I think that's it. Slight flow limitations that aren't "bad enough" to count (or be marked) as a "Flow Limitation" on the Respironics autopap's data, but enough to trigger the upward probe. I think you and ozij nailed what's happening with the little "chairs."-SWS wrote:I'm still thinking that when we see the upward pressure chairs, we are seeing an upward pressure probe that is launched from probability-based FL components in the flow signal.
Why doesn't APAP respond to apneas?
- rested gal
- Posts: 12880
- Joined: Thu Sep 09, 2004 10:14 pm
- Location: Tennessee
Re: Why doesn't APAP respond to apneas?
ResMed S9 VPAP Auto (ASV)
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Re: Why doesn't APAP respond to apneas?
Unfortunately no pattern match exists for the VB controller in the patent description I have listed below. At first glance "Case 2" appears to be a pattern match---until we read that the pressure rise in "Case 2" is a prior pressure increase that might have caused the variable breathing in the first place.
Patent: "Auto-titration pressure support system and method of using same" Greg Matthews et al
Application number: 10/788,507
Publication number: US 2004/0187870 A1
Filing date: Feb 27, 2004
Inventors: Greg Matthews, Michael T. Kane, Winslow K. Duff, Rochelle Siirola, Daniel Martin, Heather Ressler, Uday Shankar
U.S. Classification
128204220; 128204180; 128204210
I still favor what Rested Gal has highlighted above. In her case it's those darn cigarettes combined with salty Caribbean Ocean air!
Patent: "Auto-titration pressure support system and method of using same" Greg Matthews et al
Application number: 10/788,507
Publication number: US 2004/0187870 A1
Filing date: Feb 27, 2004
Inventors: Greg Matthews, Michael T. Kane, Winslow K. Duff, Rochelle Siirola, Daniel Martin, Heather Ressler, Uday Shankar
U.S. Classification
128204220; 128204180; 128204210
I still favor what Rested Gal has highlighted above. In her case it's those darn cigarettes combined with salty Caribbean Ocean air!
Re: Why doesn't APAP respond to apneas?
VB has to identified for the algorithm to function as planned:
Text from the algorithm training program:
By the way, as far as Respironics is conerned, the "extended" time for constant pressure is 5 to 15 minutes.
Text from the algorithm training program:
.Once flow limitation is observed, the algorithm increases the pressure in response to the flow limitation. Ptherapy is initiated
While in Ptherapy mode, if flow limitation occurs during the last 4 breaths or over several minutes, the algorithm begins a Popt search.
In Popt search mode, the algorithm searches by increasing the pressure at a rate of 0.5 cmH20 per minute. After increasing 1.5 cmH20, if flow limitation continues to occur, continue Popt search. When no further improvement is seen, the algorithm reduces pressure by 0.5 cmH20 and hold Ptherapy for 5 minutes.
Underlined and purple emphasis added by me.The flow limitation algorithm analyzes the inspiratory airflow waveform. It looks for relative changes in the roundness, flatness, peak, or shape ("skewness") of the inspiratory portion of the airflow waveform. These changes are observed both over a short period of time (groups of 4 breaths) and over a long period of time (several minutes). Statistical measures are used to help minimize false event detection while allowing the device to be sensitive to even small changes. For example, a change needs to be observed in at least two of the measures before a response is initiated. Also, responses to Flow Limitations are disabled during unstable breathing conditions such as vibratory snore, apneas, hypopneas, high leak, and variable breathing.
By the way, as far as Respironics is conerned, the "extended" time for constant pressure is 5 to 15 minutes.
Ptherapy - Provides an extended period of constant pressure at ideal level. Typically, this can range from 5-15 minutes depending on where the algorithm is in the analysis.
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Machine: Resmed AirSense10 for Her with Climateline heated hose ; alternating masks. |
And now here is my secret, a very simple secret; it is only with the heart that one can see rightly, what is essential is invisible to the eye.
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Re: Why doesn't APAP respond to apneas?
Ageed. The above description is that responsive scenario we were talking about that does not commence with a downward Pcrit search. Rather, it commences with an upward Popt search because a spontaneous and potentially problematic precursor exists in the patient flow signal.ozij wrote: Text from the algorithm training program:
.Once flow limitation is observed, the algorithm increases the pressure in response to the flow limitation. Ptherapy is initiated
While in Ptherapy mode, if flow limitation occurs during the last 4 breaths or over several minutes, the algorithm begins a Popt search.
In Popt search mode, the algorithm searches by increasing the pressure at a rate of 0.5 cmH20 per minute. After increasing 1.5 cmH20, if flow limitation continues to occur, continue Popt search. When no further improvement is seen, the algorithm reduces pressure by 0.5 cmH20 and hold Ptherapy for 5 minutes.
The part I have outlined in bold red means amplitude variation alone is insufficient. We need another parameter (any two statistical measures actually) to commence the "pressure chair" routines we see on Bev's charts or Rested Gal's charts.The flow limitation algorithm analyzes the inspiratory airflow waveform. It looks for relative changes in the roundness, flatness, peak, or shape ("skewness") of the inspiratory portion of the airflow waveform. These changes are observed both over a short period of time (groups of 4 breaths) and over a long period of time (several minutes). Statistical measures are used to help minimize false event detection while allowing the device to be sensitive to even small changes. For example, a change needs to be observed in at least two of the measures before a response is initiated. Also, responses to Flow Limitations are disabled during unstable breathing conditions such as vibratory snore, apneas, hypopneas, high leak, and variable breathing.
Agreed. However, earlier I mentioned that this control layer enjoys virtually bottom priority. Now that I look at the patent description I'm reminded that this routine has exactly bottom priority. So there is no obligation to hold at 5 to 15 minutes unless this bottom-priority control layer manages to stay in control. This part of the algorithm really sounds like it should be called the "FLC controller" but it's actually that bottom-most control layer called the "auto-cpap controller". And that part you have highlighted above in purple substantiates this module's very low priority contending among the various layers of control.ozij wrote:By the way, as far as Respironics is conerned, the "extended" time for constant pressure is 5 to 15 minutes.
Ptherapy - Provides an extended period of constant pressure at ideal level. Typically, this can range from 5-15 minutes depending on where the algorithm is in the analysis.
Thanks for posting that, ozij!
Re: Why doesn't APAP respond to apneas?
