I have uploaded a winRAR file (had to do it in three parts) to a file sharing site. Could you please email me a contact address so I can send you the links? It doesn't look like you allow PMs.NotMuffy wrote:Sure.split_city wrote:Windaq files are 200-300MB. Are you ok with this?
I'm a lot stronger than I look.
Squishing the belly increases AHI
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Squishing the belly increases AHI
Re: Squishing the belly increases AHI
It looks like there will not only be a battle of Real (American) Football vs. Running Into A Wall Without A Helmet (or Australian whatever the heck you'd call it) but Chicago vs AASM 2008, sleep vs sleep disruption, Good vs Evil (NotMuffy = good, of course) as well as a host of other topics!
But I guess since this topic:
viewtopic/t56120/Sex-Life-and-Apnea-Im-embarrassed.html
puts up double the views in half the time, TechnoFlash and the War of the Continents isn't quite as exciting as I thought and will go underground.
See ya!
But I guess since this topic:
viewtopic/t56120/Sex-Life-and-Apnea-Im-embarrassed.html
puts up double the views in half the time, TechnoFlash and the War of the Continents isn't quite as exciting as I thought and will go underground.
See ya!
"Don't Blame Me...You Took the Red Pill..."
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Squishing the belly increases AHI
Maybe best to continue discussion in here now.
Calculated AHI under each cuff condition (stage 2 ONLY):
Deflated: 17
Mid: 27
Max: 61
Total time spent under each cuff condition (mins):
Deflated: 121.5
Mid: 111
Max: 121.5
Time spent under each cuff condition - separated by sleep stage (minutes / % of total time under cuff condition)
Deflated
Wake: 32 / 26.3
Stage 1: 15.5 / 12.8
Stage 2: 74 / 60.9
Stage 3: 0 / 0
Stage 4: 0 / 0
REM: 0 / 0
Mid
Wake: 56.5 / 50.9
Stage 1: 16.5 / 14.9
Stage 2: 38 / 34.2
Stage 3: 0 / 0
Stage 4: 0 / 0
REM: 0 / 0
Max
Wake: 58.5 / 48.1
Stage 1: 18 / 14.8
Stage 2: 44.5 / 36.6
Stage 3: 0.5 / 0.4
Stage 4: 0 / 0
REM: 0 / 0
I guess the million $ question from this study is...what caused the increase in AHI with abdominal compression? Is it simply due to an increase in upper airway collapsibility as shown by my previous abdominal compression study? Maybe, but we didn't directly measure airway collapsibility in this study. I think a vital point raised by you is the effect of arousals. A problem with this study is that abdominal compression perhaps led to increased arousals and that the rise in AHI may simply reflect the increased occurrence of post-arousal central hypopneas. Several groups have shown that arousals result in a period of hyperventilation, followed by a period of hypoventilation (Jordan et al 2003, 2004). Badr also supports this finding, by showing that mild hypocapnia, induced by mechanical ventilation, resulted in hypopnea (central flavor) once the ventilator was switched off. Nevertheless, while abdominal compression may directly alter upper airway function via tracheal traction effects, it may also influence respiratory control. For example, abdominal compression leads to a reduction in lung volume (data still to be analyzed). The subsequent reduction in lung volume is less effective in damping out fluctuations in alveolar gas tensions, potentially leading to unstable breathing.
Just some food-for-thought...not saying any of this is right, but good for discussion.
So what are your throughts about the results from the Heinzer et al 2006 study?
A few things to add about this patient:NotMuffy wrote: In a guy like this tho I would argue that he never gets to a steady state. If we agree that sleep instability unto itself generates respiratory instabilty, that this guy is a train wreck adds far too many variables to say +abdominal compression > +AHI. In re: poor sleep architecture, I would look at stage changes (total and to stage 1) to get a feel for poor architecture (sleep efficiency is good to know, but obviously since wake doesn't figure in to calculations who cares).
