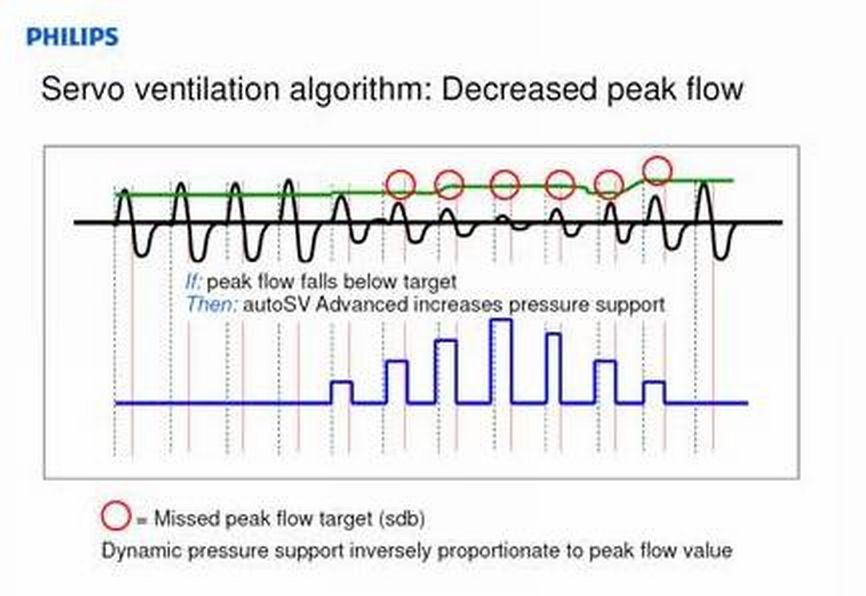
I agree. The ASV part of the algorithm above is probably not going to treat UARS---based on RERA occurring before sufficient volume reduction has occurred. And I don't see where the EPAP-adjusting treatment arms in either brand ASV will avoid UARS RERA's significantly better than ordinary APAP algorithms. As a result, I envision Dr. Krakow's UARS patients still leaving NPSG with high PS min values. I think Dr. Guilleminault still prefers ordinary CPAP for his UARS patients. I suppose two germane questions for any UARS patient is: 1) where is threshold of arousal relative to perfect sinusoid, but more importantly 2) what pressure settings are sufficient to avoid RERA? Unfortunately, iatrogenic problems can offset the intended benefits of those high pressures.mollete wrote:So it strikes me that it would only work when one's baseline peak flow is normal (and one has real "peaks"):-SWS wrote:Respironics ASV targets 95% of recent-averaged peak flow...
However, if one's baseline is flow-limited, the most one could hope for is 95% of that, which may not attain "normalcy".
Perhaps one could hope that the ASV would see a failure to respond to PS and identify the event as obstructive-- however, the PR ASV response to obstruction is raise EPAP (that's the only thing it can do to correct the underlying issue), and not simply chase it all night long.
Which is why I contend that an AutoAnythingElse algorithm is better suited to attack obstructions (i.e., look for snores and flow-limitations, positive response to pressure increases, etc.).
ASV users: the everything ASV thread.
Re: ASV users: the everything ASV thread.
Re: ASV users: the everything ASV thread.
Adding this from a Guide:-SWS wrote: The Ti setting specifies the maximum time allowed for inspiration----from 0.5s to 3.0s in 0.1s increments. However, this parameter is automatically maintained (and not user adjustable) when the backup rate is set to auto.
A Ti limit is typically calculated using spontaneous BPM and I:E ratio.
"The inspiratory time and breath rate controls are linked so the inspiratory time never exceeds the expiratory time. If the breath rate or inspiratory time are set to values that would cause the I:E ratio to exceed 1:1, the inspirator ytime is automatically reduced to maintain a 1:1 I:E ratio."
1- when the BPM is set to auto:
If I understand, the expiratory time must always be larger than the inspiratry time; am I correct to understand that within this constraint however, the Ti will increase when the I:E ratio increases?
-- so, to obtain a longer inspiratory time (as in, trying to reach the upper limit of 3.0s), one could elicit that by exhaling for a longer time?, (which is possible to do as an exercise, during the pre-sleep conscious phase?)
2- when the BPM is set to manual:
how does the ASV determine the Ti value to deliver (except for preventing it from overshooting the limit set)?
3- to complete a better understanding of #1 process above, adding the BPM factor
do you know how does it use the BPM in this calculation?-SWS wrote: A Ti limit is typically calculated using spontaneous BPM and I:E ratio.