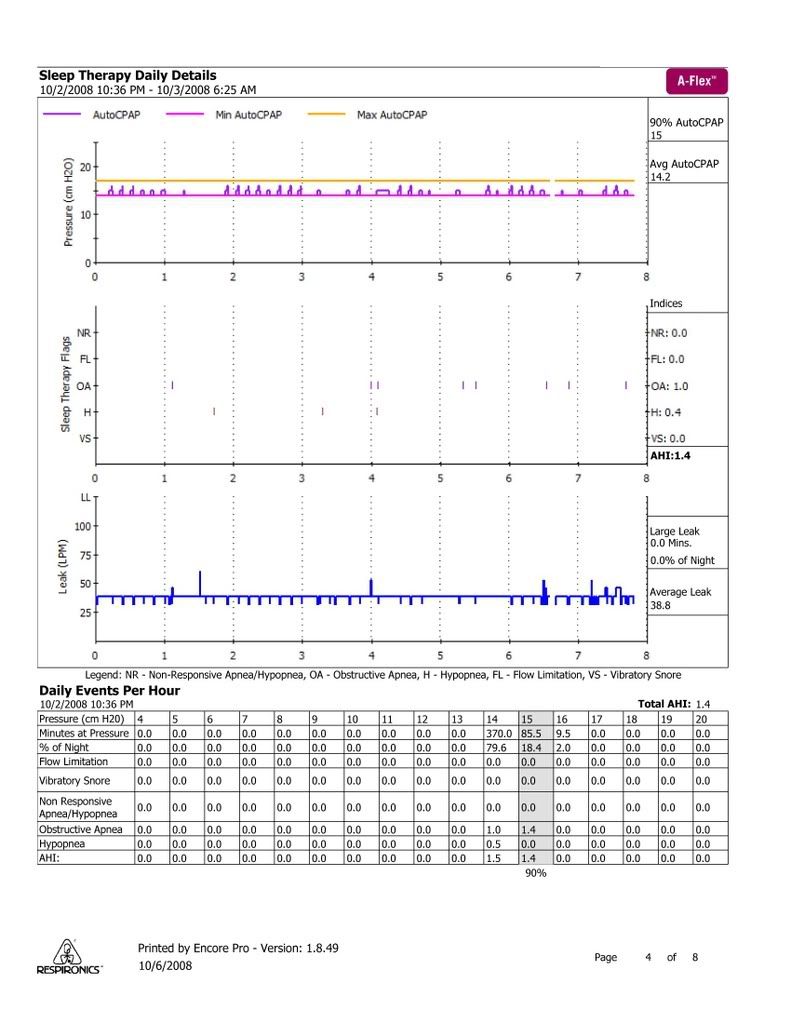
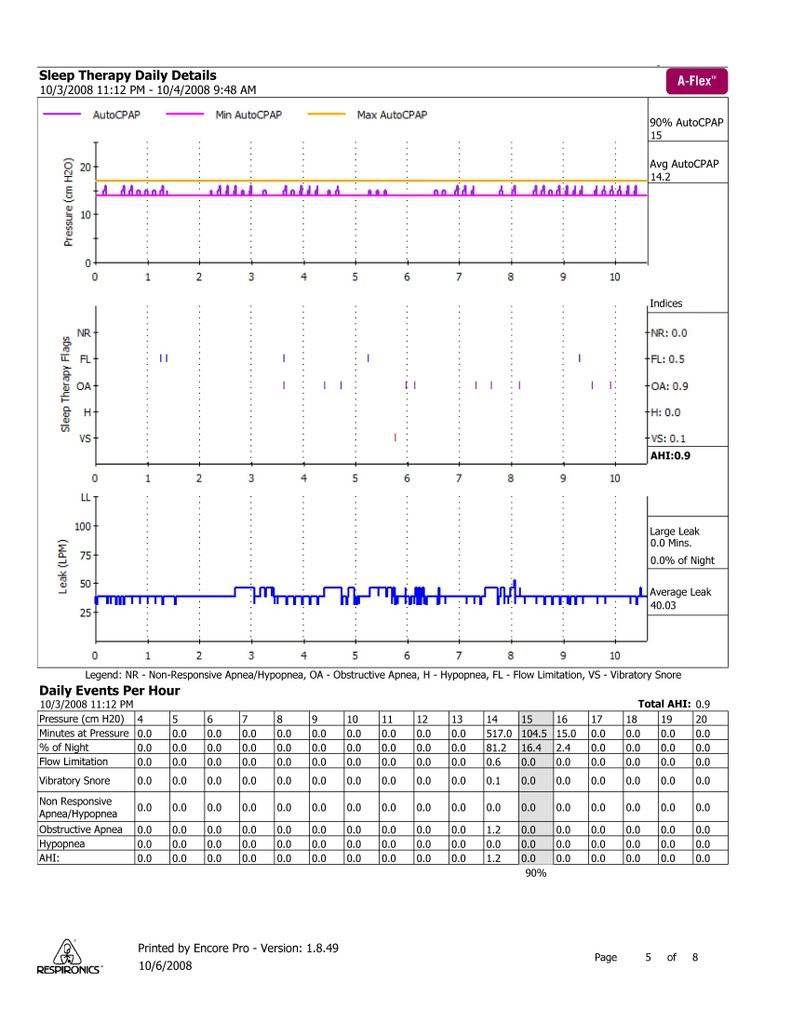
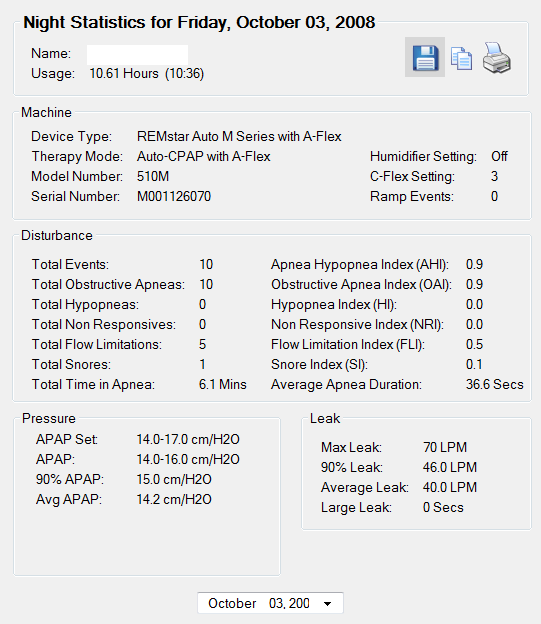
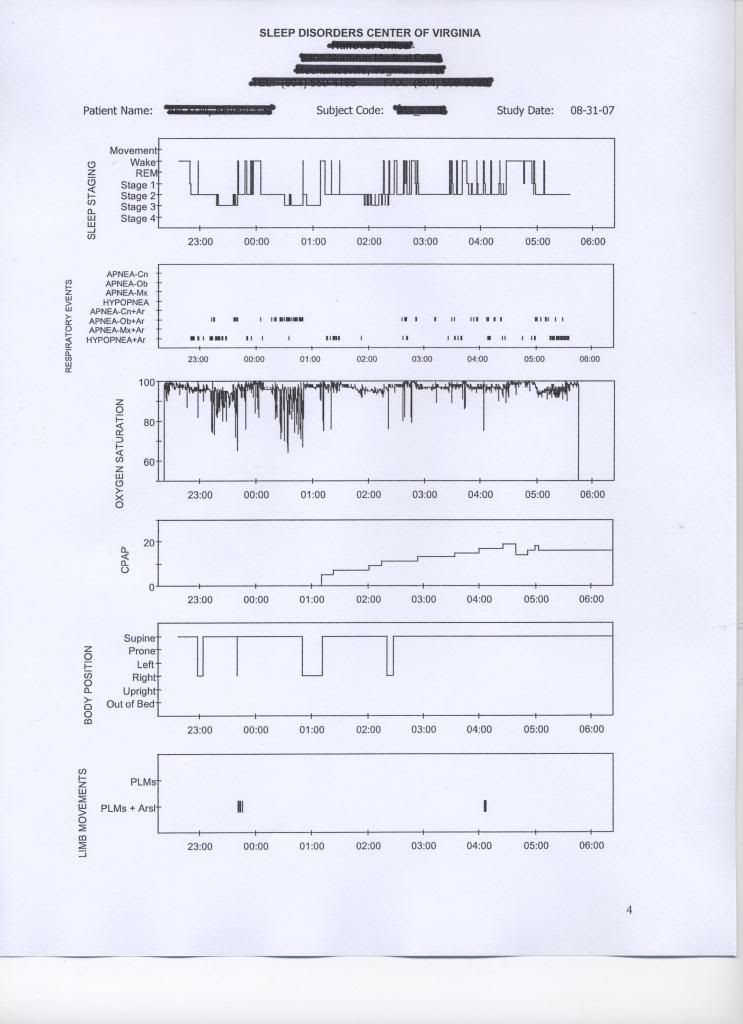
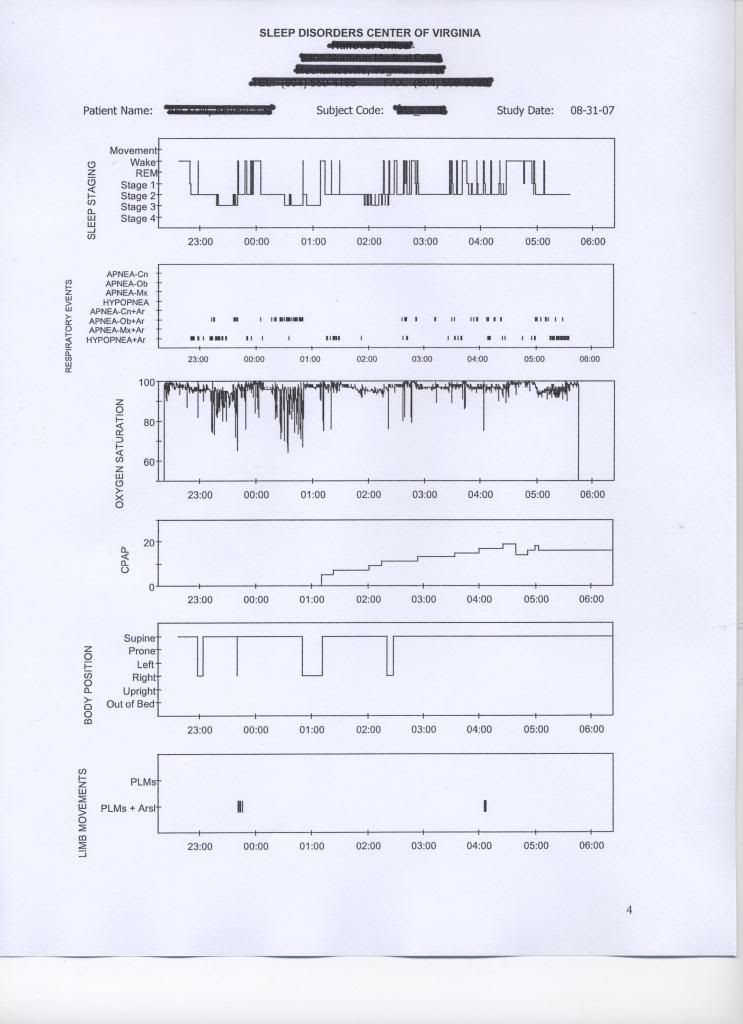
I've been trying to keep an eye on this tread while having a very busy work week. Here are the missing pages of my sleep study from last October:
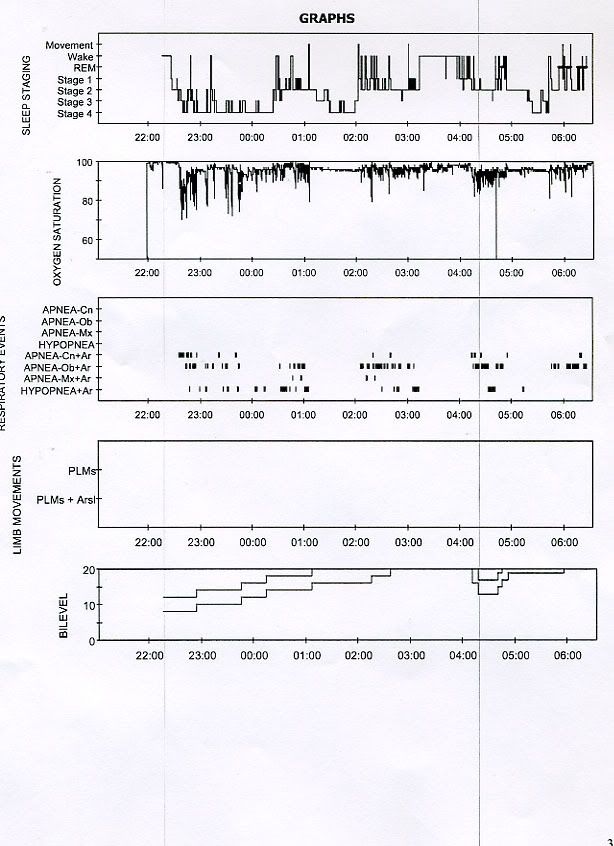
And for those of you who think I lucked out having great leak lines and AHI, here is where I was a year ago:
That was using a Hybrid, which, as you can see, did not work out for me.
