Interpreting CPAP results
-
walshsurvey
Interpreting CPAP results
Hi:
Here's the story...I've had fatigue for 9 years now. Major fatigue, sleeping 14 hours a night and still not feeling rested fatigue, but I've had 3 sleep studies (2 night one day) and they all show me with no apneas. My GP sent me to a sleep doc to see what he had to say. He gave me a script for a CPAP machine, saying that in some cases CPAP is not detectable, but if the CPAP helps me then the proof will be in the pudding as it were. I've gotten the cpap, used it most every night until I take it off in my sleep. I walk in my sleep, go get mail in my sleep, so taking off a mask is no problem for me.
I went to see the CPAP guy today and they gave me a printout of the results:
There are lots of pages but this one looked important:
Auto-CPAP Mean Pressure: 6.2 cm H2O
Auto-CPAP peak average pressure: 8.2 cm H2O
Average Device Pressure <= 90% of the time: 7.6 cm H2)
Average time in apnea per day: 17.6 secs
Average Time in Large Leak per day: 1.1 mins
Average AHI: 1.9
Thanks,
Connie
Here's the story...I've had fatigue for 9 years now. Major fatigue, sleeping 14 hours a night and still not feeling rested fatigue, but I've had 3 sleep studies (2 night one day) and they all show me with no apneas. My GP sent me to a sleep doc to see what he had to say. He gave me a script for a CPAP machine, saying that in some cases CPAP is not detectable, but if the CPAP helps me then the proof will be in the pudding as it were. I've gotten the cpap, used it most every night until I take it off in my sleep. I walk in my sleep, go get mail in my sleep, so taking off a mask is no problem for me.
I went to see the CPAP guy today and they gave me a printout of the results:
There are lots of pages but this one looked important:
Auto-CPAP Mean Pressure: 6.2 cm H2O
Auto-CPAP peak average pressure: 8.2 cm H2O
Average Device Pressure <= 90% of the time: 7.6 cm H2)
Average time in apnea per day: 17.6 secs
Average Time in Large Leak per day: 1.1 mins
Average AHI: 1.9
Thanks,
Connie
Re: Interpreting CPAP results
Hello & Welcome,
Obtain copies of all your sleep studies and post them here for more opinions. Since you have started CPAP, if it were me, I would continue it to see if I felt a difference.
Good Luck, and stay around for advice that should help.
Georgio
Obtain copies of all your sleep studies and post them here for more opinions. Since you have started CPAP, if it were me, I would continue it to see if I felt a difference.
Good Luck, and stay around for advice that should help.
Georgio
DreamStation 2, Oscar
Resmed AirFit P30i Nasal Mask
Resmed AirFit P30i Nasal Mask
-
walshsurvey
Re: Interpreting CPAP results
Here is one of my sleep studies data:
Epworth sleepiness scale:16.
No report of snoring or witnessed apnea
Sleep onset latency was 3 minutes
Sleep efficiency high at 97%
Number of wakenings: 6
Normal amounts of sleep
REM sleep increased at 94 minutes
REM sleep latency was normal at 103 minutes.
Respiratory disturbance: 1 event/hour
Ox Sat: 97% and did not fall below 94%
Sinus rhythm was present
No restless leg
That's all it has.
Connie
Epworth sleepiness scale:16.
No report of snoring or witnessed apnea
Sleep onset latency was 3 minutes
Sleep efficiency high at 97%
Number of wakenings: 6
Normal amounts of sleep
REM sleep increased at 94 minutes
REM sleep latency was normal at 103 minutes.
Respiratory disturbance: 1 event/hour
Ox Sat: 97% and did not fall below 94%
Sinus rhythm was present
No restless leg
That's all it has.
Connie
Re: Interpreting CPAP results
Hi Connie,
Since CPAP was prescribed, hopefully it will make a difference for you. I think, "Ox Sat: 97% and did not fall below 94%" is a good thing for you. I hope one of the resident experts will be able to offer you more advice.
Georgio
Since CPAP was prescribed, hopefully it will make a difference for you. I think, "Ox Sat: 97% and did not fall below 94%" is a good thing for you. I hope one of the resident experts will be able to offer you more advice.
Georgio
DreamStation 2, Oscar
Resmed AirFit P30i Nasal Mask
Resmed AirFit P30i Nasal Mask
-
walshsurvey
Re: Interpreting CPAP results
If you ask me I don't even have apnea. I don't snore. I sleep like a baby. Nothing wakes me up. I mean most mornings I wouldn't wake up with my alarm at full blare.
Anyway, I would really appreciated it if someone could take pity on a noob and look at my results and see if there is anything out of whack.
Blessings,
Connie
Anyway, I would really appreciated it if someone could take pity on a noob and look at my results and see if there is anything out of whack.