_________________
| Mask: Wisp Nasal CPAP Mask with Headgear - Fit Pack |
| Humidifier: DreamStation Heated Humidifier |
PR Dreamstation BiPap ASV, WISP nasal mask with magnets
Re: ASV users: the everything ASV thread.
The above text refers to the clinician's procedure of programming the BPM and Ti values into the machine. As an example, if a clinician entered a Ti value of 3.0, and then entered BPM of 15, then the machine would correct the programming error. The machine would automatically change Ti to 2.0s.4betterO2 wrote: Adding this from a Guide:
"The inspiratory time and breath rate controls are linked so the inspiratory time never exceeds the expiratory time. If the breath rate or inspiratory time are set to values that would cause the I:E ratio to exceed 1:1, the inspiratory time is automatically reduced to maintain a 1:1 I:E ratio."
When BPM is set to auto, the machine uses a recent average of spontaneous breathing periods (reciprocal of averaged frequency) toward an auto-BPM value. Similarly, the algorithm uses a recent average of spontaneous inspiratory time toward an auto-Ti value. I think the machine's recent-averaging will discount anomalies such as "burst breathing" or small volumes immediately prior to central apneas. I'm not sure if the auto-backup algorithm will impose that same 1:1 rule against the recent-averaged Ti target. But I'd also guess, as you did, that the same rule is imposed here as well.4betterO2 wrote:1- when the BPM is set to auto:
If I understand, the expiratory time must always be larger than the inspiratry time; am I correct to understand that within this constraint however, the Ti will increase when the I:E ratio increases?
-- so, to obtain a longer inspiratory time (as in, trying to reach the upper limit of 3.0s), one could elicit that by exhaling for a longer time?, (which is possible to do as an exercise, during the pre-sleep conscious phase?)
When BPM is set to manual, the BPM and Ti values are cut-and-dry. The machine uses the BPM and Ti values programmed into the machine by the clinician or user. At that point IPAP is delivered for Ti seconds throughout each machine-delivered breath. I originally said Ti was an upper limit. But after scouring through an older Respironics document, I think that was wrong. It looks as if Ti will not come into play at all during spontaneous breaths----and that Ti will be delivered as a fixed value (rather than upper limit) during all backed or machine-cycled breaths. Again, that was my mistake several posts up, and I apologize.4betterO2 wrote: 2- when the BPM is set to manual:
how does the ASV determine the Ti value to deliver (except for preventing it from overshooting the limit set)?
In that quote above I was describing how a clinician or user might calculate a Ti value to program into the machine. See my comment above about the auto backup algorithm relying on recent-averages of spontaneous breaths to derive backup rate and Ti value.4betterO2 wrote: 3- to complete a better understanding of #1 process above, adding the BPM factor
do you know how does it use the BPM in this calculation?-SWS wrote: A Ti limit is typically calculated using spontaneous BPM and I:E ratio.
Re: ASV users: the everything ASV thread.
Right, PaceWave Technology.-SWS wrote:I see Resmed recently added a separate obstruction-addressing treatment arm to their ASV:
http://www.resmed.com/us/products/s9_vp ... cliniciansResmed Marketing wrote: ...auto-adjusting EPAP in ASVAuto mode or fixed EPAP in ASV mode.
In their new CS-2, they said that they would address flow limitation and snores, but it appears the algorithm, like PR's, looks for failure to respond to PS and then simply raises EPAP. So again, when these flow-limited breaths should be enhanced by IPAP, they are crudely attacking any obstruction with EPAP.
Re: ASV users: the everything ASV thread.
That's my observation with PaceWave as well. Also, PaceWave's obstructive-addressing treatment arm does not seem as static-pressure aggressive as that of OSA-targeted AutoSet. It's much more gradual with static pressure variations. And while that approach might not be best-suited for UARS patients, it makes good sense for CompSAS patients who are generally sensitive to the aggressive static-pressure changes administered by ordinary OSA-targeted APAP algorithms.mollete wrote: ...it appears the algorithm, like PR's, looks for failure to respond to PS and then simply raises EPAP. So again, when these flow-limited breaths should be enhanced by IPAP, they are crudely attacking any obstruction with EPAP.
But I don't believe UARS/FL patients are going to find FL-suitable treatment in PaceWave's gradual static-pressure part of the algorithm---nor in Resmed's 90% targeting of MV. Both of those automated treatment arms will likely fall short of RERA avoidance. If perfect sinusoids via PS are the titration goal for UARS patients (e.g. Krakow's experimental UARS protocol), then high PS min values are still going to be necessary. At that point, the only value I can see in using ASV vs BiLevel for UARS patients is the ability for ASV to correct some of the iatrogenic central dysregulation those high PS min values will cause in some of the UARS patients.
