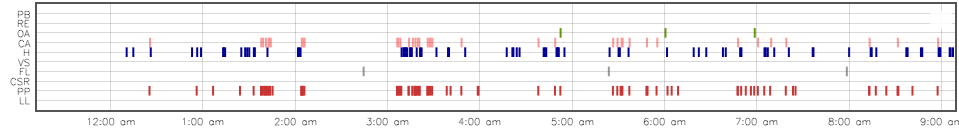
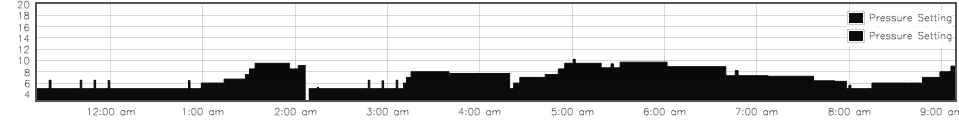
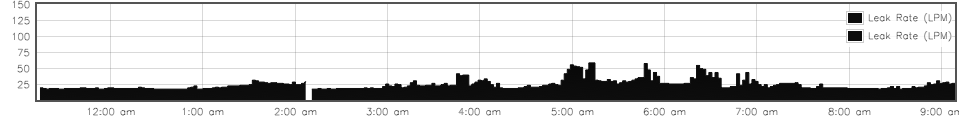
avi123 wrote:Thanks DSM. Please check where I stand now with reference to identifying Periodic Breathing from the Flow graphs obtained by ResScan from Resmed S9 Autoset and S9 Elite. The two machines are using similar technology.
See it on page 5 here:
viewtopic/t66572/viewtopic.php?f=1&t=66 ... 59#p620059
The idea is to scan the Flow graph over time (horizontally) and check for repeats of the comlpexes that are unique to PB and CSR.
This is my source of info regarding the CSR lengths of the cycles:
Central Sleep Apnea and Cheyne-Stokes Respiration
Dai Yumino1,2 and T. Douglas Bradley1,2,3
http://pats.atsjournals.org/cgi/reprint/5/2/226
Read the info about CSR on pg 228
I am not familiar with Respironics machines. So I rather stay away from rendering comments on their graphs.
Regards.
Avi
Avi
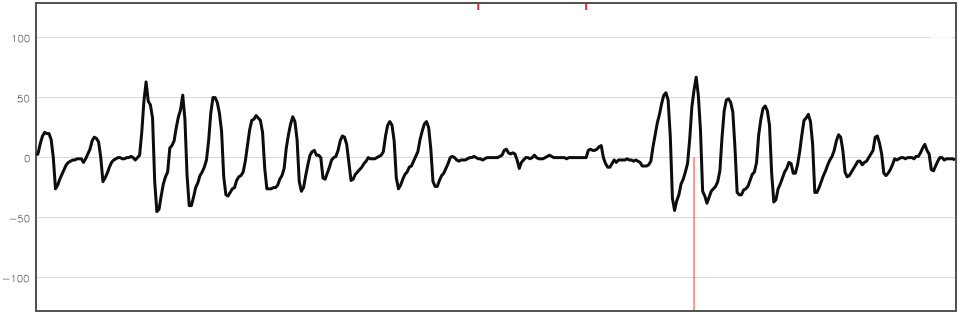
Tks for the links - it clarifies your POV. That paper by Dai Yumino1,2 and T. Douglas Bradley was familiar to me & have always considered it to be very helpful. I have reproduced (below) their illustration from page 228 because it was what you highlighted.
Firstly to establish common ground I am sure we all agree that CSR & PB are patterns of 'cyclic respiration' (
periods of
breathing interspersed with central apneas and/or central hypopneas). And it is agreed that CSR is a pattern where the cycles (consisting of a number of breaths + apnea) are usually observed as occurring around every 2 mins or so and illustrate steadily increasing respiration followed by steadily decreasing respiration followed by apnea (or apnea followed by the pattern - either view is ok). I previously made refs to sub 3-min cycles because I know that ASV machines (originally designed just for CSR) were designed to respond to cyclic breathing patterns that are under 3 mins in duration.
The image below was being used in the linked to paper to illustrate (
using a single cycle of the breathing pattern) the difference between an 'idopathic' central apnea and a central apnea resulting from Cheynes-Stokes respiration. From the side box you can read that they placed an SpO2 probe at the patients ear to best approximate the blood O2 levels at the same distance to where the chemoreceptors are from the lungs and thus the probes SpO2 readings will more closely reflect what the chemoreceptors see of the CO2 levels in the blood. The blood CO2 level is what will drive respiration & that drive or lack of it, subsequently impacts the blood O2 level. i.e. Hypocapnia (too little CO2 in the blood) slows breathing which means less oxygen is being picked up in the lungs.
Adequate O2 in the blood is what nourishes the cells in the body & brain.
The main points I got from this were
1) the different effects on respiration - see in the diag CSR respiration steadily rising then falling in that cycle where the apnea duration is A=>B (21secs) and respiration is B=>D (46secs) vs the CA cycle where the apnea duration is A=>B (18 secs) and respiration is B=>D (7 secs). In particular the effect of blood oxygen - the SpO2 in CSR reaches its lowest point at C whereas in the CA cycle C is much later in the cycle.
2) The actual respiration patterns are quite different
Just to summarize their observations re CSR ...
>>
In patients with HF and CSR, the periodic cycle duration averaged approximately 60 seconds, similar to that described by Cheyne, compared with only 35 seconds in patients with idiopathic CSA or high-altitude periodic breathing without HF (18, 28). Thus it is the presence of a prolonged hyperpnea with a waxing-waning pattern of tidal volume, and prolonged cycle duration, that distinguishes CSR from other forms of periodic breathing. Therefore, if the term ‘‘Cheyne-Stokes respiration’’ is to have any distinctive meaning, its use should be confined to periodic breathing in which the hyperpnea and cycle durations are prolonged. Since this pattern is characteristic of prolonged lung to chemoreceptor circulation time, it appears to be a manifestation of a low cardiac output as one would observe in patients with HF or bradyarrhythmias.
<<
(DSM NOTE: where hyperpnea means increased depth of breathing (opposite to hypopnea) when required to meet metabolic demand of body tissues)
#2 It is probably fair to say that PB (Periodic Breathing) really has become the alternate name for CSA (Central Sleep Apnea). By this I am saying that PB is periods of breathing interspersed with central apneas. A CA on its own can be quite normal so how do we differentiate a bad CA from a benign one ? - answer has to be when there is
repeated Periodic Breathing resulting in SpO2 desats. So when a patient is said to have CSA (vs OSA) they can also be said to be having Periodic Breathing. It may be a moot point but I think it may help people understand just what is really meant by PB.
Cheers DSM