General UARS Discussion
Re: General UARS Discussion
This below reply fits into this thread just as well as where it got posted ...
viewtopic/t40126/UARS-and-Spontaneous-A ... -help.html
DSM
viewtopic/t40126/UARS-and-Spontaneous-A ... -help.html
DSM
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)
Re: General UARS Discussion
Some further research on UARS - mostly easy to read.
Here is one paper from a researcher in Edinburgh UK ( albeit dated 2000) who puts the case that UARS as a condition fails to meet the required medical criteria.
(from the American Journal of Respiratory & Critical Care Medicine)
http://ajrccm.atsjournals.org/cgi/conte ... 161/5/1413
EXTRACT:
=========
>>
INTRODUCTION
The term "upper airway resistance syndrome" (UARS [1]) proved useful in highlighting deficiencies in the definition of the sleep apnea/hypopnea syndrome (SAHS). However, UARS is not distinct from SAHS, nor is there adequate evidence that UARS exists.
A syndrome is "a complex of signs and symptoms resulting from a common cause" (2). Thus, a distinct syndrome has distinct signs and symptoms. Patients with UARS usually have no signs---abnormalities on physical examination (2)---and the symptoms of UARS (1, 3) are identical to those for SAHS (4). Thus, UARS is not a distinct syndrome.
Having dismissed UARS on important semantic grounds, it is equally vulnerable medically. To be a distinct condition, it must have the following:
1. 1. Distinct diagnostic criteria
2. 2. Diagnostic criteria that are abnormal
3. 3. Diagnostic criteria that are specific
4. 4. Evidence of a causal link between the diagnostic abnormalities and clinical features (consequent morbidity)
UARS fails on all criteria.
1. DISTINCT DIAGNOSTIC CRITERIA
In the original description (1), diagnosis required sleepiness, a low apnea-hypopnea index (AHI), and frequent arousals. All reported sleepiness but no specific level of subjective or objective sleepiness was required. No subject "had obstructive sleep apnea syndrome as currently defined" but their AHI was not reported. They had to have at least 10 "short" arousals per hour slept. Esophageal pressure was not a diagnostic criterion for UARS (1). Criteria have been further complicated---not clarified---by use of differing AHI thresholds (3, 5), the introduction of esophageal pressure criteria (6, 7), and the possible use of flattening of the flow-time profile to diagnose UARS (8).
Major diagnostic confusion about UARS centers on the scoring of hypopneas. Many centers have scored hypopneas from thermal sensors. These are excellent for detecting apneas, but poor for identifying hypoventilation; exhalations of 50 and 500 ml have identical temperature. Thus, when it was recognized that hypopneas and apneas had similar consequences, and it was recommended that hypopneas should be defined by semiquantative rather than thermal techniques (9) and these now include inductance plethysmography, nasal pressure, and pneumotachography (10). Those centers that use these methods to define hypopneas rarely, if ever, classify patients as having UARS, whereas centers that rely on thermal definitions report UARS frequently (5, 6, 11).
2. DIAGNOSTIC CRITERIA MUST BE ABNORMAL
Sleepiness
The threshold for significant sleepiness is based on self-reports and nearly 20% of women and about 7% of men in the normal population report sleepiness (12). An Epworth score of > 8 has been used (3), but the normal range is up to 12 or even 15 (13).
Low AHI
The criterion of low AHI is deliberately set to define normality.
Arousal
The arousal frequency used to define UARS, > 10 per hour, is normal on the first night of polysomnography whether without (median, 16 [95% confidence interval 6-33] per hour for age < 60 yr [14]) or with (mean, 24 [SD 12] per hour [7]) the sleep-disturbing effect of esophageal pressure monitoring. Thus, it is erroneous to use > 10 arousals per hour as a cutoff for abnormality in patients undergoing polysomnography (1, 5, 6). Indeed, all patients with UARS in some studies have normal arousal frequencies at < 30 per hour (3).
Negative Pleural Pressure
The addition of criteria requiring progressive falls in esophageal pressure seemed sensible, but such falls are not synonymous with increasing resistance, and may also result from increased ventilation. A decreasing pressure over 10 s (6) may mean as few as two consecutive breaths with increasing pressure generation and normal subjects have frequent such episodes, especially during rapid eye movement (REM) sleep (15).
Thus, all four criteria are common in the normal population.
********************************************************************************************************
This researcher argues that it is a distinct medical condition ...
Look at the chapter on page 241 of this book. ... (you can increase the size of the pages using the + and - magnifying glasses in the top middle of the frame)
http://books.google.com.au/books?id=aNh ... lt#PPP8,M1
********************************************************************************************************
Also, it appears that Dr Rapoport is the person who made the association of UARS & Flow Limitations.