Re: ASV users: the everything ASV thread.
When the BPM is set to manual:
is it something like
60s/(Tix2) =< BPM
(I guess the 'Tix2' would rather use a # larger than 2, since the expiration is supposed to be longer than the inspiration)
or rather, if you know how to calculate this, please tell me what is the max Ti that one could set for a BPM of 10 (probably between 2.0 and 3.0)?
By " backed or machine-cycled breaths", do you mean those breaths which are not patient-triggered? (and, what is the difference/significance between backed and machine-cycled?)
The fact that Ti will not come into play at all during spontaneous breaths, is that true also if BPM is set to auto?
2- if BPM is set to auto
If when the BPM is set to auto as well, the Ti does not come into play during patient-triggered beaths, which are the most prevalent ones, what causes short inspiration breaths most of the time, if it is not leaks? Could it be that the machine is not working properly, i.e. not sensing properly when the patient begins exhalation? Do the DME's have the tools to check the machine in such detail?
Mnay thanks for your experience, research, and answers...
I've often felt that an ST machine would be better for me, by giving me set cycle-times and pressures I could count on, but my Dr. said it is reserved for COPD patients. I guess it may have undesired consequences for someone who does not need it that much. Possibly, receiving machine-triggered breaths on onging basis could render the CNS dependent and thus aggravate any CNS problem... in the meantime, I really wish the ASV had a fullproof mode to prevent short inspirations times if you want that, it's hard to imagine why would anyone who does not absoluely need short inspirations, would want to have any of those, as they really limit how much oxygen you get...
Please give me the actual arithmetic equation for this:-SWS wrote: As an example, if a clinician entered a Ti value of 3.0, and then entered BPM of 15, then the machine would correct the programming error. The machine would automatically change Ti to 2.0s.
is it something like
60s/(Tix2) =< BPM
(I guess the 'Tix2' would rather use a # larger than 2, since the expiration is supposed to be longer than the inspiration)
or rather, if you know how to calculate this, please tell me what is the max Ti that one could set for a BPM of 10 (probably between 2.0 and 3.0)?
-SWS wrote:At that point IPAP is delivered for Ti seconds throughout each machine-delivered breath.
It looks as if Ti will not come into play at all during spontaneous breaths----and that Ti will be delivered as a fixed value (rather than upper limit) during all backed or machine-cycled breaths.
By " backed or machine-cycled breaths", do you mean those breaths which are not patient-triggered? (and, what is the difference/significance between backed and machine-cycled?)
The fact that Ti will not come into play at all during spontaneous breaths, is that true also if BPM is set to auto?
2- if BPM is set to auto
If when the BPM is set to auto as well, the Ti does not come into play during patient-triggered beaths, which are the most prevalent ones, what causes short inspiration breaths most of the time, if it is not leaks? Could it be that the machine is not working properly, i.e. not sensing properly when the patient begins exhalation? Do the DME's have the tools to check the machine in such detail?
Mnay thanks for your experience, research, and answers...
I've often felt that an ST machine would be better for me, by giving me set cycle-times and pressures I could count on, but my Dr. said it is reserved for COPD patients. I guess it may have undesired consequences for someone who does not need it that much. Possibly, receiving machine-triggered breaths on onging basis could render the CNS dependent and thus aggravate any CNS problem... in the meantime, I really wish the ASV had a fullproof mode to prevent short inspirations times if you want that, it's hard to imagine why would anyone who does not absoluely need short inspirations, would want to have any of those, as they really limit how much oxygen you get...
_________________
| Mask: Wisp Nasal CPAP Mask with Headgear - Fit Pack |
| Humidifier: DreamStation Heated Humidifier |
PR Dreamstation BiPap ASV, WISP nasal mask with magnets
Re: ASV users: the everything ASV thread.
seems to me the ASV algorithm does enhance IPAP as well, since it increases IPAP automatically by adding at least the min PS to the increased EPAP. Moreover, it also increases the IPAP further by increasing the PS part of th equation as needed even over increased EPAP, it does not necessarily keep using the minimum PS value when raising EPAP.mollete wrote: it appears the algorithm, like PR's, looks for failure to respond to PS and then simply raises EPAP. So again, when these flow-limited breaths should be enhanced by IPAP, they are crudely attacking any obstruction with EPAP.
Do you mean that flow-limited breaths are not included, in the way the machine attacks obstruction?
_________________
| Mask: Wisp Nasal CPAP Mask with Headgear - Fit Pack |
| Humidifier: DreamStation Heated Humidifier |
PR Dreamstation BiPap ASV, WISP nasal mask with magnets
Re: ASV users: the everything ASV thread.
