Why is this?
First, the patient in the sleep lab is sleeping in a strange environment, with many devices connected to him, and with people observing him through cameras and listening to him through microphones. The patient often arrives with considerable anxiety and this may continue throughout the night. The room, the bed, the pillows, the bed covers, and the room temperature and relative humidity are often very different to what he is accustomed to at home. Also, the patient is likely using CPAP for the first time and is experiencing some discomfort because he has not adjusted to the mask or the pressure. This means more anxiety.
Second, with all these problems the sleep lab only has one night to get the settings right. And these are settings the patient is going to use for many, many nights.
The bottom line is the patient is unlikely to sleep in the lab as he does at home and the pressure settings determined during the lab titration may not produce an optimal therapy at home. With improper settings the patient is setup to be a failure, to struggle with CPAP, and in many cases to abandon CPAP altogether.
What is the solution to this problem?
For many people the solution has been to obtain a “fully data-capable” machine with software to monitor their breathing while sleeping at home. The software will produce a daily report giving breathing details throughout the night on a time line graph. These patients can see data on apneas, hypopneas, snores, mask leak, pressure, etc. throughout the night.
By observing this data over days, weeks, and even months the patient can make sure his therapy is working well. With a little self-education and some support from experienced CPAPers, the patient can make adjustments to his mask, his sleeping position, and his CPAP settings to achieve a healthy CPAP therapy.
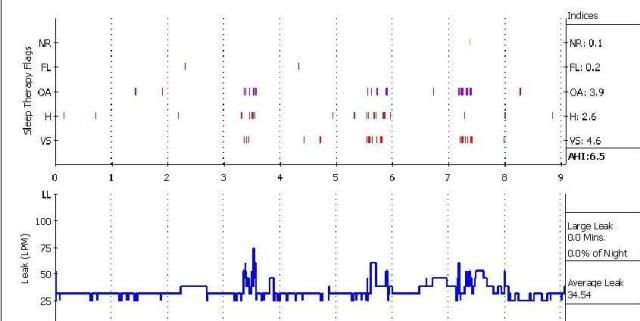
Below is an extract of a report from one patient’s data. This patient is using the CPAP settings prescribed by his sleep lab. Note that the patient had an AI (Apnea Index or OA) of 3.9 over 9 hours. This is 35 apneas for the night and it means the patient stopped breathing 35 times and was awakened 35 times to restart breathing. How do you like being awakened in the middle of the night by a wrong phone number? What if it happened 35 times in a night?
Note also that the patient had a significant amount of hypopneas (H) and snores (VS).
Now below is an extract of the same patient’s data a few weeks later. In the interim the patient has gradually adjusted his CPAP settings and made some other changes. Each time an adjustment was made the data was reviewed the next morning to observe the effect of the adjustment. Making small adjustments over several nights, the patient eventually achieved an optimal therapy. Note that for this night his AI (OA) was 0.4 or only 3 apneas for the night compared to 35 apneas using the lab-prescribed settings. The patient had a minimal number of hypopneas and flow limitations (FL) and no snores.
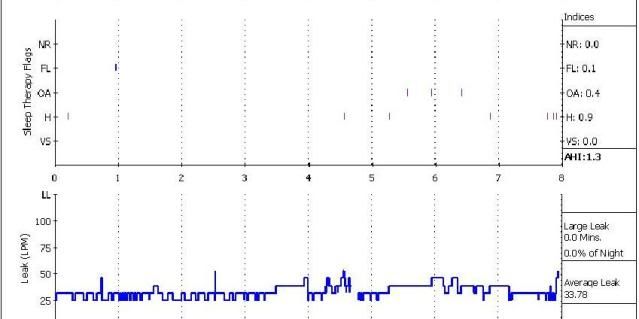
The patient reports a much improved level of energy, no sleepiness during the day, and less irritability. This patient was able to lose weight, bring his blood-sugar levels into the normal range down from prediabetic range, and increase his level of exercise from moderate to strenuous.
So what about you? Do you want to manage your therapy with or without the software?