Bev
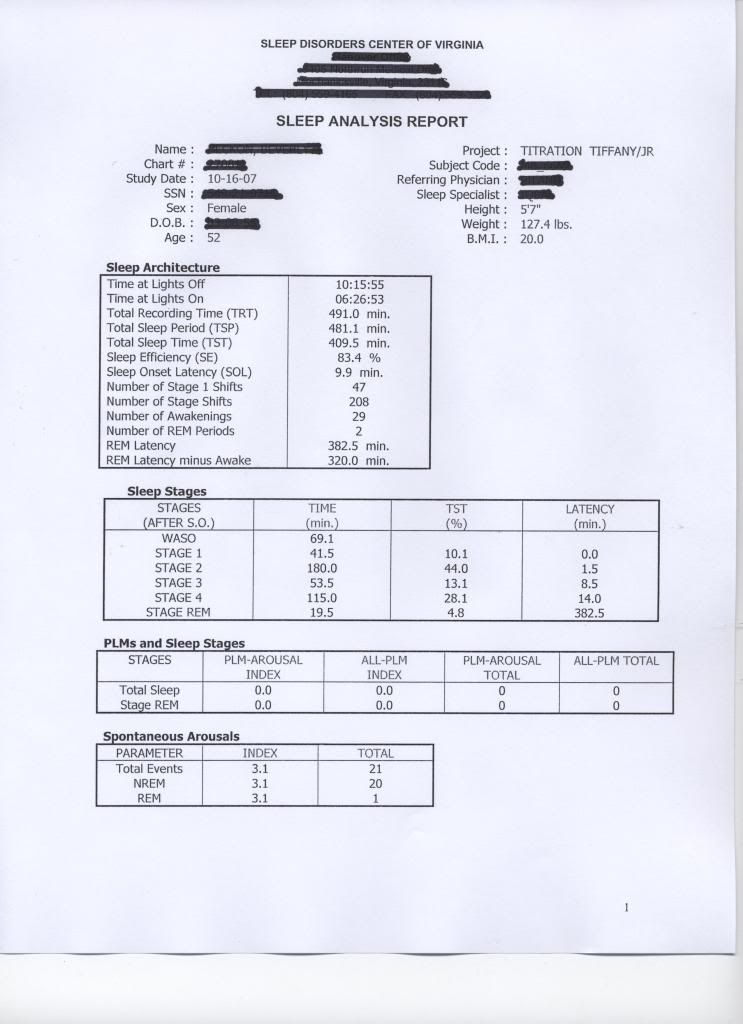
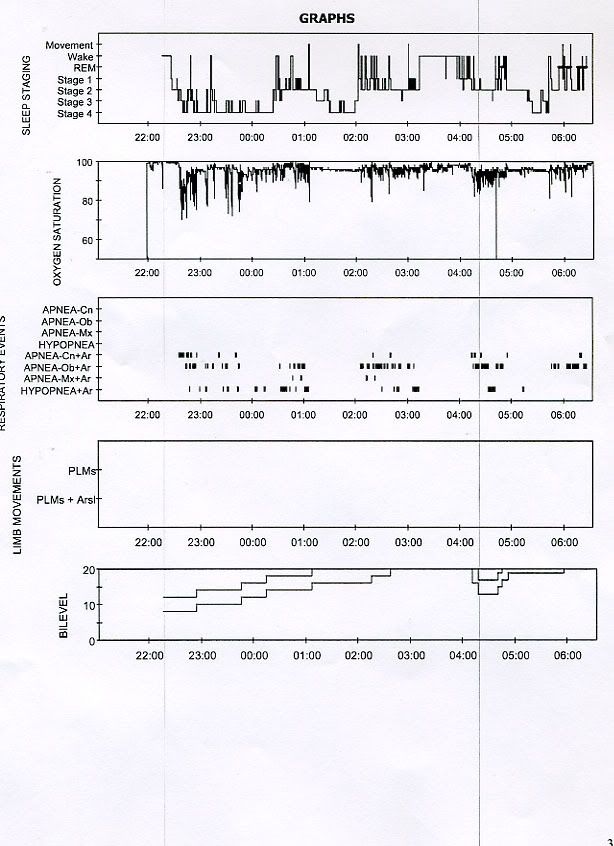
And for those of you who think I lucked out having great leak lines and AHI, here is where I was a year ago:
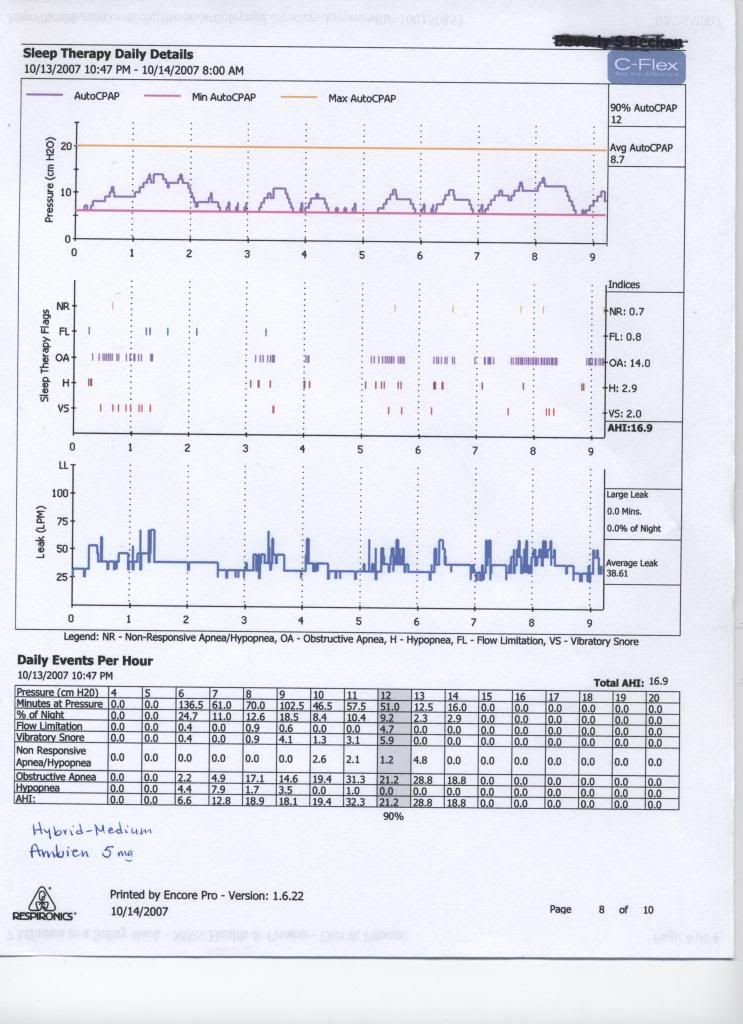
That was using a Hybrid, which, as you can see, did not work out for me.