Calculated AHI under each cuff condition (stage 2 ONLY):
Deflated: 17
Mid: 27
Max: 61
Total time spent under each cuff condition (mins):
Deflated: 121.5
Mid: 111
Max: 121.5
Time spent under each cuff condition - separated by sleep stage (minutes / % of total time under cuff condition)
Deflated
Wake: 32 / 26.3
Stage 1: 15.5 / 12.8
Stage 2: 74 / 60.9
Stage 3: 0 / 0
Stage 4: 0 / 0
REM: 0 / 0
Mid
Wake: 56.5 / 50.9
Stage 1: 16.5 / 14.9
Stage 2: 38 / 34.2
Stage 3: 0 / 0
Stage 4: 0 / 0
REM: 0 / 0
Max
Wake: 58.5 / 48.1
Stage 1: 18 / 14.8
Stage 2: 44.5 / 36.6
Stage 3: 0.5 / 0.4
Stage 4: 0 / 0
REM: 0 / 0
Unfortunately no. Probably something we should have included.NotMuffy wrote:Was there a snoring channel? I don't see it in my EDF Reader. I think it might help a little in giving support to central hypopnea identification.
We didn't specifically have any rule for these. As shown by the report, 6.5 arousals per hour were attributed to by leg movements. Therefore, PLMS perhaps an issue.NotMuffy wrote:What rule did she use when PLMs appeared with respiratory events? I think this guy does have PLMs:
All very interesting. I haven't yet analysed the arousal index within each cuff condition. But based on the data I presented, there would likely be more arousals with cuff up, at least in this patient.NotMuffy wrote:
so I would submit in this area the respiratory stuff is all post-arousal central hypopnea.
I guess the million $ question from this study is...what caused the increase in AHI with abdominal compression? Is it simply due to an increase in upper airway collapsibility as shown by my previous abdominal compression study? Maybe, but we didn't directly measure airway collapsibility in this study. I think a vital point raised by you is the effect of arousals. A problem with this study is that abdominal compression perhaps led to increased arousals and that the rise in AHI may simply reflect the increased occurrence of post-arousal central hypopneas. Several groups have shown that arousals result in a period of hyperventilation, followed by a period of hypoventilation (Jordan et al 2003, 2004). Badr also supports this finding, by showing that mild hypocapnia, induced by mechanical ventilation, resulted in hypopnea (central flavor) once the ventilator was switched off. Nevertheless, while abdominal compression may directly alter upper airway function via tracheal traction effects, it may also influence respiratory control. For example, abdominal compression leads to a reduction in lung volume (data still to be analyzed). The subsequent reduction in lung volume is less effective in damping out fluctuations in alveolar gas tensions, potentially leading to unstable breathing.
Just some food-for-thought...not saying any of this is right, but good for discussion.
So what are your throughts about the results from the Heinzer et al 2006 study?
Thorax. 2006 May;61(5):435-9. Epub 2006 Feb 20.
Effect of increased lung volume on sleep disordered breathing in patients with sleep apnoea.
Heinzer RC, Stanchina ML, Malhotra A, Jordan AS, Patel SR, Lo YL, Wellman A, Schory K, Dover L, White DP.
Sleep Medicine Division, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. rheinzer@post.harvard.edu
Abstract
BACKGROUND: Previous studies have shown that changes in lung volume influence upper airway size and resistance, particularly in patients with obstructive sleep apnoea (OSA), and that continuous positive airway pressure (CPAP) requirements decrease when the lung volume is increased. We sought to determine the effect of a constant lung volume increase on sleep disordered breathing during non-REM sleep.
METHODS: Twelve subjects with OSA were studied during non-REM sleep in a rigid head-out shell equipped with a positive/negative pressure attachment for manipulation of extrathoracic pressure. The increase in lung volume due to CPAP (at a therapeutic level) was determined with four magnetometer coils placed on the chest wall and abdomen. CPAP was then stopped and the subjects were studied for 1 hour in three conditions (in random order): (1) no treatment (baseline); (2) at "CPAP lung volume", with the increased lung volume being reproduced by negative extrathoracic pressure alone (lung volume 1, LV1); and (3) 500 ml above the CPAP lung volume(lung volume 2, LV2).