DSM
Here is one paper from a researcher in Edinburgh UK ( albeit dated 2000) who puts the case that UARS as a condition fails to meet the required medical criteria.
(from the American Journal of Respiratory & Critical Care Medicine)
http://ajrccm.atsjournals.org/cgi/conte ... 161/5/1413
EXTRACT:
=========
>>
INTRODUCTION
The term "upper airway resistance syndrome" (UARS [1]) proved useful in highlighting deficiencies in the definition of the sleep apnea/hypopnea syndrome (SAHS). However, UARS is not distinct from SAHS, nor is there adequate evidence that UARS exists.
A syndrome is "a complex of signs and symptoms resulting from a common cause" (2). Thus, a distinct syndrome has distinct signs and symptoms. Patients with UARS usually have no signs---abnormalities on physical examination (2)---and the symptoms of UARS (1, 3) are identical to those for SAHS (4). Thus, UARS is not a distinct syndrome.
Having dismissed UARS on important semantic grounds, it is equally vulnerable medically. To be a distinct condition, it must have the following:
1. 1. Distinct diagnostic criteria
2. 2. Diagnostic criteria that are abnormal
3. 3. Diagnostic criteria that are specific
4. 4. Evidence of a causal link between the diagnostic abnormalities and clinical features (consequent morbidity)
UARS fails on all criteria.
1. DISTINCT DIAGNOSTIC CRITERIA
In the original description (1), diagnosis required sleepiness, a low apnea-hypopnea index (AHI), and frequent arousals. All reported sleepiness but no specific level of subjective or objective sleepiness was required. No subject "had obstructive sleep apnea syndrome as currently defined" but their AHI was not reported. They had to have at least 10 "short" arousals per hour slept. Esophageal pressure was not a diagnostic criterion for UARS (1). Criteria have been further complicated---not clarified---by use of differing AHI thresholds (3, 5), the introduction of esophageal pressure criteria (6, 7), and the possible use of flattening of the flow-time profile to diagnose UARS (8).
Major diagnostic confusion about UARS centers on the scoring of hypopneas. Many centers have scored hypopneas from thermal sensors. These are excellent for detecting apneas, but poor for identifying hypoventilation; exhalations of 50 and 500 ml have identical temperature. Thus, when it was recognized that hypopneas and apneas had similar consequences, and it was recommended that hypopneas should be defined by semiquantative rather than thermal techniques (9) and these now include inductance plethysmography, nasal pressure, and pneumotachography (10). Those centers that use these methods to define hypopneas rarely, if ever, classify patients as having UARS, whereas centers that rely on thermal definitions report UARS frequently (5, 6, 11).
2. DIAGNOSTIC CRITERIA MUST BE ABNORMAL
Sleepiness
The threshold for significant sleepiness is based on self-reports and nearly 20% of women and about 7% of men in the normal population report sleepiness (12). An Epworth score of > 8 has been used (3), but the normal range is up to 12 or even 15 (13).
Low AHI
The criterion of low AHI is deliberately set to define normality.
Arousal
The arousal frequency used to define UARS, > 10 per hour, is normal on the first night of polysomnography whether without (median, 16 [95% confidence interval 6-33] per hour for age < 60 yr [14]) or with (mean, 24 [SD 12] per hour [7]) the sleep-disturbing effect of esophageal pressure monitoring. Thus, it is erroneous to use > 10 arousals per hour as a cutoff for abnormality in patients undergoing polysomnography (1, 5, 6). Indeed, all patients with UARS in some studies have normal arousal frequencies at < 30 per hour (3).
Negative Pleural Pressure
The addition of criteria requiring progressive falls in esophageal pressure seemed sensible, but such falls are not synonymous with increasing resistance, and may also result from increased ventilation. A decreasing pressure over 10 s (6) may mean as few as two consecutive breaths with increasing pressure generation and normal subjects have frequent such episodes, especially during rapid eye movement (REM) sleep (15).
Thus, all four criteria are common in the normal population.
********************************************************************************************************
This researcher argues that it is a distinct medical condition ...
Look at the chapter on page 241 of this book. ... (you can increase the size of the pages using the + and - magnifying glasses in the top middle of the frame)
http://books.google.com.au/books?id=aNh ... lt#PPP8,M1
********************************************************************************************************
Also, it appears that Dr Rapoport is the person who made the association of UARS & Flow Limitations.
