Thanks for weighing in, Jay. I definitely appreciate the suggestions. To hit most of your points, although not in order:
* My doc right now has his specialty in pulmonary, and I'm scheduled for a follow-up with him mid-month. Your suggestion that someone with a neurology background seems spot-on and is what I've been thinking as well. I'm planning to see another local sleep doc who has an excellent reputation and a neurology background. I figure more input is a good thing, and since I'll just be out my copay, the price is right. If there really is more than one problem going on, that's the best way to figure it out.
* Changing settings: I have been trying to keep things constant for several days at a time. Unfortunately, so far, I've yet to find anything that consistently yields both a quantitative and qualitative improvement. I took a nap two days ago without the ventilator, and while I wore it that night, when I woke up the following morning I went back to sleep without it. I felt so much more rested and wonderful
not using it. I know the common advice is to encourage patience, but in my case, I've been on one ventilator or another for the better part of a year now. I don't feel like this is an issue of me getting "used to it."
* Meds: I've set aside the clonazepam almost completely, although my understanding is that it can actually help with central apneas and PLMD. Nevertheless, that's not really the med I want to get dependent on to deal with those problems. As far as the Ambien goes, I had initially started with 5 mg a couple years ago but had to bump it up to 10 mg about a year ago. My body seems to build up a tolerance to it, which is why I switch back and forth between it and Lunesta (to which I build a quicker tolerance). I wish I didn't have to take
any of these things, but my insomnia is just bad enough to make sleep nearly impossible while on the ventilator without them. Anyway, I kind of like your idea about splitting the tablet and taking a little more when I wake up -- I'll give that a shot tonight.
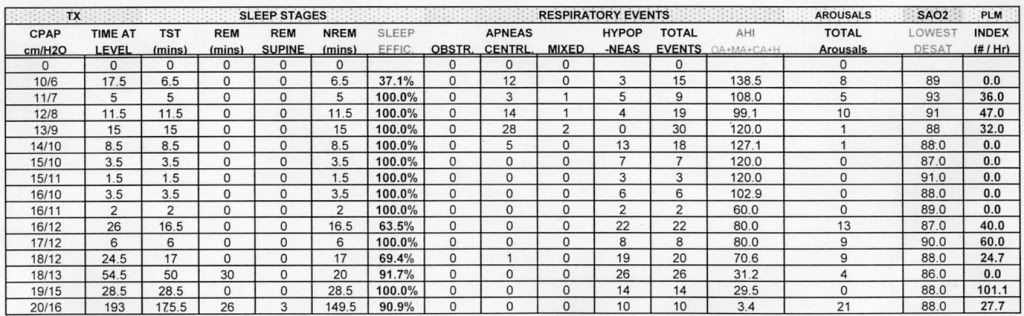
An addendum I've been meaning to add to this thread has to do with my "old" titration results. A lot of the thinking is that giving the ASV free reign has me starting at a pressure that's simply too low. I should have done it earlier, but this is the table from my BiPAP titration:
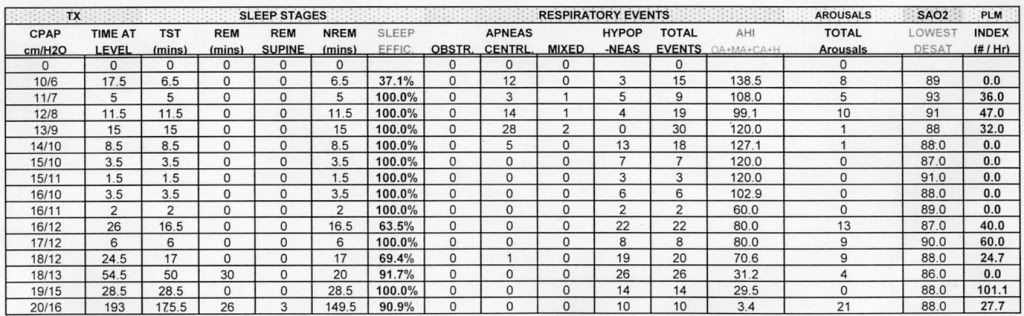
What's most interesting and perplexing to me is that the pressure increases by the technologist were not done to treat obstructive apneas; they were to treat centrals predominantly, and then hypopneas. As -SWS had explained to me in my BiPAP thread a while back, we can't be sure whether hypopneas are obstructive or central in nature, but here I actually don't think that matters since the ratio of centrals to hypopneas is high for the first four pressure settings they tried, ranging from 10/6 to 13/9. Throughout the entire night, I didn't have a single obstructive apnea at
any pressure setting. Granted, the brief duration at each setting means that there is no guarantee that an obstructive event
wouldn't have occurred at that setting given enough time, but still...
What does this mean practically for me? I don't know. Maybe some of you folks do. But at least in the BiPAP titration, the pressure increases weren't to address obstructive apneas. I have a call into my nurse to get my full PSG results from all four of my studies, as I'm eager to see what the table in my initial CPAP titration looked like too.