RESULTS: The mean (SE) apnoea/hypopnoea index (AHI) for baseline, LV1, and LV2, respectively, was 62.3 (10.2), 37.2 (5.0), and 31.2 (6.7) events per hour (p = 0.009); the 3% oxygen desaturation index was 43.0 (10.1), 16.1 (5.4), and 12.3 (5.3) events per hour (p = 0.002); and the mean oxygen saturation was 95.4 (0.3)%, 96.0 (0.2)%, 96.3 (0.3)%, respectively (p = 0.001).
CONCLUSION: An increase in lung volume causes a substantial decrease in sleep disordered breathing in patients with OSA during non-REM sleep.
Re: Squishing the belly increases AHI
Right, we looked at that in the other thread, you can't go wrong with the Boston crowd.split_city wrote:So what are your throughts about the results from the Heinzer et al 2006 study?
Thorax. 2006 May;61(5):435-9. Epub 2006 Feb 20.
Effect of increased lung volume on sleep disordered breathing in patients with sleep apnoea.
Heinzer RC, Stanchina ML, Malhotra A, Jordan AS, Patel SR, Lo YL, Wellman A, Schory K, Dover L, White DP.
Sleep Medicine Division, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. rheinzer@post.harvard.edu
Abstract
BACKGROUND: Previous studies have shown that changes in lung volume influence upper airway size and resistance, particularly in patients with obstructive sleep apnoea (OSA), and that continuous positive airway pressure (CPAP) requirements decrease when the lung volume is increased. We sought to determine the effect of a constant lung volume increase on sleep disordered breathing during non-REM sleep.
METHODS: Twelve subjects with OSA were studied during non-REM sleep in a rigid head-out shell equipped with a positive/negative pressure attachment for manipulation of extrathoracic pressure. The increase in lung volume due to CPAP (at a therapeutic level) was determined with four magnetometer coils placed on the chest wall and abdomen. CPAP was then stopped and the subjects were studied for 1 hour in three conditions (in random order): (1) no treatment (baseline); (2) at "CPAP lung volume", with the increased lung volume being reproduced by negative extrathoracic pressure alone (lung volume 1, LV1); and (3) 500 ml above the CPAP lung volume(lung volume 2, LV2).
RESULTS: The mean (SE) apnoea/hypopnoea index (AHI) for baseline, LV1, and LV2, respectively, was 62.3 (10.2), 37.2 (5.0), and 31.2 (6.7) events per hour (p = 0.009); the 3% oxygen desaturation index was 43.0 (10.1), 16.1 (5.4), and 12.3 (5.3) events per hour (p = 0.002); and the mean oxygen saturation was 95.4 (0.3)%, 96.0 (0.2)%, 96.3 (0.3)%, respectively (p = 0.001).
CONCLUSION: An increase in lung volume causes a substantial decrease in sleep disordered breathing in patients with OSA during non-REM sleep.
As we look at this particular guy tho, he seems to have too many confounders to be your showcase guy.
In another interesting spot...
"Don't Blame Me...You Took the Red Pill..."