DSM
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)
Re: General UARS Discussion
Thanks, Doug! Those top-most excerpts were part of that interesting debate mentioned several pages earlier:
viewtopic.php?f=1&t=40009&st=0&sk=t&sd= ... 15#p349995
Yep, here we are a decade later, and that same debate is still going strong in the medical community.
viewtopic.php?f=1&t=40009&st=0&sk=t&sd= ... 15#p349995
Opposing UARS views in 1999:
Upper Airway Resistance Syndrome Is a Distinct Syndrome
Upper Airway Resistance Syndrome Is Not a Distinct Syndrome
And that lack of consensus about UARS carries on to this day. That's science hard at work on one very mysterious SDB problem.
Yep, here we are a decade later, and that same debate is still going strong in the medical community.
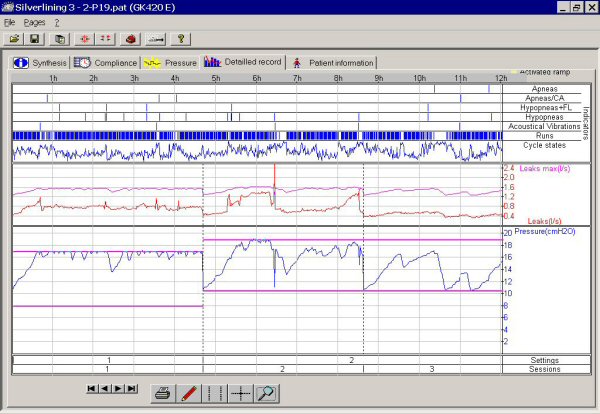
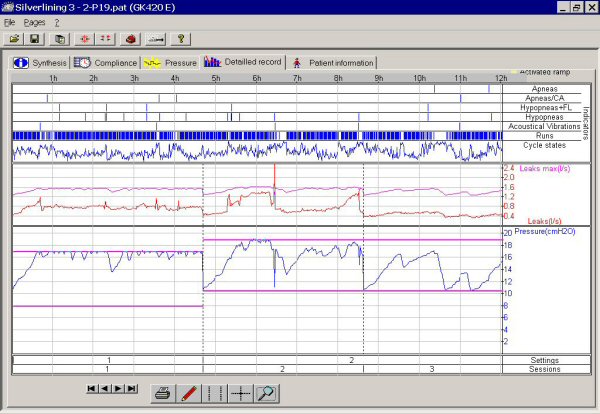
Dr. Rapoport is another giant icon of a researcher IMHO. That's his patented algorithm inside the 420e and Sandman APAP machines. And as APAP algorithms go, his algorithm is the most pressure aggressive when it comes to treating standalone flow limitations. So I suspect that Dr. Rapoport's views of aggressively treating FL may actually be similar to Dr. Krakow's views. Both treatment approaches can intentionally administer a very high pressure to unaccompanied flow limitations. However, I'm not sure how Dr. Rapoport's manual titration protocol (attended multichannel) compares to his APAP algorithm (unattended single-channel) when it comes to pressure-aggressively treating FL unaccompanied by other events.dsm wrote:Also, it appears that Dr Rapoport is the person who made the association of UARS & Flow Limitations.
Re: General UARS Discussion
Dr Krakow told me that any FL comment he made was based on Dr Rapoport's views.-SWS wrote:
<snip>
Dr. Rapoport is another giant icon of a researcher IMHO. That's his patented algorithm inside the 420e and Sandman APAP machines. And as APAP algorithms go, his algorithm is the most pressure aggressive when it comes to treating standalone flow limitations. So I suspect that Dr. Rapoport's views of aggressively treating FL may actually be similar to Dr. Krakow's views.dsm wrote:Also, it appears that Dr Rapoport is the person who made the association of UARS & Flow Limitations.
So that may reflect that one runs sleep clinics & the other does research & designs algorithms ?-SWS wrote: Both treatment approaches can intentionally administer a very high pressure to unaccompanied flow limitations. However, I'm not sure how Dr. Rapoport's manual titration protocol (attended multichannel) compares to his APAP algorithm (unattended single-channel) when it comes to pressure-aggressively treating FL unaccompanied by other events.
DSM
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)
- rested gal
- Posts: 12880
- Joined: Thu Sep 09, 2004 10:14 pm
- Location: Tennessee
Re: General UARS Discussion
Yeah. The FL1 algorithm that has been known to do this to more than one "flow limited" breather on this board:
Pardon me if I just can't bring myself to be very impressed with either doctor's views on dealing with stand-alone flow limitations.
I am impressed, however, with Dr. Rapoport's contributions to bilevel design.
About Dr. Krakow's zero tolerance policy for titrating out all flow limitations:
As I understand it, the syndrome (UARS) has long been defined by its "discoverer", Dr. Guilleminault, as having more going on with it (arousals fragmenting sleep architecture) than just the appearance of what I'd think of as probably a benign degree of flow limited breaths.
