san_fran_gal,
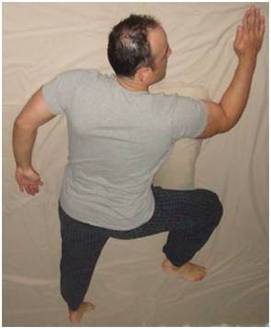
You've inspired me to get my photos of this sleeping position accomplished, as I promised.
Here they are below. Thanks for the nomination to give the 'partial swastika sleeping position' a new name...and call it the Falcon Position!
Actually, I can't take full credit for this sleeping position. I remembered seeing it a long time ago on a re-run of an old Merv Griffin show. A sleep expert (don't recall his name) was one of Merv's guests, and he told Merv and the audience about this position. He said that studies and surveys had been done, and this was found to be the most comfortable position among all other sleeping positions. (Personally, I found that it actually took a little time to get used to it, when I first tried it. Now I find it extremely comfortable.) The guest also said that this sleeping position was one of the best for alignment, as well, since the spine of your neck, torso, and hips stay lined-up with each other.
The mental image I saw on that talk show episode stayed with me, and about three years ago I started to experiment and use this position at night. I found that it really helped significantly with somewhat reducing my sleep-disordered breathing related symptoms, in conjunction with my other treatment approaches, especially compared with back-sleeping (with or without a pillow, neck roll, etc) or side-sleeping positions.
As I mentioned previously, with this sleeping position, the head is kept turned completely to the side, while it rests flat against the bed.
The body is not actually completely prone, since the chest and abdomen stay lifted up off of the bed somewhat, because of the bend in the hip of one leg, which keeps the torso/abdomen propped up a bit.
For added support and comfort, I like to keep a pillow under the half of my chest and abdomen which is lifted up slightly off the bed. You can see the pillow that I have under my chest/abdomen in the photos.
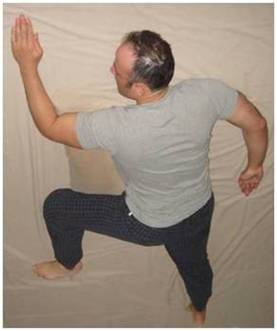
Left-facing position:
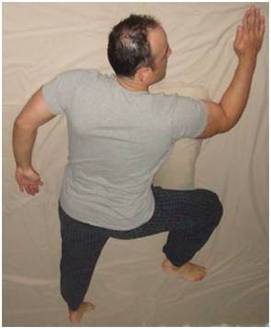
Right-facing position:
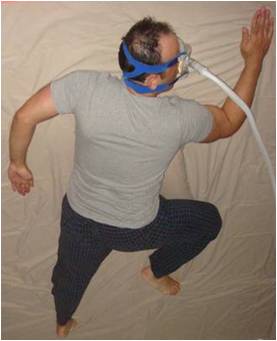
As I mentioned before, this sleeping position is also very compatible with cpap gear, in my experience. Back when I was using my cpap machine and facemask/headgear, I slept in this position very consistently and effectively each night, without any interference.
Today, I went and dug my cpap mask out of the closet where it's been for the past two years (since I no longer need cpap treatment), and took these photos, to demonstrate that this sleeping position is compatible with facemask/headgear usage.
Left-facing position, with facemask/headgear:

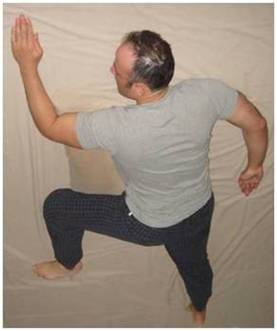
Right-facing position, with facemask/headgear:
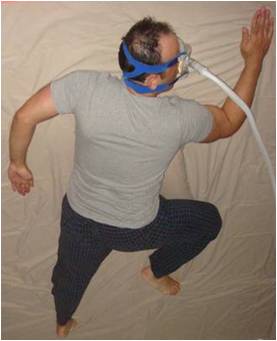
With practice and conditioning, I found that I was able to become accustomed to being able to switch from the left-facing position to the right-facing position while asleep, without any interference to my facemask/ headgear, for a greater degree of variety and comfort during the night. At first, I practiced this switching from left-facing to right-facing several times, consciously, before falling asleep at night for a couple of weeks. Then, my subconscious took over and I was able to switch from left- to right-facing a few times during the night while asleep, without interruption of my sleep.
For those that didn't see it earlier on page 1 of this forum string, here's the excerpt again from my ebook, at
http://www.uarsrelief.com, which I wrote on the topic of "Sleeping Positions".