Bev
Diagnosed 9/4/07
Sleep Study Titrated to 19 cm H2O
Rotating between Activa and Softgel
11/2/07 RemStar M Series Auto with AFlex 14-17
10/17/08 BiPAP Auto SV 13/13-23, BPM Auto, AHI avg <1
Sleep Study Titrated to 19 cm H2O
Rotating between Activa and Softgel
11/2/07 RemStar M Series Auto with AFlex 14-17
10/17/08 BiPAP Auto SV 13/13-23, BPM Auto, AHI avg <1
Re: Why doesn't APAP respond to apneas?
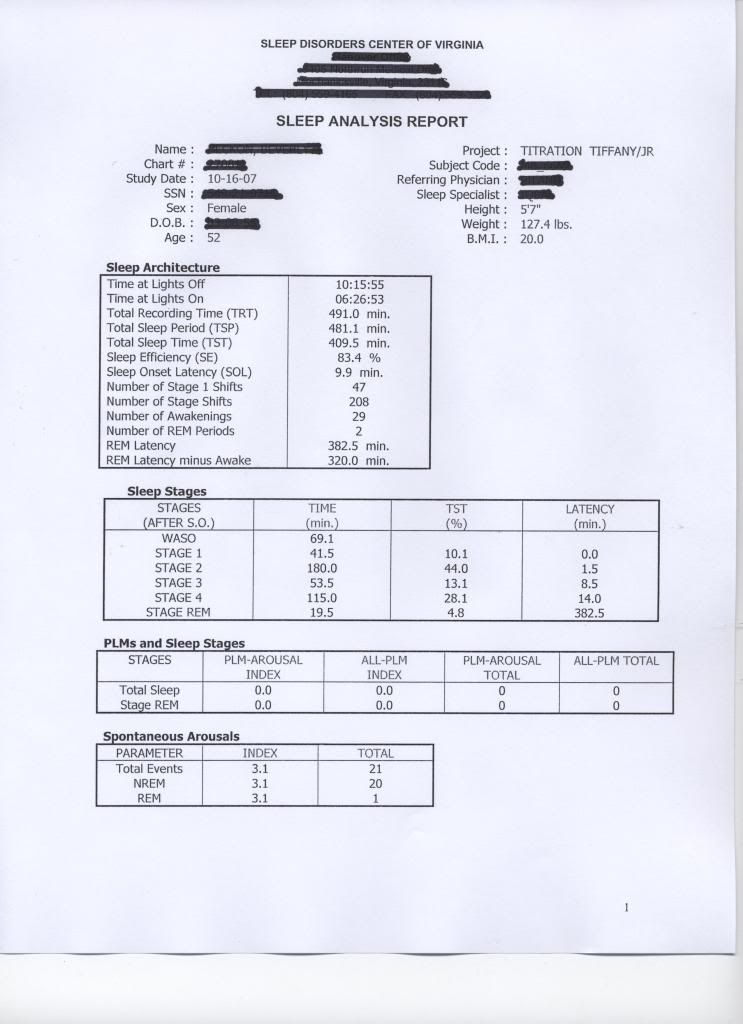
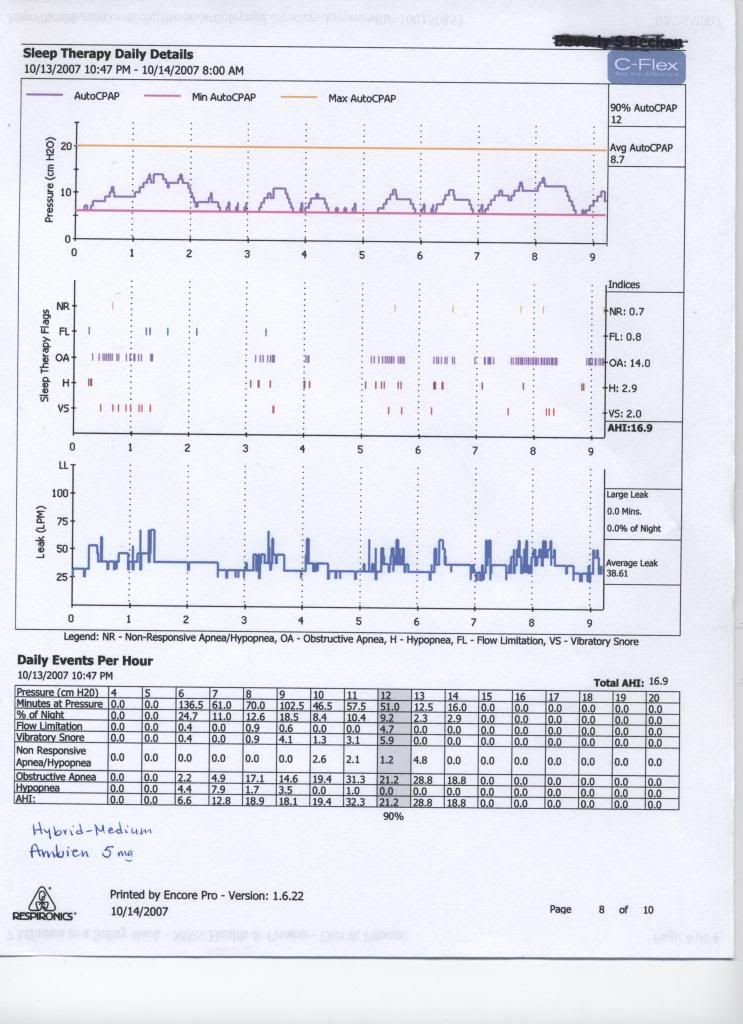
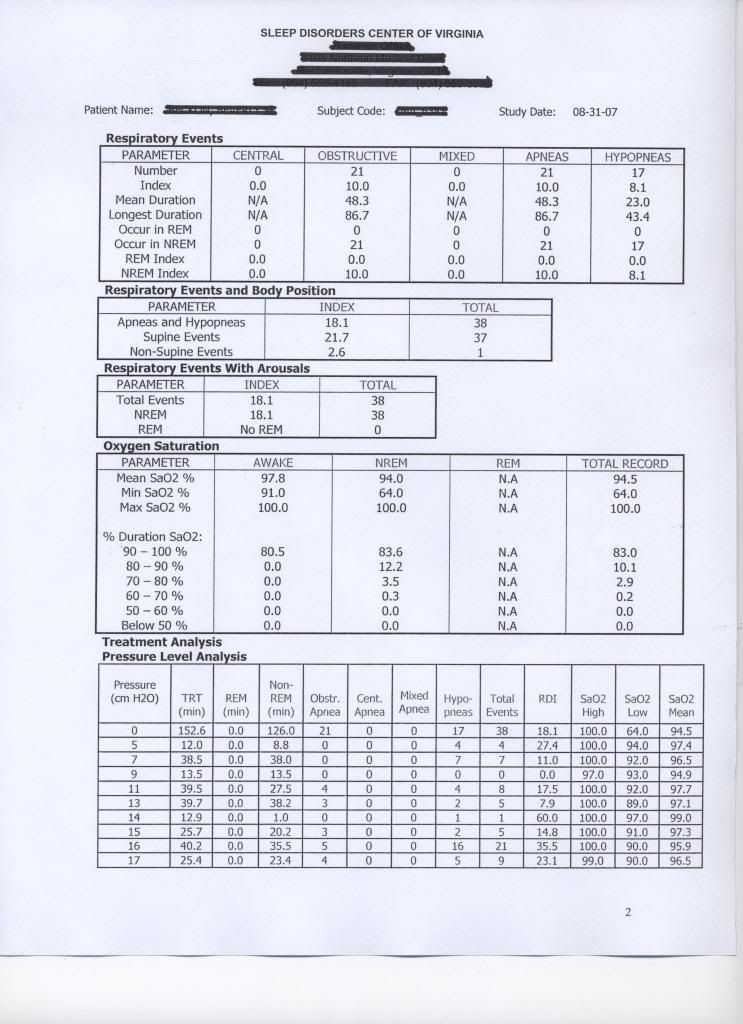
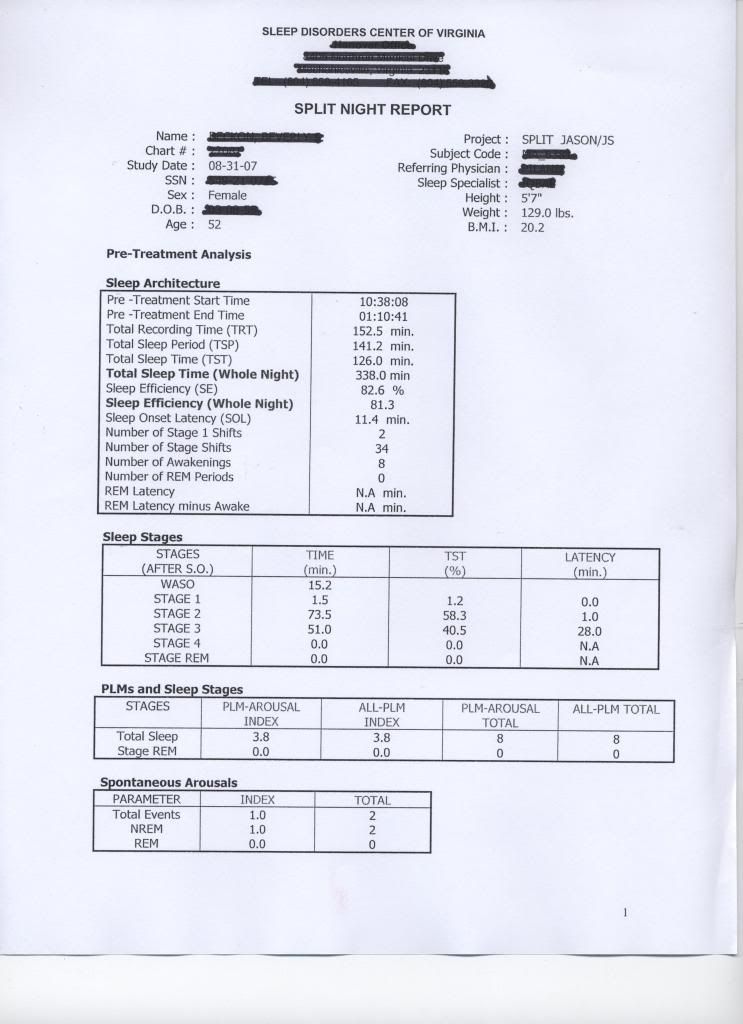
Here is my first Sleep Study:
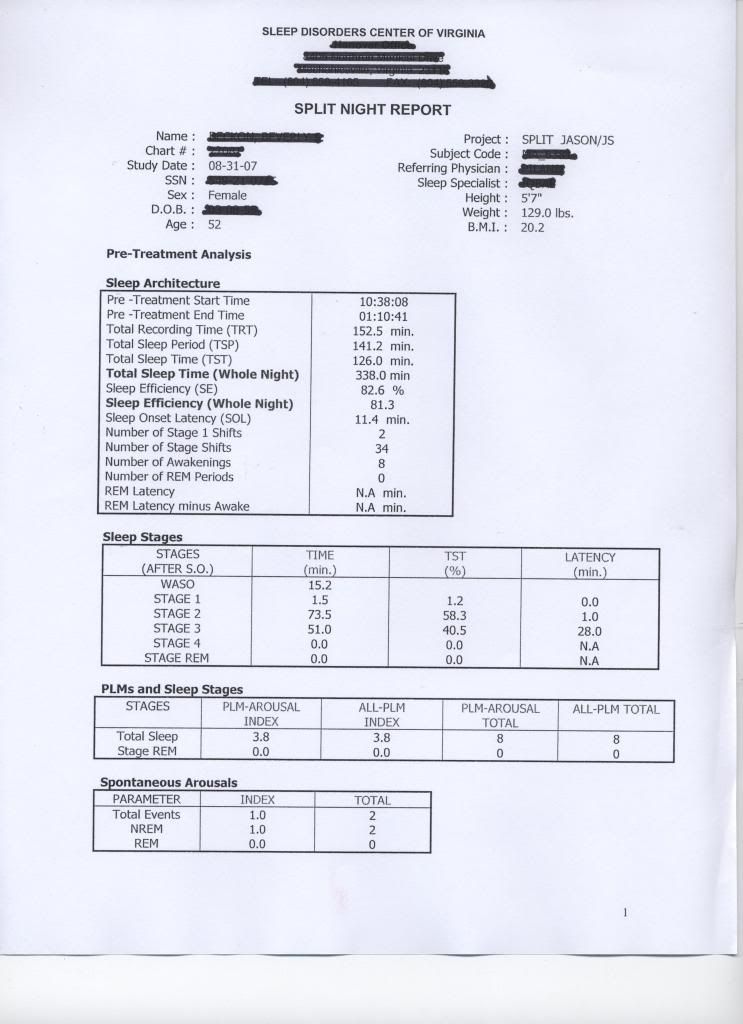
I have a BiPAP Auto SV on the way, so if anyone wants to make suggestions on how to set it up, feel free. My doctor didn't have a clue.