Pardon me if I just can't bring myself to be very impressed with either doctor's views on dealing with stand-alone flow limitations.
I am impressed, however, with Dr. Rapoport's contributions to bilevel design.
About Dr. Krakow's zero tolerance policy for titrating out all flow limitations:
You nailed it exactly, imho, jnk. Just call it what titrating 'em out what it is ... getting rid of all flow limitations. Or give it a new name -- Flow Limitations Syndrome.jnk wrote:Maybe what he was attempting to fix shouldn't have been called UARS.
As I understand it, the syndrome (UARS) has long been defined by its "discoverer", Dr. Guilleminault, as having more going on with it (arousals fragmenting sleep architecture) than just the appearance of what I'd think of as probably a benign degree of flow limited breaths.
ResMed S9 VPAP Auto (ASV)
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Re: General UARS Discussion
Well put, Rested Gal.rested gal wrote: . . . Pardon me if I just can't bring myself to be very impressed with either doctor's views on dealing with stand-alone flow limitations.
I am impressed, however, with Dr. Rapoport's contributions to bilevel design.
About Dr. Krakow's zero tolerance policy for titrating out all flow limitations:You nailed it exactly, imho, jnk. Just call it what titrating 'em out what it is ... getting rid of all flow limitations. Or give it a new name -- Flow Limitations Syndrome.jnk wrote:Maybe what he was attempting to fix shouldn't have been called UARS.
As I understand it, the syndrome (UARS) has long been defined by its "discoverer", Dr. Guilleminault, as having more going on with it (arousals fragmenting sleep architecture) than just the appearance of what I'd think of as probably a benign degree of flow limited breaths.
I guess what I find infinitely further unimpressive is the number of sleepy/tired people who do not fall into the OSA box as judged by one tech on one night who are apparently often being told, 'Sorry, pal, nothing we can do for you--your AHI/RERA isn't high enough (yet). Have a nice day!'
What is the alternative to that?
One alternative is to make the assumption that maybe the flow limitations ARE disturbing sleep for THAT patient--even though the events, as imperfectly scored by one tech, don't meet the somewhat arbitrary definitions of hypopnea or RERA--and then to see if titrating away some events helps or hurts sleep for that patient.
What name is a doctor supposed to give that process today if he needs to give insurance an explanation?
Is it OK to make the assumption that a flow limitation can definitively be judged a non-RERA, since one tech may score an event a RERA and another tech might not? Could it be that the "benign degree of flow limited breaths" is very different from one patient to the next?
Calling the process "treating UARS" is a way for docs on the front lines to give a name to their treatment process for any non-OSA patients, even if hijacking that name undermines the work of the researchers trying to establish UARS as a separate well-defined syndrome. Many people showing up at this board saying they were "diagnosed UARS" may fall into the merely-outside-the-OSA-definition-box category and may not technically fall neatly into the box for UARS as a syndrome either. The solution is not to tell them, "You don't really have UARS. You are disqualified. Go turn in your equipment."
So the bottom line for me is still that the main service that the label "UARS" presently provides is to keep alive the notion that there are people who can benefit from PAP therapy who do not meet the definition for OSA. That may not be why the term was coined or how it was originally meant to be used, but that seems to be how it is being used anyway by the doc on the street, if he uses the term at all.
For now, too, I think that anyone needing PAP who doesn't fall into standard vanilla OSA categories would likely do better on a bilevel. But, then again, I look forward to the day when every SDB patient is given a bilevel that can also run in 'monolevel' and autotitrate in either mode.
I realize my views are nonstandard on much of that. So I appreciate everyone putting up with me. I learn from and enjoy all opposing views.
Last edited by jnk on Tue Mar 24, 2009 8:41 am, edited 1 time in total.
Re: General UARS Discussion
Doug, thanks for finding that out. I can definitely see how Dr. Krakow incorporated Dr. Rapoport's FL views as a springboard for his own work and paradigm. Dr. Rapoport's APAP algorithm performs a statistical covariance comparison between each measured inspiratory curve and a perfect sinusoidal template. Dr. Krakow takes that a step further. Dr. Krakow manually "normalizes" both inspiratory and expiriatory flow curves to achieve a perfect sinusoidal waveform on both the top and bottom halves.dsm wrote:Dr Krakow told me that any FL comment he made was based on Dr Rapoport's views.
What's so interesting about a perfect sinusoid? In the energy-based domain of frequency harmonics, a sinusoid represents the most efficient energy transfer that mother nature has to offer.
Are Dr. Krakow's patients really feeling significantly better the following day because of those nicely rounded sinusoidal flow curves? If so, I think it's entirely plausible that they just may be experiencing other important biologic benefits beyond sleep-arousal or even transient blood-gas based mitigation. When clinicians increase pressure only to the extent that FL-based arousals are mitigated, then they have performed the traditional short-sighted (indispensable) task of mitigating disturbances and possibly consolidating sleep architecture.