Re: Squishing the belly increases AHI
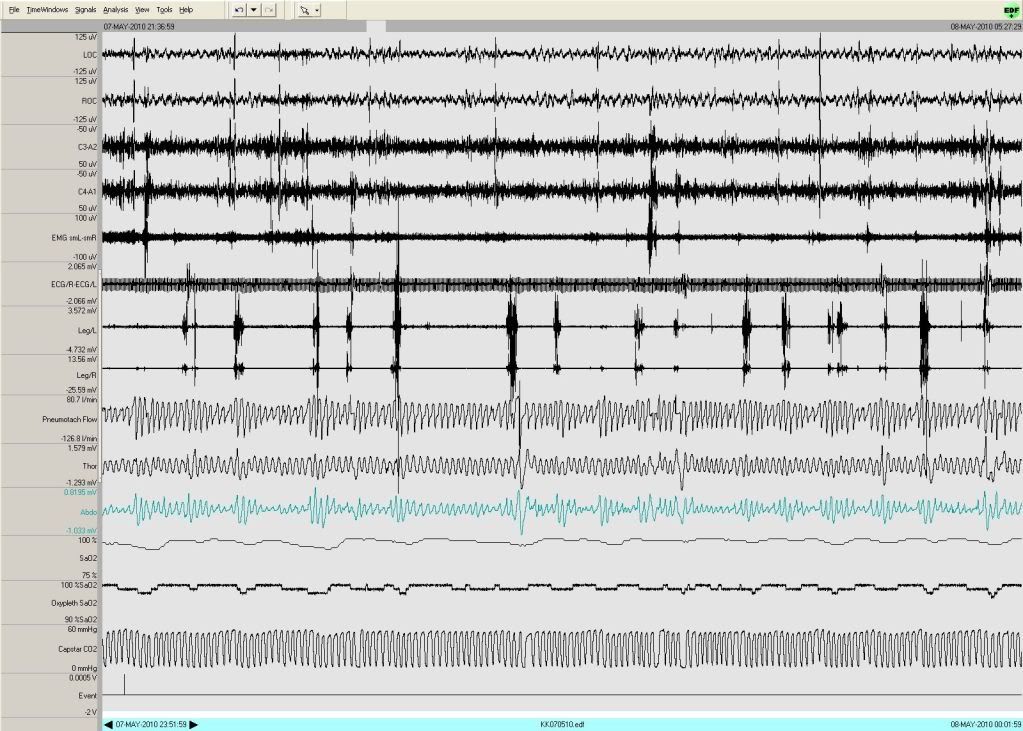
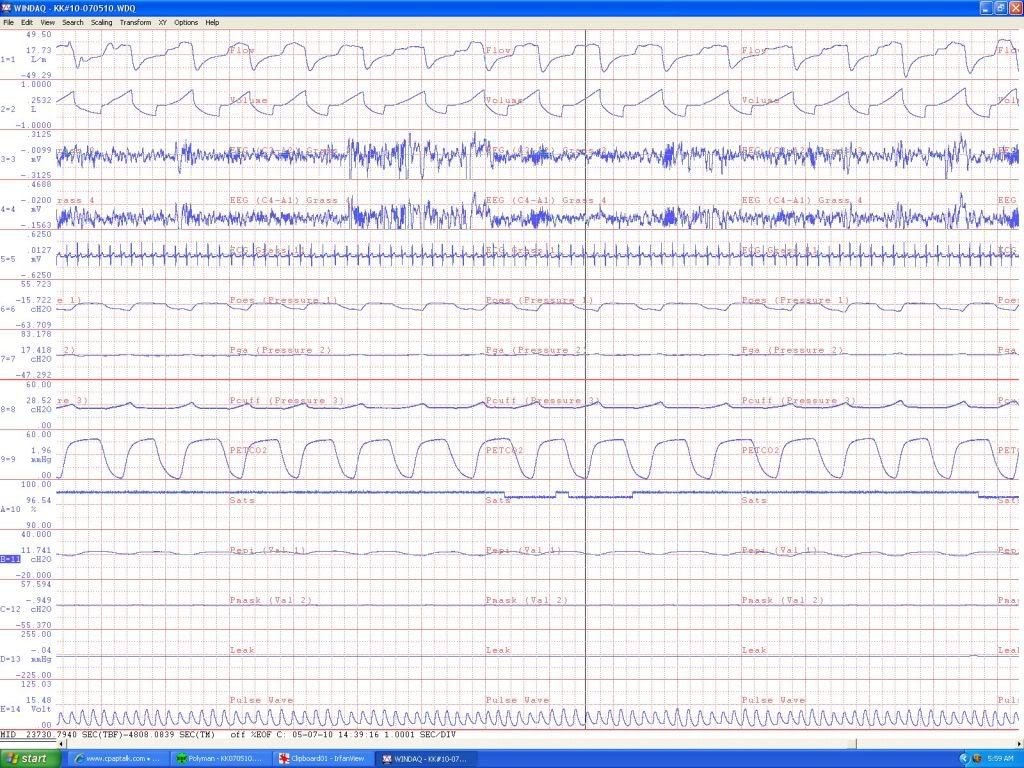
...looking at this area (using WinDAQ, for those who wonder why the grid is different):
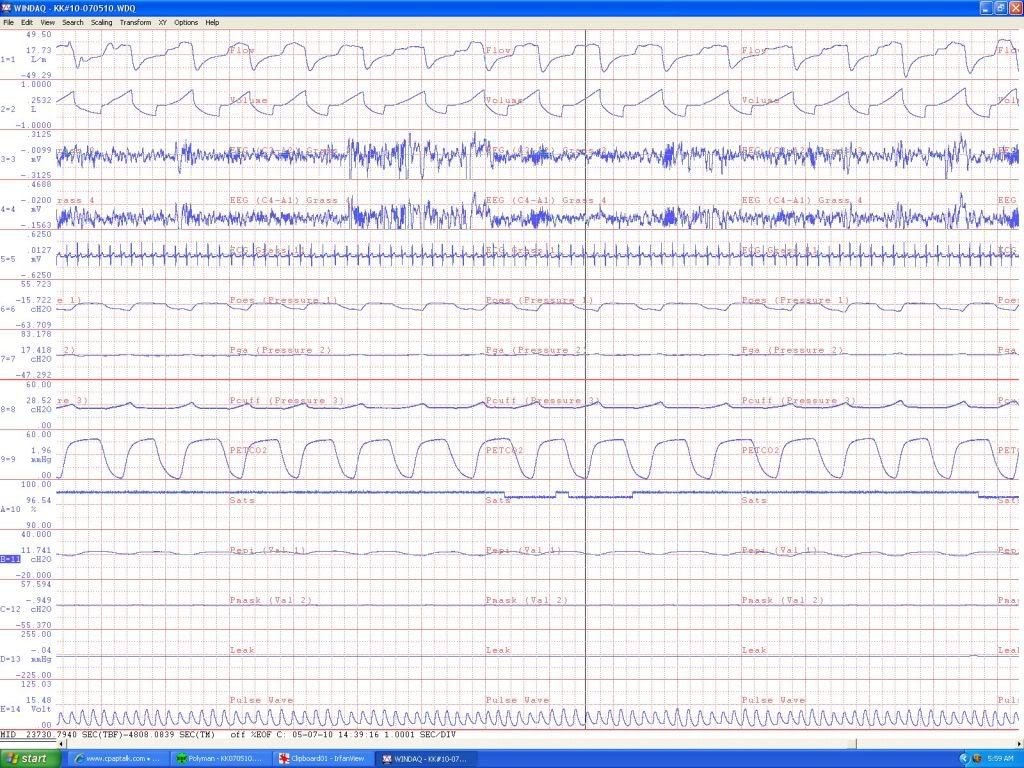
he does put up some stable Stage 2 (I think your scorer called a lot of this SWS, but other than that delta burst, all them spindles are saying this is Duece).
Was this guy on medications? Depression? He's also sans REM. This is a screwy case.
he does put up some stable Stage 2 (I think your scorer called a lot of this SWS, but other than that delta burst, all them spindles are saying this is Duece).
Was this guy on medications? Depression? He's also sans REM. This is a screwy case.
"Don't Blame Me...You Took the Red Pill..."
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Squishing the belly increases AHI
Hey? Nah, that part of the file was scored as stage 2.NotMuffy wrote:...looking at this area (using WinDAQ, for those who wonder why the grid is different):
he does put up some stable Stage 2 (I think your scorer called a lot of this SWS, but other than that delta burst, all them spindles are saying this is Duece.