If you want to calculate the largest Ti allowed by your ASV machine, then you can use Ti =< (30/BPM). Recall that Respironics does not allow Ti to be set greater than 3.0s under ANY circumstances. So that equation works for BPM values at 10 and greater. If you programmed BPM at less than 10, then the largest Ti allowed would still be 3.0s. But if you programmed BPM at 10 or any value greater, then Ti=<(30/BPM) would work.4betterO2 wrote:When the BPM is set to manual:
Please give me the actual arithmetic equation for this:-SWS wrote: As an example, if a clinician entered a Ti value of 3.0, and then entered BPM of 15, then the machine would correct the programming error. The machine would automatically change Ti to 2.0s.
is it something like
60s/(Tix2) =< BPM
(I guess the 'Tix2' would rather use a # larger than 2, since the expiration is supposed to be longer than the inspiration)
or rather, if you know how to calculate this, please tell me what is the max Ti that one could set for a BPM of 10 (probably between 2.0 and 3.0)?
Yes. A backed breath is not patient triggered. So a backed breath entails the machine "triggering" the EPAP-to-IPAP transition as well as "cycling" the IPAP-to-EPAP transition. Thus the machine will "trigger" IPAP---and deliver IPAP for the duration of Ti. The machine will also "cycle" EPAP---and deliver the EPAP pressure for the duration of total T minus Ti. In other words, total EPAP time allotted would be [(60/BPM) - Ti)].4betterO2 wrote: By " backed or machine-cycled breaths", do you mean those breaths which are not patient-triggered? (and, what is the difference/significance between backed and machine-cycled?)
I think so, but I'm not absolutely certain.4betterO2 wrote: The fact that Ti will not come into play at all during spontaneous breaths, is that true also if BPM is set to auto?
I think it's going to boil down to one of these three possibilities: 1) leaks that skew accurate detection of spontaneous I and E transitions, 2) erratic patient breathing the algorithm finds difficult to frequency-count & average, or 3) machine malfunction as you pointed out.4betterO2 wrote: 2- if BPM is set to auto
If when the BPM is set to auto as well, the Ti does not come into play during patient-triggered beaths, which are the most prevalent ones, what causes short inspiration breaths most of the time, if it is not leaks? Could it be that the machine is not working properly, i.e. not sensing properly when the patient begins exhalation? Do the DME's have the tools to check the machine in such detail?
BiLevel S/T, BiPAP S/T, or VPAP S/T in general are well-suited for non-COPD patients with central issues. Perhaps your doctor was thinking of a different treatment platform such as AVAPS. Good luck!4betterO2 wrote: Mnay thanks for your experience, research, and answers...
I've often felt that an ST machine would be better for me, by giving me set cycle-times and pressures I could count on, but my Dr. said it is reserved for COPD patients. I guess it may have undesired consequences for someone who does not need it that much. Possibly, receiving machine-triggered breaths on onging basis could render the CNS dependent and thus aggravate any CNS problem... in the meantime, I really wish the ASV had a fullproof mode to prevent short inspirations times if you want that, it's hard to imagine why would anyone who does not absoluely need short inspirations, would want to have any of those, as they really limit how much oxygen you get...
Re: ASV users: the everything ASV thread.
Thanks for all the details on Ti.-SWS wrote: BiLevel S/T, BiPAP S/T, or VPAP S/T in general are well-suited for non-COPD patients with central issues.
Perhaps your doctor was thinking of a different treatment platform such as AVAPS. Good luck!
what is the difference between these machines? Are these all from PR? are they successive/improved models, if so wich is the best one, or do they function differently for other reasons than improvement?
_________________
| Mask: Wisp Nasal CPAP Mask with Headgear - Fit Pack |
| Humidifier: DreamStation Heated Humidifier |
PR Dreamstation BiPap ASV, WISP nasal mask with magnets
Re: ASV users: the everything ASV thread.
You're very welcome. They are all BiLevel S/T machines. BiPAP is Respironics' trademark for BiLevel, while VPAP is Resmed's trademark for BiLevel. The Resmed VPAP S/T machines offer Ti min and Ti max controls, which is what I think you are hoping might work better than Respironics' single Ti parameter. Bear in mind that Resmed's ASV does not offer Ti min and Ti max clinician settings.4betterO2 wrote: Thanks for all the details on Ti.
what is the difference between these machines? Are these all from PR? are they successive/improved models, if so wich is the best one, or do they function differently for other reasons than improvement?
Re: ASV users: the everything ASV thread.