Bev
I have a BiPAP Auto SV on the way, so if anyone wants to make suggestions on how to set it up, feel free. My doctor didn't have a clue.
Bev
Diagnosed 9/4/07
Sleep Study Titrated to 19 cm H2O
Rotating between Activa and Softgel
11/2/07 RemStar M Series Auto with AFlex 14-17
10/17/08 BiPAP Auto SV 13/13-23, BPM Auto, AHI avg <1
Sleep Study Titrated to 19 cm H2O
Rotating between Activa and Softgel
11/2/07 RemStar M Series Auto with AFlex 14-17
10/17/08 BiPAP Auto SV 13/13-23, BPM Auto, AHI avg <1
Re: Why doesn't APAP respond to apneas?
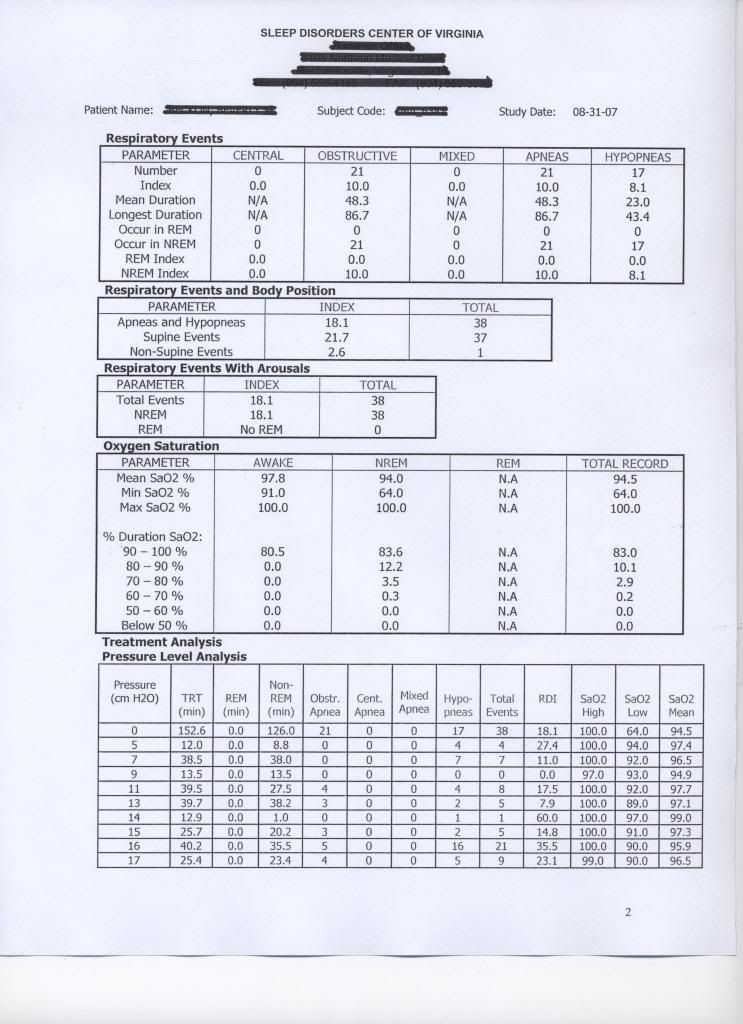
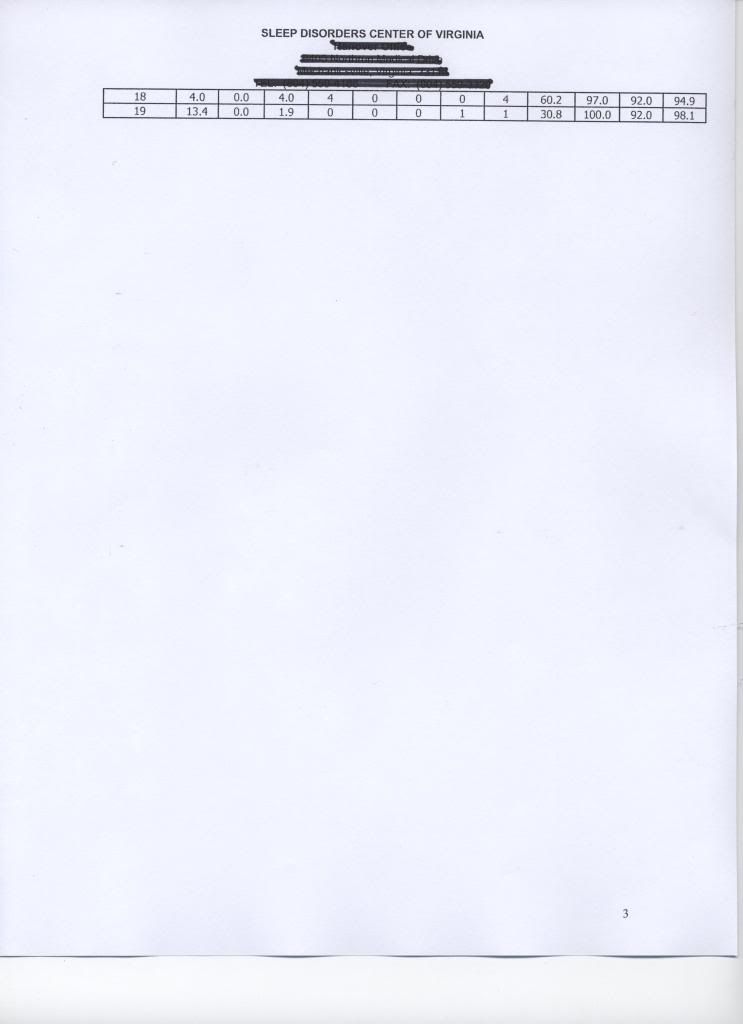
I have to ask why they didn't just stop at 9 cm pressure, that is where you did the best.