Blessings,
Connie
Re: Interpreting CPAP results
Most here have been diagnosed with Obstructive Sleep Apnea Syndrome or one of the related syndromes involving some sort of apneas or at least some air flow limitations. From the perspective of those problems, your numbers look better than good. Nothing "out of whack" in the info you gave. You may be better off than the average person on the street, in fact.
If a sleep study was done, then your doc has paperwork that has some 8 or 9 pages of information from that study. That may have information that could be explained to you by some who post here, if you can post any of that. (The law in the U.S. says that patients are entitled to a copy.) Some here might be curious to know exactly what the doc saw that made him/her think you might be a candidate for PAP therapy.
If a sleep study was done, then your doc has paperwork that has some 8 or 9 pages of information from that study. That may have information that could be explained to you by some who post here, if you can post any of that. (The law in the U.S. says that patients are entitled to a copy.) Some here might be curious to know exactly what the doc saw that made him/her think you might be a candidate for PAP therapy.
Re: Interpreting CPAP results
If you can scan your entire report, upload it to photobucket, and post a link to it here, maybe someone can offer more advice.
Georgio
Georgio
DreamStation 2, Oscar
Resmed AirFit P30i Nasal Mask
Resmed AirFit P30i Nasal Mask
-
walshsurvey
Re: Interpreting CPAP results
That's all I needed to know. I am in Canada. The sleep study doc said that there was nothing out of place in my sleep study results just that there was a study done and 20% of people with sleep apnea aren't detected during sleep study. It was an experiment and it seems like this is not my answer...off to tilt at some more windmills.jnk wrote:Most here have been diagnosed with Obstructive Sleep Apnea Syndrome or one of the related syndromes involving some sort of apneas or at least some air flow limitations. From the perspective of those problems, your numbers look better than good. Nothing "out of whack" in the info you gave. You may be better off than the average person on the street, in fact.
If a sleep study was done, then your doc has paperwork that has some 8 or 9 pages of information from that study. That may have information that could be explained to you by some who post here, if you can post any of that. (The law in the U.S. says that patients are entitled to a copy.) Some here might be curious to know exactly what the doc saw that made him/her think you might be a candidate for PAP therapy.
Thank you for taking the time to look at my data. I have a follow up with the sleep study doc in a couple of weeks. I will see if he concurs with you.
Connie
-
fortomorrow
- Posts: 174
- Joined: Thu Sep 11, 2008 9:57 am
- Location: Sacramento, CA
Re: Interpreting CPAP results
I'm not a medical professional (nor do I always have a high opinion of them) but if I were in that situation I'd feel like he gave me the CPAP to placate me. Your sleep info looks great. Your desats are normal, your sleep efficiency is awesome, you're hitting REM sleep.
I'd find a new doctor, to be honest, or at least try to get a second opinion from a neurologist that specialises in sleep disorders. I don't know how difficult that would be in Canada.
There are so many other things that could be causing your hypersomnia, I can't even begin to imagine why your doctor prescribed CPAP with those sleep study results. Have you been checked for MS or CFS?
http://en.wikipedia.org/wiki/Sleep_disorder
I'd find a new doctor, to be honest, or at least try to get a second opinion from a neurologist that specialises in sleep disorders. I don't know how difficult that would be in Canada.
There are so many other things that could be causing your hypersomnia, I can't even begin to imagine why your doctor prescribed CPAP with those sleep study results. Have you been checked for MS or CFS?
http://en.wikipedia.org/wiki/Sleep_disorder
Have you always wanted to try the Liberty? Test drive it here!
-
walshsurvey
Re: Interpreting CPAP results
No I would say he is right on the money: http://www.talkaboutsleep.com/sleep-dis ... andard.htmfortomorrow wrote:I'm not a medical professional (nor do I always have a high opinion of them) but if I were in that situation I'd feel like he gave me the CPAP to placate me. Your sleep info looks great. Your desats are normal, your sleep efficiency is awesome, you're hitting REM sleep.
I'd find a new doctor, to be honest, or at least try to get a second opinion from a neurologist that specialises in sleep disorders. I don't know how difficult that would be in Canada.
There are so many other things that could be causing your hypersomnia, I can't even begin to imagine why your doctor prescribed CPAP with those sleep study results. Have you been checked for MS or CFS?
http://en.wikipedia.org/wiki/Sleep_disorder
He did a trial, it did not work...he is not a bad doctor because he acted on some research...
I have been diagnosed with CFS. But CFS, is just a diagnosis based on symptoms, it is a catch all. There may be some underlying reason for the problem, which is what I'm trying to find out.
Thank you for the time to respond!! It is kind of bittersweet ruling one more thing out.