But when Dr. Krakow takes that a step further, by making it a point to achieve the most energy-efficient transfer possible (reflected by that perfect sinusoid), then he may very well be providing his patients with sustained pathophysiologic benefits more related to neuromuscular WOB improvements itself. For all we know, there may be significant numbers of SDB patients who feel presently unmeasured following-day adverse effects of moderately or even marginally heightened WOB----irrespective of measured FL and/or sleep arousals.
Re: General UARS Discussion
SWS,
I am taking that last post as saying that going for the ideal sinusoidal curves may offer benefits beyond just clearing RERAs.
On this whole topic of UARS, I feel I am reaching some conclusions based on my own constricted nasal breathing & some is opposite of what I was thinking even a short time ago. In a different thread I hd said I thought SVs could benefit some UARS situations. I am ready to qualify that view. JNK may have been closer to the right answer in one of his posts where he replied to my notion that varying the pressure as an SV does should help Flow Limitations (as UARS) JNK said he thought it would make it worse. I know that in my own case I have an inability to draw good flows of air through my nose. This goes back to childhood when I had operations on my nose to try to 'straighten the inside' - at school I played sports with a special nose guard to protect it. IF I grab my nares with thumbs & forefingers & open my nose the air flows very freely, let go & it slows noticeably.
I had been to my doctor 18 months ago to explore surgery but he asked me to do an extended trial using Nasonex & in balance doing that has made a noticeable improvement - losing weight has also helped. But I am acutely aware that with the Vpap Adapt SV (vs the Bipap Auto SV) if I breathe through my nose alone, the machine immediately begins stepping up the pressure. I am guessing it is straight away seeing flattening of the curve & responding with PS. If it were simply a FL & not an issue with lack of air being able to get through, then I believe the SV would be helping but in my case it is just an inability to get enough air through (sucking air through a straw) and so adding PS does nothing because that air just can't get through any better.
As soon as this PS happens I start breathing through my mouth & the machine reverts to normal. The Bipap Auto SV is far more tolerant but the prior Bipap models were not.
By chance, I just sold a Vpap III machine to someone who collected it yesterday & when I saw this person, he was what I would call of slight build & in no way overweight & with a very normal looking nose & neck. I asked him with some surprise why he needed cpap. He commented that he had always had difficulty breathing through his nose & had only recently had some surgery to reinforce his nose structure to let more air in and it had made the world of difference to him. He commented that he could hear how I sounded & that reminded him of how he used to be. My nose is better than it has been (as mentioned).
So, my comments re SV & UARS is that if the issue a person has is not related to restricted airflow due to nose structure, an SV *may* be of help but if the UARS problem is related to nasal structure & flow being restricted by it, then PS is not going to help. I am now going to see my doctor again and ask him for a referral to a good ENT.
DSM
I am taking that last post as saying that going for the ideal sinusoidal curves may offer benefits beyond just clearing RERAs.
On this whole topic of UARS, I feel I am reaching some conclusions based on my own constricted nasal breathing & some is opposite of what I was thinking even a short time ago. In a different thread I hd said I thought SVs could benefit some UARS situations. I am ready to qualify that view. JNK may have been closer to the right answer in one of his posts where he replied to my notion that varying the pressure as an SV does should help Flow Limitations (as UARS) JNK said he thought it would make it worse. I know that in my own case I have an inability to draw good flows of air through my nose. This goes back to childhood when I had operations on my nose to try to 'straighten the inside' - at school I played sports with a special nose guard to protect it. IF I grab my nares with thumbs & forefingers & open my nose the air flows very freely, let go & it slows noticeably.
I had been to my doctor 18 months ago to explore surgery but he asked me to do an extended trial using Nasonex & in balance doing that has made a noticeable improvement - losing weight has also helped. But I am acutely aware that with the Vpap Adapt SV (vs the Bipap Auto SV) if I breathe through my nose alone, the machine immediately begins stepping up the pressure. I am guessing it is straight away seeing flattening of the curve & responding with PS. If it were simply a FL & not an issue with lack of air being able to get through, then I believe the SV would be helping but in my case it is just an inability to get enough air through (sucking air through a straw) and so adding PS does nothing because that air just can't get through any better.
As soon as this PS happens I start breathing through my mouth & the machine reverts to normal. The Bipap Auto SV is far more tolerant but the prior Bipap models were not.