Can't remember if this guy was ony meds. Don't recall him stating he had depression.NotMuffy wrote:Was this guy on medications? Depression? He's also sans REM. This is a screwy case.
Re: Squishing the belly increases AHI
OK, matching up the time stamp (about 1439), it looked like SWS on the histogram:split_city wrote:Hey? Nah, that part of the file was scored as stage 2.NotMuffy wrote:...looking at this area (using WinDAQ, for those who wonder why the grid is different):
he does put up some stable Stage 2 (I think your scorer called a lot of this SWS, but other than that delta burst, all them spindles are saying this is Duece.
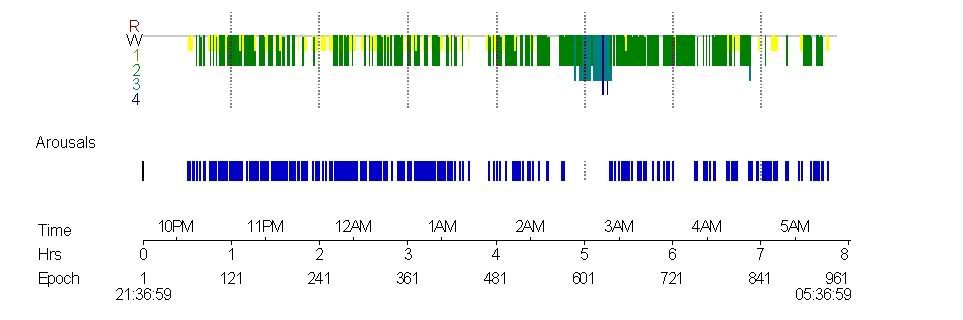
Note train-wreck architecture and absence of REM.
"Don't Blame Me...You Took the Red Pill..."
Re: Squishing the belly increases AHI
Well, this scientific thread has great esoteric appeal IMHO. I for one enjoy and appreciate the discussion. However, if you want to increase readership, the subject line needs to be reworked to something like: Subject: Did Occult/Repressed Sex Drive Confound Our Squished Belly AHI Results???NotMuffy wrote:It looks like there will not only be a battle of Real (American) Football vs. Running Into A Wall Without A Helmet (or Australian whatever the heck you'd call it) but Chicago vs AASM 2008, sleep vs sleep disruption, Good vs Evil (NotMuffy = good, of course) as well as a host of other topics!
But I guess since this topic:
viewtopic/t56120/Sex-Life-and-Apnea-Im-embarrassed.html
puts up double the views in half the time, TechnoFlash and the War of the Continents isn't quite as exciting as I thought and will go underground.
See ya!
There... we now have mass reader appeal! Seriously, thanks for stopping in once again to share your research results, Dr. split_city. It means a lot to me and I'm sure it means a lot to others as well. And thanks to both of you for a great read.
Re: Squishing the belly increases AHI
Maybe we can work Gloria into the header.-SWS wrote:However, if you want to increase readership, the subject line needs to be reworked to something like: Subject: Did Occult/Repressed Sex Drive Confound Our Squished Belly AHI Results???
Ahhhh, Gloria...
"Don't Blame Me...You Took the Red Pill..."
-
CollegeGirl
- Posts: 1038
- Joined: Thu Oct 20, 2005 6:49 pm
- Location: VA
Re: Squishing the belly increases AHI
Forgive my completely unscientific intrusion.
In the vast majority of cases, doesn't supine sleeping at least somewhat eliminate apneas? In a person with quite a lot of abdominal fat, wouldn't this position "squish the belly" quite a bit? If your hypothesis were true, shouldn't it make them worse?
I am a very large (no really... very large) woman with a whole lot of abdominal fat that gets compressed when I sleep on my stomach. Yet, I have far fewer apneas in this position. Obviously one person is anecdotal, but given what we know about supine sleeping meaning fewer apneas for many, I don't see how your hypothesis could be true.