God Bless,
Connie
Re: Interpreting CPAP results
walshsurvey,
I applaud that you are working with your doctor. I applaud that you and he are both willing to try things to see if they make a difference. I also applaud your checking up on things (and him) in this forum the way you did. Your positive, proactive, involved approach should do you good in your search for what will help.
I once met the criteria for CFS. And my doctor told me that fact, like a good doc should. But he also said that he would not make that his official diagnosis, for much the same reason you just gave. He didn't want to 'wash his hands of me and stop trying things,' as he put it. And it took a few years, but I eventually no longer met the CFS criteria.
I wish you well as you continue to explore what mainstream medicine has to offer. Don't give up on it until you have to. But don't get discouraged if you seem to exhaust all it has to offer, either, since some respond to treatments slightly outside the mainstream, once it comes to that.
Keep thinking as logically as you are. Try one thing at a time. Don't forget the basics of good health as you go about your search with your positive attitude.
We all wish you well, walshsurvey.
jeff
I applaud that you are working with your doctor. I applaud that you and he are both willing to try things to see if they make a difference. I also applaud your checking up on things (and him) in this forum the way you did. Your positive, proactive, involved approach should do you good in your search for what will help.
I once met the criteria for CFS. And my doctor told me that fact, like a good doc should. But he also said that he would not make that his official diagnosis, for much the same reason you just gave. He didn't want to 'wash his hands of me and stop trying things,' as he put it. And it took a few years, but I eventually no longer met the CFS criteria.
I wish you well as you continue to explore what mainstream medicine has to offer. Don't give up on it until you have to. But don't get discouraged if you seem to exhaust all it has to offer, either, since some respond to treatments slightly outside the mainstream, once it comes to that.
Keep thinking as logically as you are. Try one thing at a time. Don't forget the basics of good health as you go about your search with your positive attitude.
We all wish you well, walshsurvey.
jeff
-
walshsurvey
Re: Interpreting CPAP results
Thank you so much, Jeff.
That is so kind of you to give me a pat on the back. I sure appreciate it. I visit many different boards to find out if I "fit". And most times I get ignored, sometimes I get "yelled" at and occasionally (very occasionally) I get someone who truly helps.
Thank you, and I wish you the best on your journey.
God Bless,
Connie
That is so kind of you to give me a pat on the back. I sure appreciate it. I visit many different boards to find out if I "fit". And most times I get ignored, sometimes I get "yelled" at and occasionally (very occasionally) I get someone who truly helps.
Thank you, and I wish you the best on your journey.
God Bless,
Connie
Re: Interpreting CPAP results
You need to gather up copies your 2 night time PSG's (daytime one was for ruling out narcolepsy), you don't want that disorder anyway. The PSG reports (4 or more pages long each with graphs and table charts) should show more information than just obstructive sleep apnea (OSA) events.walshsurvey wrote: had fatigue for 9 years now. Major fatigue, sleeping 14 hours a night and still not feeling rested fatigue, but I've had 3 sleep studies (2 night one day) and they all show me with no apneas.
You can have other parasomnias including REM Behavior Disorder (RBD) which can interrupt the quality of sleep you are getting. Sleep walking and other things you mention about your sleep/dreams are such parasomnias.
http://www.sleepdisorderchannel.com/rem/index.shtml
Ask yourself why you are acting out on your dreams? Normally, when you reach REM where you dream all physical muscle movement is turned off except those needed for breathing. The opposite might be a person that wakes up before that neuro switch as been turned On and find they are awake and cannot move. That syndrome is called Sleep Paralysis, not harmful but can lead to a lot of anxiety, but it is also a form of a parasomnia, usually associated with narcolepsy.
Then long periods of sleep may also indicate a problem with your sleep architecture, if you were getting quality sleep at night you probably wouldn't be sleeping for those 14 hours. I know a lot of us would like to get that much sleep and it may be perfectly normal for you but it can also indicate that the sleep you are getting is NOT quality sleep and that is why you feel so fatigued during the day.
Look on your PSG's, this information should be included in your study and show something similar to:
Normal Sleep Architecture:
Stage1: 5%
Stage2: 50%
Stage3: 10%
Stage4: 10%
Stage REM: 25%
Stage3&4, REM decrease as we age.
Now the above are averages, but if you compare your sleep architecture to the above you might see something different. For example when you fall asleep you may land in Stage1 or Stage2, as time progresses you move to deep sleep in Stage3 or 4, you may go into REM after about 90 minutes you cycle back through those stages again. You may have 3-5 of those cycles per night. Now if you have a parasomnia like PLMD the firing in the brain that causes the limb to move may also send a shock/jolt through you like a perfectly normal hypnic jerk when transitioning from wake to sleep, but this time you are in REM sleep, it may prematurely shorten REM and send you back to deep sleep or even stage 2. Have an apnea same thing, it causes an arousal which if severe enough it may even kick in your fight or flight response and wake you.