By chance, I just sold a Vpap III machine to someone who collected it yesterday & when I saw this person, he was what I would call of slight build & in no way overweight & with a very normal looking nose & neck. I asked him with some surprise why he needed cpap. He commented that he had always had difficulty breathing through his nose & had only recently had some surgery to reinforce his nose structure to let more air in and it had made the world of difference to him. He commented that he could hear how I sounded & that reminded him of how he used to be. My nose is better than it has been (as mentioned).
So, my comments re SV & UARS is that if the issue a person has is not related to restricted airflow due to nose structure, an SV *may* be of help but if the UARS problem is related to nasal structure & flow being restricted by it, then PS is not going to help. I am now going to see my doctor again and ask him for a referral to a good ENT.
DSM
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)
- rested gal
- Posts: 12880
- Joined: Thu Sep 09, 2004 10:14 pm
- Location: Tennessee
Re: General UARS Discussion
That could certainly be the case for some individuals. Yes. Good point.jnk wrote:One alternative is to make the assumption that maybe the flow limitations ARE disturbing sleep for THAT patient--even though the events, as imperfectly scored by one tech, don't meet the somewhat arbitrary definitions of hypopnea or RERA--and then to see if titrating away some events helps or hurts sleep for that patient.
What name is a doctor supposed to give that process today if he needs to give insurance an explanation?
Is it OK to make the assumption that a flow limitation can definitively be judged a non-RERA, since one tech may score an event a RERA and another tech might not? Could it be that the "benign degree of flow limited breaths" is very different from one patient to the next?
Again, you make a very good point.jnk wrote:Calling the process "treating UARS" is a way for docs on the front lines to give a name to their treatment process for any non-OSA patients, even if hijacking that name undermines the work of the researchers trying to establish UARS as a separate well-defined syndrome.
ok, I can go along with that.jnk wrote:So the bottom line for me is still that the main service that the label "UARS" presently provides is to keep alive the notion that there are people who can benefit from PAP therapy who do not meet the definition for OSA. That may not be why the term was coined or how it was originally meant to be used, but that seems to be how it is being used anyway by the doc on the street, if he uses the term at all.
Very plausible.-SWS wrote: Are Dr. Krakow's patients really feeling significantly better the following day because of those nicely rounded sinusoidal flow curves? If so, I think it's entirely plausible that they just may be experiencing other important biologic benefits beyond sleep-arousal or even transient blood-gas based mitigation.
I would ask this about which patients are feeling significantly better the following day. Which of these are we talking about...
A. patients who had been not feeling better on CPAP that were now being titrated on a bilevel machine, which can provide much more comfortable "breathing out" than CPAP. Wouldn't surprise me at all that in getting to experience breathing on a bilevel machine, they would report feeling better -- even if IPAP were titrated only to the point of preventing flow limited arousals (RERAs) and not raised on up to the point Dr. K would take it.
B. new patients -- never been on any kind of positive airway pressure treatment -- who feel better after their very first experience with it, especially with the comfort of bilevel delivery of separate inhale/exhale pressures. Perhaps those people would feel equally good with a traditional bilevel titration as with a zero flow limitations titration.
C. patients who had not been doing well on bilevel reporting that after a "Dr. K style" titration, they felt better. Now those, I can see, could fall into the realm you and jnk are considering. Non-arousal-causing flow limitations that are seen on the PSG, but are not considered to need anything to be done about them by current PSG standards. Possibly causing a problem for certain people. Those might very well do better if all breaths are rounded out perfectly with additional IPAP pressure than is currently considered necessary in a standard PSG bilevel titration.
My guesstimate is that for most people that is sufficient for good sleep, good breathing while sleeping, and is truly effective positive air pressure treatment.-SWS wrote:When clinicians increase pressure only to the extent that FL-based arousals are mitigated, then they have performed the traditional short-sighted (indispensable) task of mitigating disturbances and possibly consolidating sleep architecture.
If a person does not benefit from a "standard" titration that achieves consolidation of sleep architecture, keeps the O2 level up nicely, and helps them feel better after treatment, I think I'd look first at other factors that could be keeping a person from feeling good -- other health or sleep hygiene factors that have nothing to do with needing more pressure to round out every breath.
Right. Even slightly elevated Work of Breathing without arousals could affect some people. I kind'a doubt it's significant numbers of people, but as you say... "for all we know"... there could be.-SWS wrote:But when Dr. Krakow takes that a step further, by making it a point to achieve the most energy-efficient transfer possible (reflected by that perfect sinusoid), then he may very well be providing his patients with sustained pathophysiologic benefits more related to neuromuscular WOB improvements itself. For all we know, there may be significant numbers of SDB patients who feel presently unmeasured following-day adverse effects of moderately or even marginally heightened WOB----irrespective of measured FL and/or sleep arousals.