In the vast majority of cases, doesn't supine sleeping at least somewhat eliminate apneas? In a person with quite a lot of abdominal fat, wouldn't this position "squish the belly" quite a bit? If your hypothesis were true, shouldn't it make them worse?
I am a very large (no really... very large) woman with a whole lot of abdominal fat that gets compressed when I sleep on my stomach. Yet, I have far fewer apneas in this position. Obviously one person is anecdotal, but given what we know about supine sleeping meaning fewer apneas for many, I don't see how your hypothesis could be true.
Machine: M-Series Auto
Mask: Headrest
No humidifier
On the hose since 2005.
Mask: Headrest
No humidifier
On the hose since 2005.
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Squishing the belly increases AHI
Nah, that 1439 is not correct. Mine says 04:09 i.e. about 4am. I don't know why yours is different.NotMuffy wrote: OK, matching up the time stamp (about 1439), it looked like SWS on the histogram:
Aldeady discussed. Fot those who missed out, in addition to standard PSG setup, these patients had 3 nasal catheters, 8 cables strapped to their chest and abdomen, an inflatable cuff around the stomach (periods with and without abdominal compression), were asked to remain in one posture (they could buzz and ask to switch position for a short period of time) and wore a nasal mask. Given these were CPAP naive patients, they took a bit of time to get used to the mask. How many of you would get a "good night sleep" with this setup?NotMuffy wrote:Note train-wreck architecture and absence of REM.
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Squishing the belly increases AHI
Sorry, a little confused as you discuss both supine and prone (stomach). OSA is generally worse (not better) when you sleep on your back. Sleeping on your stomach would likely have different results. None of my patients slept prone so I am unsure whether the results from my study can extend to those who sleep on their stomach.CollegeGirl wrote:Forgive my completely unscientific intrusion.
In the vast majority of cases, doesn't supine sleeping at least somewhat eliminate apneas? In a person with quite a lot of abdominal fat, wouldn't this position "squish the belly" quite a bit? If your hypothesis were true, shouldn't it make them worse?
I am a very large (no really... very large) woman with a whole lot of abdominal fat that gets compressed when I sleep on my stomach. Yet, I have far fewer apneas in this position. Obviously one person is anecdotal, but given what we know about supine sleeping meaning fewer apneas for many, I don't see how your hypothesis could be true.
Oh, i do recall my supervisor telling me they tried to run a pilot study years ago (before I worked there), where they removed some of the slats in a wooden bed and had OSA patients sleep prone with their stomach sort of dangling through the hole in the bottom of the bed to see if OSA severity decreased. I don't think the study was very successful as patients were just too uncomfortable.
Last edited by split_city on Fri Oct 08, 2010 7:11 am, edited 1 time in total.
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Squishing the belly increases AHI
No worries. I'll consider a more catchy thread title next time!-SWS wrote:Well, this scientific thread has great esoteric appeal IMHO. I for one enjoy and appreciate the discussion. However, if you want to increase readership, the subject line needs to be reworked to something like: Subject: Did Occult/Repressed Sex Drive Confound Our Squished Belly AHI Results???NotMuffy wrote:It looks like there will not only be a battle of Real (American) Football vs. Running Into A Wall Without A Helmet (or Australian whatever the heck you'd call it) but Chicago vs AASM 2008, sleep vs sleep disruption, Good vs Evil (NotMuffy = good, of course) as well as a host of other topics!
But I guess since this topic:
viewtopic/t56120/Sex-Life-and-Apnea-Im-embarrassed.html
puts up double the views in half the time, TechnoFlash and the War of the Continents isn't quite as exciting as I thought and will go underground.
See ya!
There... we now have mass reader appeal! Seriously, thanks for stopping in once again to share your research results, Dr. split_city. It means a lot to me and I'm sure it means a lot to others as well. And thanks to both of you for a great read.