Your lab reports seem very complete, No PLM's, not that many Spontaneous Arousals either. There is a pattern seen on both your lab reports and the older Encore Reports, think that is what SWS was talking about with CAP.
Interesting: On your 8/31/07 lab report they tested you on CPAP at or above 17 cm pressure, you had NO central events shown. Now is it you didn't have any or was it you had a inexperienced tech who didn't look for them?
Your lab reports seem very complete, No PLM's, not that many Spontaneous Arousals either. There is a pattern seen on both your lab reports and the older Encore Reports, think that is what SWS was talking about with CAP.
Interesting: On your 8/31/07 lab report they tested you on CPAP at or above 17 cm pressure, you had NO central events shown. Now is it you didn't have any or was it you had a inexperienced tech who didn't look for them?
someday science will catch up to what I'm saying...
Re: Why doesn't APAP respond to apneas?
Good question. All I can say about that is I was so tired after that night that I came home and slept another 6 or so hours. And I am not one to take naps
And I have experienced that if I don't limit my top pressure to 17, I have NRs.
And I have experienced that if I don't limit my top pressure to 17, I have NRs.
Diagnosed 9/4/07
Sleep Study Titrated to 19 cm H2O
Rotating between Activa and Softgel
11/2/07 RemStar M Series Auto with AFlex 14-17
10/17/08 BiPAP Auto SV 13/13-23, BPM Auto, AHI avg <1
Sleep Study Titrated to 19 cm H2O
Rotating between Activa and Softgel
11/2/07 RemStar M Series Auto with AFlex 14-17
10/17/08 BiPAP Auto SV 13/13-23, BPM Auto, AHI avg <1
Re: Why doesn't APAP respond to apneas?
Bev, congratulations on your new acquisition!
Regarding how to set up that machine. The unopened box should come with the clinician's manual. If not, I have a copy as do several others. That will get you into the actual keystrokes or buttons. According to Respironics the initial settings can be based off a previously determind fixed CPAP pressure, or a previously determined fixed pair of BiLevel pressures: http://bipapautosv.respironics.com/
1) establish a data baseline by running at that best BiLevel or CPAP pressure (with BiFlex relief also set to match your current best CFlex/Aflex setting), or
2) use that previous "best" pressure setting as basis for your initial ASV pressure setting values as Respironics describes above (thus an "ASV free" data baseline for later comparison would not get established with this acceptable option)
Thoughts, comments, questions, from others about the above two suggested options?
-----------------------------------------------------------------------
Also, I would like to make two comments about your various data presented thus far. The first comment is that your xPAP and PSG results seem to vary widely from one period of time or set of circumstances to the next. One night in the lab you didn't have any central apneas. Another night in the lab you had quite a few, as well as mixed apneas. My highly unqualified guess about your wildly varying patterns of response to certain stimuli: I think your central physiology just may be inherently defensive or twitchy based on certain physiologic stimuli. That now-you-have-centrals and now-you-don't tendency sure seems like "bifurcation" to perhaps some subtle or not-so-subtle stimuli change to me.
My second comment is more specific and underscores the above generalization. Look at your AHI of 16 that happens to entail that constituent AI of 12. I would like to comment that some people are more sensitive to leaks than others. That Encore chart you show with up-and-down leaks indeed explains your poor sleep and less-than-satisfactory AHI. But you want to know something? There's plenty of pressure there during those leaks to hold your passively-collapsing apneic airway open----if those were passive apneas, which I do not suspect. You didn't reach a large-leak condition, and therefore the APAP machine shouldn't have had any problem whatsoever holding your required pressure. And your data set doesn't show merely subtle signs of signal skew----such as more FL or even H. Those are long, hard frank apneas in response to the ups-and-downs of frequent leaks.
I think, with all that up-and-down pressure fluctuation introduced by those leaks, that one neurologically twitchy and defensive autonomic system may very well have thrown quite a few defensive airway closures there. I don't see in physics how those non-large-leaks could have allowed for full passive airway collapses. Those leaks are all of acceptable magnitude. It's the frequency of activity---the variation---that seems to throw a pretty bad wrench here. So I suspect we might very tentatively surmise that in neurology and biophysics, some people experience very active airway closures that are induced from certain stimuli that would have been perceived or decoded as inert stimuli by plenty of other people. Chemoreceptor sensitivity? Of course. But chemoreceptor sensitivity itself can be a moving target based on input of neurologically "requisite" and defensively "ad hoc" stimuli.
Some folks have acceptable nights when their leaks look like yours. Other folks have a bit of a hard time with leaks like that. And there are other folks---like you---who have a much more difficult time with the leak magnitudes and especially leak frequency variations you have shown above. And since the lab saw a night without central occurrences and at least another night with centrals & mixed events, those outstanding thirty-some-second apneas on your Encore charts just may be central or mixed. And if that physiology of yours really is neurologically twitchy or defensive while asleep, there just may be some bad "neurologically defensive" sleep at work that Encore Pro simply cannot detect. As I said earlier, excessive cyclic alternating pattern is not typically measured in the lab---and was not mentioned anywhere on your reports. I look forward to seeing if BiPAP AutoSV can give you improved sleep by the way of better ventilation and perhaps even some optimal rhythmic pattern of vagal stimulation---soothing reinforcement perhaps? Perhaps less-interrupted and thus better potentiation?
So Bev and others, what are your thoughts about the two options highlighted in blue above? Baseline data first? Straight to ASV? I'm sure Bev welcomes all opinions and comments, and I sure do.
Regarding how to set up that machine. The unopened box should come with the clinician's manual. If not, I have a copy as do several others. That will get you into the actual keystrokes or buttons. According to Respironics the initial settings can be based off a previously determind fixed CPAP pressure, or a previously determined fixed pair of BiLevel pressures: http://bipapautosv.respironics.com/
Respironics BiPAP AutoSV FAQ wrote: If the CPAP or BiPAP pressure is already determined in lab, the patient can be put directly on BiPAPautoSV. To assure that the patient is being properly treated it is a good idea to download the SmartCard data after 7-10 days.
So I'm thinking this thread should probably entertain some discussion about what your previous best fixed CPAP pressure or best fixed BiLevel pressure happened to be. I would suggest coming up with some analysis and rational about what and why your previous best pressure(s) treated you the best. I would then suggest taking that "best" previous pressure setting and doing one of two things with it:Respironics BiPAP AutoSV FAQ wrote:For the set up of these patients it is advisable to use the CPAP or BiPAP pressure from the “old” unit,set the IPAPmax 10cmH2O above the CPAP or BiPAP pressure and set the back up Rate to Auto."
1) establish a data baseline by running at that best BiLevel or CPAP pressure (with BiFlex relief also set to match your current best CFlex/Aflex setting), or
2) use that previous "best" pressure setting as basis for your initial ASV pressure setting values as Respironics describes above (thus an "ASV free" data baseline for later comparison would not get established with this acceptable option)
Thoughts, comments, questions, from others about the above two suggested options?
-----------------------------------------------------------------------
Also, I would like to make two comments about your various data presented thus far. The first comment is that your xPAP and PSG results seem to vary widely from one period of time or set of circumstances to the next. One night in the lab you didn't have any central apneas. Another night in the lab you had quite a few, as well as mixed apneas. My highly unqualified guess about your wildly varying patterns of response to certain stimuli: I think your central physiology just may be inherently defensive or twitchy based on certain physiologic stimuli. That now-you-have-centrals and now-you-don't tendency sure seems like "bifurcation" to perhaps some subtle or not-so-subtle stimuli change to me.