My concern about a Dr. K style titration as "standard protocol" (which it seems to be in his clinic, but I may be wrong about that) is that it would be overkill for most people, and would result in a poor tradeoff when it comes to mask sealing ability. Beautifully rounded breath waveforms achieved at high pressures to the detriment of maintaining a good mask seal. I can imagine mask leaks here, there, and yonder at unnecessarily (for most people, imho) high pressures.
ResMed S9 VPAP Auto (ASV)
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Re: General UARS Discussion
My personal opinion on that is based strictly on assumptions and not at all on any firsthand (or second- or third-, for that matter) knowledge. All I meant was that any machine with a timed backup or that constantly plays with the spread between IPAP and EPAP would seem to me likely to be a sleep-disturber for anyone with a sensitive throat or who is easily aroused by minor flow changes.dsm wrote:. . . JNK may have been closer to the right answer in one of his posts where he replied to my notion that varying the pressure as an SV does should help Flow Limitations (as UARS) JNK said he thought it would make it worse. . . .
That may be one of the reasons why, as was mentioned before by -SWS, there seems to be no connection made in any literature between UARS and SV. You would think that if there was a chance one of those machines could help UARS that there would be at least one rogue doctor out there who would go on record as having tried it.
Re: General UARS Discussion
JNK,jnk wrote:My personal opinion on that is based strictly on assumptions and not at all on any firsthand (or second- or third-, for that matter) knowledge. All I meant was that any machine with a timed backup or that plays with the spread between IPAP and EPAP would seem to me likely to be a sleep-disturber for anyone with a sensitive throat or who is easily aroused by minor flow changes.dsm wrote:. . . JNK may have been closer to the right answer in one of his posts where he replied to my notion that varying the pressure as an SV does should help Flow Limitations (as UARS) JNK said he thought it would make it worse. . . .
That may be one of the reasons why, as was mentioned before by -SWS, there seems to be no connection made in any literature between UARS and SV. You would think that if there was a chance one of those machines could help UARS that there would be at least one rogue doctor out there who would go on record as having tried it.
I tend to think that UARS is so fragmented in its definitions that no one has bothered to do any such research. Why would they if there is no adequate definition of which UARS they are testing ?. UARS is just too broad a spectrum of issues (syndrome) & there is in my mind ample evidence of two very different classes of UARS sufferers, one being unrelated to OSA & it is in that category I lean toward SV being of no help.
DSM
#2 I think there is a consensus that UARS is not an accepted medical condition, yet.
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)
Re: General UARS Discussion
Well, the big question is whether following-day benefits are really happening versus perceived. And if those benefits are happening, whether there are yet other confounding factors that may be positively skewing those following-day results in a beneficial manner. Hence the purpose of structured methodology, replication, peer review, etc.rested gal wrote:Very plausible.-SWS wrote: Are Dr. Krakow's patients really feeling significantly better the following day because of those nicely rounded sinusoidal flow curves? If so, I think it's entirely plausible that they just may be experiencing other important biologic benefits beyond sleep-arousal or even transient blood-gas based mitigation.
I would ask this about which patients are feeling significantly better the following day. Which of these are we talking about...
A...
B...
C...
With that said I think your A, B, C's represent some extremely nice initial steps in methodology. But there's plenty of room here for eventual methodology rather than heuristic intuition. One intriguing possibility that comes to mind would be to draw up some kind of composite index that just may be able to numerically reflect a patient's physiologic predisposition toward "respiratory loading". That attempted composite index might be comprised from various contributing physiologic factors or conditions that comprise aggregate diaphragmatic work load. Then employ that diaphragmatic work-load index across the SDB patient population searching for correlation between patients like Dr. Krakow's who reflected not only an increased composite WOB index, but who also reported favorable following-day energy benefits from perfectly normalized, perfectly sinusoidal I and E flow curves. That's only one off-the-cuff proposed methodology in search of sustained benefits beyond simply measuring short-termed FL and arousals.
But I'm sure medical researchers can come up with much better-considered methodologies if there really are following-day benefits to investigate here.
Well, that's an entirely different avenue of research that sleep medicine has been focusing on for quite some time. I think you are saying that you would displace research in areas such as biokinetic energy transfer and oxidative stress with better clinical practices. Well, the good news is those two are not and should not be mutually exclusive. Clinical practices should be improved across the board and research should continue across the board as well.rested gal wrote:My guesstimate is that for most people that is sufficient for good sleep, good breathing while sleeping, and is truly effective positive air pressure treatment.-SWS wrote:When clinicians increase pressure only to the extent that FL-based arousals are mitigated, then they have performed the traditional short-sighted (indispensable) task of mitigating disturbances and possibly consolidating sleep architecture.