Re: Squishing the belly increases AHI
Probably got messed up crossing the International Date Line. The point remains, then, that this guy can put up stable Duece.split_city wrote:Nah, that 1439 is not correct. Mine says 04:09 i.e. about 4am. I don't know why yours is different.
NotMuffy wrote:Note train-wreck architecture and absence of REM.
I concur:split_city wrote:Aldeady discussed. Fot those who missed out, in addition to standard PSG setup, these patients had 3 nasal catheters, 8 cables strapped to their chest and abdomen, an inflatable cuff around the stomach (periods with and without abdominal compression), were asked to remain in one posture (they could buzz and ask to switch position for a short period of time) and wore a nasal mask. Given these were CPAP naive patients, they took a bit of time to get used to the mask. How many of you would get a "good night sleep" with this setup?
AND the PLMs.Muffy wrote:What you have presented... suggests you have changed arousal threshold... and made sleep quality worse.
AND perhaps another something or other that wiped out his REM.
"Don't Blame Me...You Took the Red Pill..."
-
split_city
- Posts: 465
- Joined: Mon Apr 23, 2007 2:46 am
- Location: Adelaide, Australia
Re: Squishing the belly increases AHI
Maybe something to consider....NotMuffy wrote:Probably got messed up crossing the International Date Line. The point remains, then, that this guy can put up stable Duece.split_city wrote:Nah, that 1439 is not correct. Mine says 04:09 i.e. about 4am. I don't know why yours is different.
Sleep. 2009 Mar 1;32(3):361-8.
Airway dilator muscle activity and lung volume during stable breathing in obstructive sleep apnea.
Jordan AS, White DP, Lo YL, Wellman A, Eckert DJ, Yim-Yeh S, Eikermann M, Smith SA, Stevenson KE, Malhotra A.
Division of Sleep Medicine, Harvard Medical School, Boston, MA, USA. ajordan@rics.bwh.harvard.edu
Abstract
STUDY OBJECTIVES: Many patients with obstructive sleep apnea (OSA) have spontaneous periods of stable flow limited breathing during sleep without respiratory events or arousals. In addition, OSA is often more severe during REM than NREM and more severe during stage 2 than slow wave sleep (SWS). The physiological mechanisms for these observations are unknown. Thus we aimed to determine whether the activity of two upper airway dilator muscles (genioglossus and tensor palatini) or end-expiratory lung volume (EELV) differ between (1) spontaneously occurring stable and cyclical breathing and (2) different sleep stages in OSA.
DESIGN: Physiologic observation.
SETTING: Sleep physiology laboratory.
STUDY PARTICIPANTS: 15 OSA patients with documented periods of spontaneous stable breathing.
INTERVENTION: Subjects were instrumented with intramuscular electrodes for genioglossus and tensor palatini electromyograms (EMG(GG) and EMG(TP)), chest and abdominal magnetometers (EELV measurement), an epiglottic pressure catheter (respiratory effort), and a mask and pneumotachograph (airflow/ventilation). Patients slept supine overnight without CPAP.
MEASUREMENTS AND RESULTS: Peak and Tonic EMG(GG) were significantly lower during cyclical (85.4 +/- 2.7 and 94.6 +/- 4.7 % total activity) than stable breathing (109.4 +/- 0.4 and 103 +/- 0.8% total activity, respectively). During respiratory events in REM, tonic EMG(GG) activity was lower than during respiratory events in stage 2 (71.9 +/- 5.1 and 119.6 +/- 5.6% total activity). EMG(GG) did not differ between stable stage 2 and stable SWS (98.9 +/- 3.2 versus 109.7 +/- 4.4% total activity), nor did EMG(TP) or EELV differ in any breathing condition/sleep stage.
CONCLUSIONS: Increased genioglossus muscle tone is associated with spontaneous periods of stable flow limited breathing in the OSA subjects studied. Reductions in genioglossus activity during REM may explain the higher severity of OSA in that stage. Increased lung volume and tensor palatini activity do not appear to be major mechanisms enabling spontaneous stable flow limited breathing periods.