My second comment is more specific and underscores the above generalization. Look at your AHI of 16 that happens to entail that constituent AI of 12. I would like to comment that some people are more sensitive to leaks than others. That Encore chart you show with up-and-down leaks indeed explains your poor sleep and less-than-satisfactory AHI. But you want to know something? There's plenty of pressure there during those leaks to hold your passively-collapsing apneic airway open----if those were passive apneas, which I do not suspect. You didn't reach a large-leak condition, and therefore the APAP machine shouldn't have had any problem whatsoever holding your required pressure. And your data set doesn't show merely subtle signs of signal skew----such as more FL or even H. Those are long, hard frank apneas in response to the ups-and-downs of frequent leaks.
I think, with all that up-and-down pressure fluctuation introduced by those leaks, that one neurologically twitchy and defensive autonomic system may very well have thrown quite a few defensive airway closures there. I don't see in physics how those non-large-leaks could have allowed for full passive airway collapses. Those leaks are all of acceptable magnitude. It's the frequency of activity---the variation---that seems to throw a pretty bad wrench here. So I suspect we might very tentatively surmise that in neurology and biophysics, some people experience very active airway closures that are induced from certain stimuli that would have been perceived or decoded as inert stimuli by plenty of other people. Chemoreceptor sensitivity? Of course. But chemoreceptor sensitivity itself can be a moving target based on input of neurologically "requisite" and defensively "ad hoc" stimuli.
Some folks have acceptable nights when their leaks look like yours. Other folks have a bit of a hard time with leaks like that. And there are other folks---like you---who have a much more difficult time with the leak magnitudes and especially leak frequency variations you have shown above. And since the lab saw a night without central occurrences and at least another night with centrals & mixed events, those outstanding thirty-some-second apneas on your Encore charts just may be central or mixed. And if that physiology of yours really is neurologically twitchy or defensive while asleep, there just may be some bad "neurologically defensive" sleep at work that Encore Pro simply cannot detect. As I said earlier, excessive cyclic alternating pattern is not typically measured in the lab---and was not mentioned anywhere on your reports. I look forward to seeing if BiPAP AutoSV can give you improved sleep by the way of better ventilation and perhaps even some optimal rhythmic pattern of vagal stimulation---soothing reinforcement perhaps? Perhaps less-interrupted and thus better potentiation?
So Bev and others, what are your thoughts about the two options highlighted in blue above? Baseline data first? Straight to ASV? I'm sure Bev welcomes all opinions and comments, and I sure do.
Re: Why doesn't APAP respond to apneas?
Here's the post that strated this thread.
There have been many varying and at times conflicting suggestion and iterprataions of the data we've seen.
Have you tried any of the suggestiona, Bev?
Can you tell us at which pressure you're getting your best subjective results?
O.
There have been many varying and at times conflicting suggestion and iterprataions of the data we've seen.
Have you tried any of the suggestiona, Bev?
Can you tell us at which pressure you're getting your best subjective results?
O.
OutaSync wrote:Since I got James Skinner's Analyser program now, I realize that even though I have my leaks under control and my apneas down, the ones that I have are long! I can't figure out why the APAP doesn't even try to increase pressure to eliminate them. I can see missing a few that are 12 seconds long, but how about an average of 36 seconds? Isn't this why we have these machines?
Help, someone?
Bev
_________________
| Mask: AirFit™ P10 Nasal Pillow CPAP Mask with Headgear |
| Additional Comments: Machine: Resmed AirSense10 for Her with Climateline heated hose ; alternating masks. |
Last edited by ozij on Sun Oct 12, 2008 9:46 am, edited 1 time in total.
And now here is my secret, a very simple secret; it is only with the heart that one can see rightly, what is essential is invisible to the eye.
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Antoine de Saint-Exupery
Good advice is compromised by missing data
Forum member Dog Slobber Nov. 2023
Re: Why doesn't APAP respond to apneas?
SWS: Her 10/16/07 PSG Respiratory events nearly mimics the Encore Pro report pulled 10/13/07. Clearly on that PSG the centrals are the bad guys with her SAO2. While there ARE NRAH's showing up on the 10/13 Encore report, you have to also conclude that many of the obstructive apnea seen on that Encore report are Central and a mix of obstructive, maybe they are mixed apnea I don't know.
Keep in mind when NRAH shows up that is 6 events and 3 pressure increases it takes to fire that off. If there were only 3 or 4 those would be counted by Encore as obstructive (when they were most likely central). So when you see those clusters across the page and compare to the 2 PSG's pattern they are nearly identical.
But if you erase those NR's that same pattern is what I look for when a person is experiencing central apnea along with obstructive. If I had a red pen, I'd circle each one of those clusters and tell you half of those tics seen are central.
The "chair" pressure probing is again seen between the quiet periods on that 10/13 report. No look at the 10/16 PSG titration, Zero events at 9.0 cm pressure. So if it was me looking for a baseline for the Adapt SV settings, I would follow recommended protocol and start with initial settings:
Auto SV mode
Set EPAP at 9.0
IPAP Min at 10 cm (EPAP +1 cm)
IPAP Max at 19 (corrected from 25, should be 10 cm higher than EPAP setting)
Backup Mode = 10 BPM, IT=1.2 (if it cycles to backup mode that should stop the CA's).
I would want to see the above results before increasing EPAP higher. If things are smooth and User initiated breaths are high you can use the BPM to set the backup mode, or if you set backup mode to auto it will set that for you from the Spontaneous finding.
The difference over everything we've seen is the SV will be able to automatically take care of everything on the Inspiration (IPAP) side and hopefully we can get some data to set up the backup mode. Maybe EPAP is set a bit high at 9, but any higher than that and centrals appear in her lab studies. She doesn't seem to have any spontaneous arousals that are of concern, 3.1 is nothing I'd be worried about.
PSG Question: Wonder why they don't give BPM information on a PSG?
With Bev's current settings on the Aflex, it is set up nearly like CPAP, using the minimum pressure at 14 cm and limiting to 17 cm there is not much movement in that range and the result is the lowest AHI out off all the titrations and reports seen.
If it was me, I'd like to see what the AdaptSV's auto mode comes up with. Hopefully the SV can manipulate her IPAP working pressure and inspiration volume to keep those centrals at bay. But EPAP will be fixed, it is my understanding that the same EPAP will be used when in backup mode. The SV protocol calls for using the EPAP pressure that eliminates the obstructive, but you CANNOT rely on the Encore reports we've seen for that information (because it includes both obstructive and central counts and you don't now how much of each). So I would rely on the 10/16/07 PSG titration for that and let the SV do its magic.
Out of everything I've seen here on Bev, if I only had a CPAP to use, I'd set it at 9 cm.
Keep in mind when NRAH shows up that is 6 events and 3 pressure increases it takes to fire that off. If there were only 3 or 4 those would be counted by Encore as obstructive (when they were most likely central). So when you see those clusters across the page and compare to the 2 PSG's pattern they are nearly identical.
But if you erase those NR's that same pattern is what I look for when a person is experiencing central apnea along with obstructive. If I had a red pen, I'd circle each one of those clusters and tell you half of those tics seen are central.
The "chair" pressure probing is again seen between the quiet periods on that 10/13 report. No look at the 10/16 PSG titration, Zero events at 9.0 cm pressure. So if it was me looking for a baseline for the Adapt SV settings, I would follow recommended protocol and start with initial settings:
Auto SV mode
Set EPAP at 9.0
IPAP Min at 10 cm (EPAP +1 cm)
IPAP Max at 19 (corrected from 25, should be 10 cm higher than EPAP setting)
Backup Mode = 10 BPM, IT=1.2 (if it cycles to backup mode that should stop the CA's).
I would want to see the above results before increasing EPAP higher. If things are smooth and User initiated breaths are high you can use the BPM to set the backup mode, or if you set backup mode to auto it will set that for you from the Spontaneous finding.
The difference over everything we've seen is the SV will be able to automatically take care of everything on the Inspiration (IPAP) side and hopefully we can get some data to set up the backup mode. Maybe EPAP is set a bit high at 9, but any higher than that and centrals appear in her lab studies. She doesn't seem to have any spontaneous arousals that are of concern, 3.1 is nothing I'd be worried about.
PSG Question: Wonder why they don't give BPM information on a PSG?
With Bev's current settings on the Aflex, it is set up nearly like CPAP, using the minimum pressure at 14 cm and limiting to 17 cm there is not much movement in that range and the result is the lowest AHI out off all the titrations and reports seen.
If it was me, I'd like to see what the AdaptSV's auto mode comes up with. Hopefully the SV can manipulate her IPAP working pressure and inspiration volume to keep those centrals at bay. But EPAP will be fixed, it is my understanding that the same EPAP will be used when in backup mode. The SV protocol calls for using the EPAP pressure that eliminates the obstructive, but you CANNOT rely on the Encore reports we've seen for that information (because it includes both obstructive and central counts and you don't now how much of each). So I would rely on the 10/16/07 PSG titration for that and let the SV do its magic.