But the lower your values are compare to the above may indicate where the problem might be. For example, if you are not getting any REM due to this arousal, you may never dream. If these arousals are interrupting your deep sleep (thought to be where the restorative effects from sleep are gained), you may wake up more fatigued than when you went to bed.
IF your REM sleep is low compared to above one reason might be what ever is interrupting your sleep (EEG arousal) is preventing or kicking you out of a particular stage of sleep. For example, if an arousal kicks you out of REM shown above you might land back at Stage2 (you can land anywhere) so REM may be lower and Stage2 would be higher. Same for deep sleep or Stage3/4.
Now, understand that a obstructive apnea like your tongue falling into the back of your throat may block off your airway, it is not the tongue obstruction that wakes you, it is the associated "arousal".
What you need to find out is what arousals you are having and what is causing the arousals. Obviously when you go to a Sleep Specialist they try to rule out the obvious cause of these arousals such as OSA. But you might have PLM (Periodic Limb Movement) or RLS (Restless Leg Syndrome) and/or 70 some other known sleep disorders and CPAP may never address it.
Other things that can contribute to poor quality sleep are: Medications like SSRI's can destroy your sleep architecture, muscle-skeletal pains can also cause it. Medications like Lexapro is one example, so you need to look at everything carefully any and all medications.
I suggest you obtain copies of all your PSG's, if you want to post them here (black out personal info) maybe we can narrow it down a bit. Armed with that you go back to your sleep specialist and ask specific questions about those non-OSA items on the PSG. Get beyond basic OSA and many doctors are deer in the headlights. The answers you are seeking are probably included in your PSG results, your doctor just can't interpret them or doesn't know what they are.
Now if you eliminate Sleep as being the cause of the fatigue, you look at other things that can contribute to fatigue, blood disorders, low iron (if female), tumors, etc., etc., then it is best to see a hematologist for some extensive blood tests to determine whats up.
Keep in mind that the low AHI you are looking at above is treated, you may have had a lot more events if you didn't use the machine. It will take you 4-6 weeks of consistently using the machine to feel any improvement to your fatigue. You might explore other causes and avenues but you should keep using the machine until you find the other.
someday science will catch up to what I'm saying...
- StillAnotherGuest
- Posts: 1005
- Joined: Sun Sep 24, 2006 6:43 pm
???????
Well, I wouldn't go so far as to say that. That PR Article about the Le Bon Study is incorrect:walshsurvey wrote:No I would say he is right on the money: http://www.talkaboutsleep.com/sleep-dis ... andard.htm
He did a trial, it did not work...he is not a bad doctor because he acted on some research...
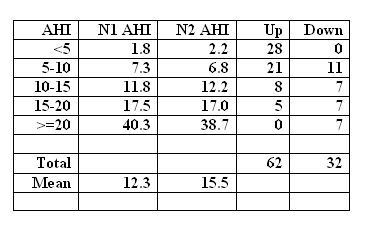
The 62/32 numbers referred to the overall totals in the study. On Night 1 there were 27 patients with AHI >/=20 while on Night 2 there were 45. Is that significant? Absolutely (especially if one thinks that AHI 20.0 is a problem, but 19.9 is fine), but a closer look at Le Bon shows:TAS Article wrote:During night two, 62 patients shifted up to a plus 20 AHI score, almost twice the 32 whose scores dropped on the second night. The scientists said this finding "underscores the larger proportion of subjects having more severe sleep events in night two.
I think what you have to take from this is that the AHI can increase somewhat on a second study night, but to think that a huge percentage of patients with normal PSG really have clinically significant OSA is a real stretch. Now, if say you have like an AHI of 5.0 - 14.0 and EDS symptoms, then CPAP trial is totally appropriate. But thinking that an AHI of 1.0 would be a 20.0 on Night 2? That would be the cousin of "Dial Wingin' ", namely, "Diagnosis Throwin' "
SAG

Aromatherapy may help CPAP compliance. Lavender, Mandarin, Chamomile, and Sweet Marjoram aid in relaxation and sleep. Nature's Gift has these and a blend of all four called SleepEase.
Re: Interpreting CPAP results
Further reading that confirms much of the info from the more experienced posters above:
http://medind.nic.in/iae/t08/i1/iaet08i1p129.pdf
jeff (one of your friendly neighborhood dial-wingin' diagnosis throwers! )
http://medind.nic.in/iae/t08/i1/iaet08i1p129.pdf
jeff (one of your friendly neighborhood dial-wingin' diagnosis throwers! )