If a person does not benefit from a "standard" titration that achieves consolidation of sleep architecture, keeps the O2 level up nicely, and helps them feel better after treatment, I think I'd look first at other factors that could be keeping a person from feeling good -- other health or sleep hygiene factors that have nothing to do with needing more pressure to round out every breath.
So I think that Dr. Krakow's experimental BiLevel work of achieving an energy-efficient sinusoidal work-load transfer points much more in the direction of investigating sustained pathopysiologic benefits related to neuromuscular WOB itself, than exclusively putting the call out for better sleep hygiene and improved clinical practices. But that's assuming his patients really are gaining significant benefits because of those perfect sinusoids. As it turns out, they may not be.
Here's one possible area in biochemistry to take a closer look at relative to those perfectly sinusoidal energy transfers:
Respiratory loading intensity and diaphragm oxidative stress: N-acetyl-cysteine effects
Last edited by -SWS on Tue Mar 24, 2009 10:16 pm, edited 1 time in total.
Re: General UARS Discussion
What I hear SWS saying is that if pushing for a 'good' well rounded (sinusoidal) I & E curve raised the WOB index (makes breathing more efficient), then Dr Krakow may be onto the right approach to titration.
RG & I then raise the specter of mask management messing it all up (based on our real world experience & the repeated stories we read here at cpaptalk).
SWS I believe that last link was to highlight side issues to do with diaphragm effort - an aspect of WOB. "We hypothesized that resistive breathing of moderate to high intensity might increase diaphragm oxidative stress, which could be partially attenuated by antioxidants".
I am taking it that the WOB index (an indicator of respiratory efficiency) is something that can be measured and should be part of a 'proof' as to titration effectiveness.
DSM
RG & I then raise the specter of mask management messing it all up (based on our real world experience & the repeated stories we read here at cpaptalk).
SWS I believe that last link was to highlight side issues to do with diaphragm effort - an aspect of WOB. "We hypothesized that resistive breathing of moderate to high intensity might increase diaphragm oxidative stress, which could be partially attenuated by antioxidants".
I am taking it that the WOB index (an indicator of respiratory efficiency) is something that can be measured and should be part of a 'proof' as to titration effectiveness.
DSM
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)
Re: General UARS Discussion
Agreed. But that's a big IF even in my opinion (not just rested gal's). But that WOB index would theoretically be lowered, since a PAP-assisted sinusoidal flow curve represents less neuromuscular work (lower WOB index) versus more work (higher WOB index).dsm wrote:What I hear SWS saying is that if pushing for a 'good' well rounded (sinusoidal) I & E curve raised the WOB index (makes breathing more efficient), then Dr Krakow may be onto the right approach to titration.
I absolutely agree with both of you on that point. High pressures thrown at any interface stand to be a HUGE spoiler in my opinion as well. Yet more reason to address other contributing factors such as nasal resistance IMHO---to bring the required BiLevel PS down to a "mask friendly" level of pressure.dsm wrote:RG & I then raise the specter of mask management messing it all up (based on our real world experience & the repeated stories we read here at cpaptalk).
Right. Extra respiratory "effort" is synonymous in this context with extra respiratory "work". Extra neuromuscular effort or work translates to oxidative stress in cellular biochemistry. That's a WOB factor that can be scrutinized irrespective of FL or sleep arousals.dsm wrote:SWS I believe that last link was to highlight side issues to do with diaphragm effort - an aspect of WOB. "We hypothesized that resistive breathing of moderate to high intensity might increase diaphragm oxidative stress, which could be partially attenuated by antioxidants".
The closest current measurement for respiratory effort is negative esophageal pressure via PES. That specifically measures inspiratory effort. My off-the-cuff half-considered thought was aimed more at the prospect of devising a composite predictive risk-factor type index for WOB irrespective of impractical PES measurement.dsm wrote:I am taking it that the WOB index (an indicator of respiratory efficiency) is something that can be measured and should be part of a 'proof' as to titration effectiveness.
Here's one proposed three-dimensional model that attempts to predictively isolate only the UARS factors contributing to WOB: http://www.angle.org/anglonline/?reques ... &page=0791. Since WOB is influenced by the sum total of all contributing factors, more than just upper airway resistance needs to be rolled into a WOB index IMO.
Last edited by -SWS on Tue Mar 24, 2009 5:38 pm, edited 1 time in total.
Re: General UARS Discussion
SWS,
got that re the index - lower WOB index being more efficient. Higher WOB index means less efficient.
Tks
DSM
got that re the index - lower WOB index being more efficient. Higher WOB index means less efficient.
Tks
DSM
xPAP and Quattro std mask (plus a pad-a-cheek anti-leak strap)