Can DME's usually do a hardware/firmware technical diagnosis procedure to check that the machine is working OK?-SWS wrote: I think it's going to boil down to one of these three possibilities: 1) leaks that skew accurate detection of spontaneous I and E transitions, 2) erratic patient breathing the algorithm finds difficult to frequency-count & average, or 3) machine malfunction as you pointed out.
Or do they usually just send off the machine to a repair center for evaluation?
_________________
| Mask: Wisp Nasal CPAP Mask with Headgear - Fit Pack |
| Humidifier: DreamStation Heated Humidifier |
PR Dreamstation BiPap ASV, WISP nasal mask with magnets
Re: ASV users: the everything ASV thread.
But the Resmed VPAP S/T machine does not deliver machine-triggered breaths, correct?-SWS wrote: The Resmed VPAP S/T machines offer Ti min and Ti max controls, which is what I think you are hoping might work better than Respironics' single Ti parameter. Bear in mind that Resmed's ASV does not offer Ti min and Ti max clinician settings.
how does it manage the cycling from IPAP to EPAP? Does it sense, or estimates, when inhaling has ended?-SWS wrote: Bear in mind that Resmed's ASV does not offer Ti min and Ti max clinician settings.
Is its cycling better managed because of its ASV algorithm, i.e. by volume control?
Does it determine better than the PR machine, when inhaling has ended?
_________________
| Mask: Wisp Nasal CPAP Mask with Headgear - Fit Pack |
| Humidifier: DreamStation Heated Humidifier |
PR Dreamstation BiPap ASV, WISP nasal mask with magnets
Re: ASV users: the everything ASV thread.
4better02, maybe if you can explain the problem that you're having a little more clearly we can try to help.
Is it that you're finding the transition between IPAP and EPAP as a problem at the top of the breath, or is it that you're finding that the ASV is forcing you to breathe more rapidly than you'd like?
Is it that you're finding the transition between IPAP and EPAP as a problem at the top of the breath, or is it that you're finding that the ASV is forcing you to breathe more rapidly than you'd like?
Re: ASV users: the everything ASV thread.
Indeed I'm interested in general in finding out the best machine across brands, for later.
Unfortunately this year I'm limited by my DME to Respironics, it's all they carry.
I haven't explored yet all the intricacies of changing DME, as I do not know if, or to what extent, my Dr. and DME are connected.
So I'm still trying my best with PR equipment as yet.
So to sum up my problem currently:
What is the best PR machine to treat someone with CSA, and needing to be protected from short inspiration times?
And, how should it be setup, to achieve these goals?
A while back soemone had given me a phone# for the Respironics tech support, you had to give an account#, then you could talk to someone, but I lost that #. Does anyone know it?
Unfortunately this year I'm limited by my DME to Respironics, it's all they carry.
I haven't explored yet all the intricacies of changing DME, as I do not know if, or to what extent, my Dr. and DME are connected.
So I'm still trying my best with PR equipment as yet.
So to sum up my problem currently:
What is the best PR machine to treat someone with CSA, and needing to be protected from short inspiration times?
And, how should it be setup, to achieve these goals?
A while back soemone had given me a phone# for the Respironics tech support, you had to give an account#, then you could talk to someone, but I lost that #. Does anyone know it?
_________________
| Mask: Wisp Nasal CPAP Mask with Headgear - Fit Pack |
| Humidifier: DreamStation Heated Humidifier |
PR Dreamstation BiPap ASV, WISP nasal mask with magnets
Re: ASV users: the everything ASV thread.
I've written about this with more detail before, but my problem is, quite often the machine cycles from IPAP to EPAP before I have finished inhaling; the drop of pressure forces me to exhale prematurely, it's as if I hit an wall of void air. -SWS has helped me a lot to explore Ti settings issues, they are tricky! if more people pitch in, it would help me to see if others are having that problem, and I might be able to either find a solution, or, determine if my own machine is defective...old64mb wrote:4better02, maybe if you can explain the problem that you're having a little more clearly we can try to help.
Other than the Ti issue, my ASV machine has been much more effective than my previous BiPAP one for treating OSA, and it has practically completely treated periodic breathing. But the Ti probem is important, very uncomfortable, and worrysome as I do not have O2 data as yet, and I'm worried that I may not get enough O2 during those shortened inspirations, they are about 0.5s!
_________________
| Mask: Wisp Nasal CPAP Mask with Headgear - Fit Pack |
| Humidifier: DreamStation Heated Humidifier |
Last edited by 4betterO2 on Wed Jan 23, 2013 6:38 pm, edited 1 time in total.
PR Dreamstation BiPap ASV, WISP nasal mask with magnets