Best regards!
--------------------------------------------------------------------------
SLEEPING POSITIONS - by Eric Falcon, MD
It is widely accepted that sleeping on your back tends to worsen all forms of sleep-disordered breathing, including UARS, sleep apnea, and snoring. Sleeping on the back allows gravity to pull the soft tissues of the palate, or the tongue, down into the back of the throat and cause airway narrowing, or as in the case of sleep apnea, complete obstruction.
Some doctors will even go so far as to advise patients with sleep-disordered breathing to sew a pocket into the back of their pajamas so that a tennis ball may be kept in it at night. After rolling onto your back at night during sleep and repeatedly experiencing the discomfort of the tennis ball continuously there, you soon "train" your subconscious mind to learn to avoid this sleeping position all together.
An easier alternative to sewing a pocket in the back of your pajamas is to just go out and buy a Dickies T-shirt or other type of T-shirt (which you can usually find in the men's section of K-mart) that has a pocket in the front upper left of the shirt. Simply put the shirt on backwards and place the tennis ball in the pocket, which is now in the upper right of the back. You get the same effect!
Sleeping on your side is preferable to sleeping on your back. When sleeping on your side try to keep your head, torso, and pelvis all in a straight line (when viewed from behind), which is a neutral anatomical position that will help to keep your spine in alignment. You can achieve this result by using a pillow of the proper height under your head and also by placing a flat pillow between your knees. Also, keep your knees and hips in a relaxed but flexed position and bent at 90 degree angles.
Many authorities feel that sleeping on the stomach, known as the "prone" position, is not a good idea. The reason for this is because it can lead to improper alignment of the spine, and because it can also place excessive pressure on the gastrointestinal organs throughout the night.
Yet doctors routinely advocate that patients with sleep-disordered breathing sleep on their stomach or side, however, and avoid sleeping on their backs. By sleeping on your side, or on your stomach with your head turned off to the side, this elicits the pull of gravity to cause the soft tissues of the palate and the tongue to fall somewhat forward and away from the back of the throat, preventing them from narrowing or obstructing the airway.
Believe it or not there actually is a PRONE sleeping position I have found which I believe retains the beneficial effects of gravity on the tissues of the back of the throat and tongue, as well as maintains some degree of proper spinal alignment, and also avoids excessive pressure on the internal organs.
This is often called the SWASTIKA SLEEPING POSITION (it's really only a PARTIAL swastika shape) because of the position of the arms, which are pointed in opposite directions away from each other, with the shoulders and the elbows bent at ninety degree angles.
Here's a complete description of the SWASTIKA SLEEPING POSITION: To start out with, first lay flat on your belly for a second and turn your head to the left. Now, bring your left arm up so that your upper arm is extending out at a ninety degree angle to the side of your torso, and your left elbow is bent ninety degrees, with your left hand pointing up away from your feet. (Your left hand ends up being next to your face, in this position.)
Next, extend your right arm out to the opposite side of your body at a ninety degree angle and bend your right elbow ninety degrees as well, with your right hand pointing down towards your feet. (You arms will now form a 'half-swastika' shape.)
Next, bring your left thigh up so that your left hip and knee are each bent at ninety degree angles. Keep the right leg extended straight downward, with no bend at the knee or hip. In this position you will find that your abdomen/belly and chest will be lifted slightly off of the bed, so that there is not a feeling of excessive pressure on your gastrointestinal organs. For added support and comfort, you can place a pillow under the left half of your chest and abdomen.
I find this to be an incredibly comfortable position which I can remain in all night long with no discomfort. By the way, no pillow is used under the head in this sleeping position. The side of your face rests directly on your flat bed and the spine of your neck, torso, and hips should all line up in a straight line.
You can also switch to the exact opposite side, using the swastika sleeping position, so that you're looking to the right instead, with your right hand now up in front of your face and your right knee and hip bent, and your left leg straight. Basically just use the same steps as I described above but replace the terms "left" with "right" and vice-versa.
Aside: Although this is my favorite sleeping position, I really DISLIKE the NAME that was given to it, for OBVIOUS REASONS! The image of a swastika however seems to help people who've never seen this sleeping position before to visualize it better, and so the term helps a bit when attempting to describe this sleeping position to others. Nonetheless, I sure hope someone comes up with a better name for it sometime soon!
12/4/08 PostScript: A nomination has been proposed to give this sleep position the new name of the "Falcon Position." I'm honored!