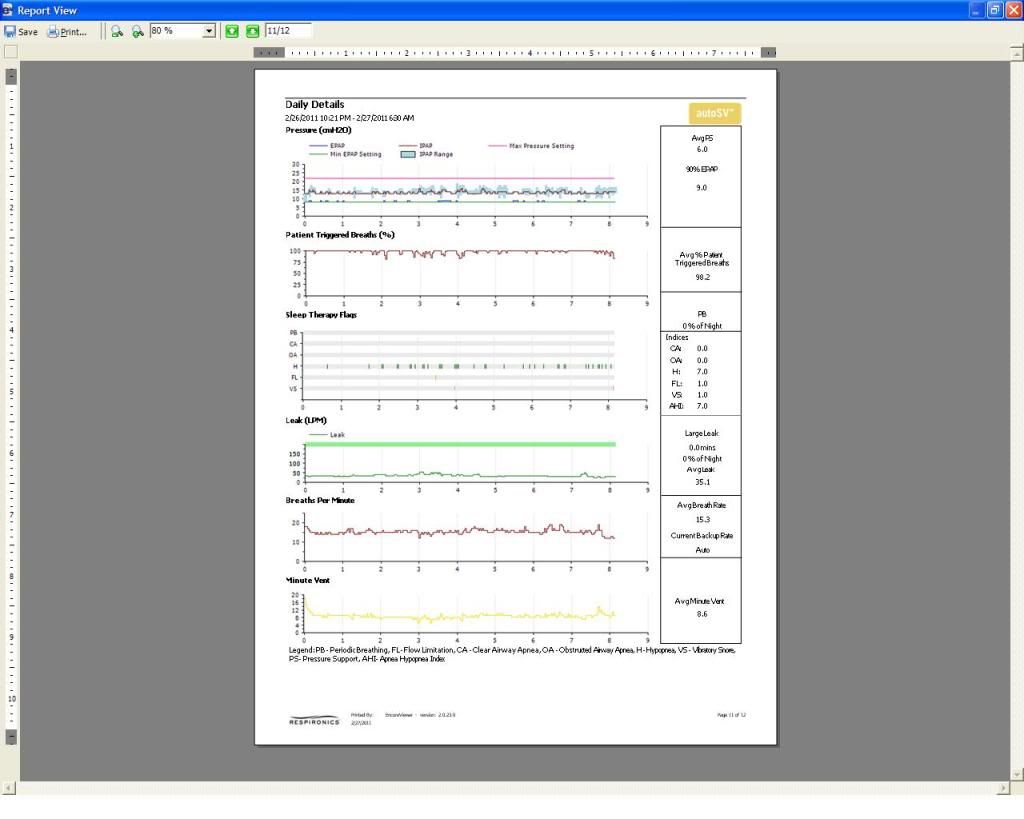
JIMCHI wrote:I have had poor results when I have lowered the EPAP Min. I did that just the other day at someone's suggestion (set min at 6 and max at 12) and had an AHI of 18, one of my highest and also felt tired. I also tried an EPAP min of 6 a few weeks ago and felt terrible the next day. So, eliminating that, my next best adjustment would be to increase the PS Min to 6 and that's all ? Or would it be better just to leave everything the way it was last night and let's see if I can get two consistent results, without the AHI going to some large number tonight? The big problem has been the variances. So the fact that I had an AHI of 7 last night could well mean nothing and I could have 17 tonight, all things remaining the same.
Leaving the settings the way they are sounds smart to me, JIMCHI. That way you can tell your doctor tomorrow exactly what your are up to... You can also test these settings another night toward discerning either consistent or variable results as you mentioned.
After that, setting PS min@ 6 would probably be my next experiment if it were me----pending doctor approval, of course. However, I wouldn't rule out eventually experimenting by also lower EPAP min----for comparison---after you find your best PS min. It's entirely possible that you have experienced some mix of both "primary" residual hypopneas and machine-induced or "iatrogenic" central hypopneas. That, in turn, implies that there may be an optimal trade-off/combination of EPAP min and PS min to thoroughly explore. So once you have PS behaving optimally, EPAP min MIGHT turn out to sit at some new optimal value that is lower. IMHO combinatorial experimentation with those two parameters beats basic deductive reasoning.
So in summary, I think PS adjustments are probably your key to treating those excessive residual hyponeas; but optimal EPAP min MIGHT change along the way as a matter of combinatorial effect on respiratory-drive.
Banned wrote:I thought the general consensus of the sleep medicine community is that the optimal spread from EPAP to IPAP is 4cmH20 and above?
Yes. Consensus suggests that standard BiLevel titrations
manually fix PS somewhere between 4cm and 10cm:
http://www.aasmnet.org/Resources/Clinic ... 040210.pdf
But bear in mind we're not manually setting a constant PS here. And what AASM recommends for a standard BiLevel machine is actually different than what Respironics suggests PS min toward setting base modality on BiPAP autoSV. Respironics recommends PS min initially set at at 0 (CPAP modality)---with BiLevel kicking in on an as-needed basis. Throughout the night, that recommended autoSV setting alternates between delivering CPAP, then BiLevel, then CPAP, and so forth. Anyway, some CompSAS patients probably fare better with CPAP as ASV's base modality (setting PS min =0) and others probably fare better with BiLevel as ASV's base modality (setting PS min > 0).
JIMCHI, so far you have tried the first three of these four treatment modalities: 1) CPAP, 2) BiLevel, 3) ASV w/ BiLevel as base modality, and 4) ASV w/ CPAP as base modality. I would encourage you to consider eventually comparing those last two modalities----rather than assuming past trials with modalities one and two (CPAP and BiLevel respectively) can yield definitive conclusions about WHICH of those last two ASV modalities is your best bet. As it stands I'd bet modality three is your best choice. But if it were me, I'd eventually get around to running at least a one-night trial of modality four---ASV w/ CPAP as base---for the sake of comparison. There's a reason Respironics defaults that as their first choice during titration for either generation of their BiPAP autoSV machines. My understanding is that CPAP as ASV's base modality is inherently less destabilizing for some CompSAS patients---otherwise it wouldn't be Respironics' first-choice during their ASV model-specific titrations.
(note: in reality the EPAP-min through EPAP-max range on the Advanced model implies APAP as base modality; setting EPAP-min to equal EPAP-max gets the Advanced model back down to true CPAP as base modality)
Above all else, I'd be sure to get my medical team in the loop and listen very carefully to what they suggest. Again, good luck.