutes later, before I post. Now I need to figure out what I meant.deltadave wrote:I do not understand the question.tetragon wrote:So, my REM may not be what it should, and if it is screwed up it's probably not what I'm taking?
_________________
| Mask: AirFit™ P10 For Her Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Software: SleepyHead, loosely following HEAD |
Re: Now with a reduced Flex setting
tetragon wrote:deltadave wrote:tetragon wrote:So, my REM may not be what it should, and if it is screwed up it's probably not what I'm taking?
I do not understand the question.
It is what happens if I forget to think, and re-read a couple minutes later, before I post. Now I need to figure out what I meant.
Y'know, "they" say that REM is important for memory consolidation...
...other than food...
Re: Now with a reduced Flex setting
OK, no time like the present...deltadave wrote:(I gotta build a new graph one of these days)
Here's a new Sleep Architecture using the 2008 nomenclature:

...other than food...