Out of everything I've seen here on Bev, if I only had a CPAP to use, I'd set it at 9 cm.
Last edited by Snoredog on Mon Oct 13, 2008 4:54 am, edited 1 time in total.
someday science will catch up to what I'm saying...
Re: Why doesn't APAP respond to apneas?
Ozij, thanks for posting that original Encore chart on the same page. I absolutely agree with what I think is your implied point comparing those two Encore charts: that the wide pressure range and especially low APAP min pressure can account for those hard apneic closures. And any xPAP situation may be as simple as needing more pressure to hold a passively collapsing airway open---in this case because APAP just can't manage to get that much-needed high pressure on time.
However, when that situation happens I'm thinking we can probably attribute the situation to two broad possibilities: 1) poor temporal variable analysis by the algorithm (more common I'll bet) and/or 2) perhaps apneic closures that are not simply a "passive" lack of neuromuscular airway maintenance, but rather some active component of neuromuscular airway closure at work in some etiologic scenarios. If that second presumably defensive case is even occurring in epidemiology, then we might expect that hypothetical person to also manifest even more disruptive sleep architecture than the case of non-defensive etiologies. We might also expect wide pressure requirements from night-to-night regarding how much work a CPAP machine would have to exert to offset those erratic and actively orchestrated airway closures. And quite possibly, we might even expect night-to-night bifurcation regarding a defensively skewed respiratory controller (central dysregulation one night but not another night). Okay. Enough wild speculation from me for now.
Snoredog, the interesting thing about Bev's response to pressures is that optimal pressure(s) in the labs and even at home seem to be a bit of a moving target. Admittedly those 13.5 minutes at 9 cm pressure looked great. But it's also conceivable that Bev can occasionally sleep for 13.5 solid minutes while not using CPAP and still have no A or H! So that 9 cm at 13.5 minutes may be good data or it may be meaningless data if those 13.5 minutes were highly atypical.
I'm thus inclined to think that Bev's own observations of what pressure(s) feel best over the long haul may be key in setting up her BiPAP autoSV machine---especially if sleep architecture is adversely impaired by certain low or high pressures that happen to yield acceptable Encore Pro results.
However, when that situation happens I'm thinking we can probably attribute the situation to two broad possibilities: 1) poor temporal variable analysis by the algorithm (more common I'll bet) and/or 2) perhaps apneic closures that are not simply a "passive" lack of neuromuscular airway maintenance, but rather some active component of neuromuscular airway closure at work in some etiologic scenarios. If that second presumably defensive case is even occurring in epidemiology, then we might expect that hypothetical person to also manifest even more disruptive sleep architecture than the case of non-defensive etiologies. We might also expect wide pressure requirements from night-to-night regarding how much work a CPAP machine would have to exert to offset those erratic and actively orchestrated airway closures. And quite possibly, we might even expect night-to-night bifurcation regarding a defensively skewed respiratory controller (central dysregulation one night but not another night). Okay. Enough wild speculation from me for now.
Snoredog, the interesting thing about Bev's response to pressures is that optimal pressure(s) in the labs and even at home seem to be a bit of a moving target. Admittedly those 13.5 minutes at 9 cm pressure looked great. But it's also conceivable that Bev can occasionally sleep for 13.5 solid minutes while not using CPAP and still have no A or H! So that 9 cm at 13.5 minutes may be good data or it may be meaningless data if those 13.5 minutes were highly atypical.
I'm thus inclined to think that Bev's own observations of what pressure(s) feel best over the long haul may be key in setting up her BiPAP autoSV machine---especially if sleep architecture is adversely impaired by certain low or high pressures that happen to yield acceptable Encore Pro results.
Re: Why doesn't APAP respond to apneas?
Hi Bev,
I'm going to give a few observations based on my own experiences, which may or may not reflect your situation at all. It is only what worked for me, and may give you some ideas. I'm sorry that I wasn't able to read the entire thread (I only got through about 2 pages). I will not be able to contribute to the technical discussion either... Anyway...
- I use the P&B 420E
- I was titrated in the range of 7-10 on straight CPAP. They said that above 10cm the central's became an issue.
- After a year, I've found that 10.5 is the best pressure, and the central's only become an issue at 11cm. I still get a few central's now and then on 10.5 (maybe 3-4 per night) but they are not a problem for me. So their interpretation and my experience is obviously a bit different!
- I tried both APAP and straight CPAP. The APAP mode wrecks my sleep - I wake up (consciously or not) every time the pressure changes. I feel miserable the next day. On APAP I tried 7-10, 8-10, 8-12, 10-12, and on straight CPAP, everything from 7 to 11.
- On every single pressure between 7 and 10, my AHI (obstructive + central apeans + hypopneas) was ALWAYS <1.0. I still never felt better.
- Same thing on all the above APAP modes I tried.
- If I go only on AHI, 7.0 is in theory my right pressure. But then I feel miserable during the day.
HOWEVER, and this is big HOWEVER, and it took me a whole year to figure this out: I am really bothered by "flow limitations" , in the way P&B detects and describes them.
When I went to 10.5, the flow limitations were reduced more than 50%, and now for the first I've had a sustained period of feeling better and sleeping well. Most people would say that flow limitations are not an issue, but they DO affect MY sleep. Also I do not know how the other machines interpret flow limitations - I am only going by what my experiences were with the P&B.
My second observation is related to insomnia. I have always had a horrible sleep schedule. I was never tired at night, and was always exhausted in the morning. That changed somewhat in the first year with CPAP, but never truly went away. I always knew that I got insomnia when I DID NOT sleep well the previous night. So the fact that my insomnia kept coming back at those other pressures was one of the indications that they were not the right pressure.
My insomnia has almost completely gone away now that I have been at the right pressure (10.5) for several months now. In fact, within a couple of days of starting 10.5 I noticed that the insomnia was much less.
I have never ever heard of this from anyone else, but in my case, poor sleep = insomnia the next night. Weird, but true.
...so for whatever these observations are worth...! I know this is not very scientific, it's only one person's experiences, and every person is different, but maybe it helps you and maybe it doesn't.
The most important thing is DO NOT GIVE UP!
I'm going to give a few observations based on my own experiences, which may or may not reflect your situation at all. It is only what worked for me, and may give you some ideas. I'm sorry that I wasn't able to read the entire thread (I only got through about 2 pages). I will not be able to contribute to the technical discussion either... Anyway...
- I use the P&B 420E
- I was titrated in the range of 7-10 on straight CPAP. They said that above 10cm the central's became an issue.
- After a year, I've found that 10.5 is the best pressure, and the central's only become an issue at 11cm. I still get a few central's now and then on 10.5 (maybe 3-4 per night) but they are not a problem for me. So their interpretation and my experience is obviously a bit different!
- I tried both APAP and straight CPAP. The APAP mode wrecks my sleep - I wake up (consciously or not) every time the pressure changes. I feel miserable the next day. On APAP I tried 7-10, 8-10, 8-12, 10-12, and on straight CPAP, everything from 7 to 11.
- On every single pressure between 7 and 10, my AHI (obstructive + central apeans + hypopneas) was ALWAYS <1.0. I still never felt better.
- Same thing on all the above APAP modes I tried.
- If I go only on AHI, 7.0 is in theory my right pressure. But then I feel miserable during the day.
HOWEVER, and this is big HOWEVER, and it took me a whole year to figure this out: I am really bothered by "flow limitations" , in the way P&B detects and describes them.
When I went to 10.5, the flow limitations were reduced more than 50%, and now for the first I've had a sustained period of feeling better and sleeping well. Most people would say that flow limitations are not an issue, but they DO affect MY sleep. Also I do not know how the other machines interpret flow limitations - I am only going by what my experiences were with the P&B.
My second observation is related to insomnia. I have always had a horrible sleep schedule. I was never tired at night, and was always exhausted in the morning. That changed somewhat in the first year with CPAP, but never truly went away. I always knew that I got insomnia when I DID NOT sleep well the previous night. So the fact that my insomnia kept coming back at those other pressures was one of the indications that they were not the right pressure.
My insomnia has almost completely gone away now that I have been at the right pressure (10.5) for several months now. In fact, within a couple of days of starting 10.5 I noticed that the insomnia was much less.
I have never ever heard of this from anyone else, but in my case, poor sleep = insomnia the next night. Weird, but true.
...so for whatever these observations are worth...! I know this is not very scientific, it's only one person's experiences, and every person is different, but maybe it helps you and maybe it doesn't.
The most important thing is DO NOT GIVE UP!
PR System One APAP, 10cm
Activa nasal mask + mouth taping w/ 3M micropore tape + Pap-cap + PADACHEEK + Pur-sleep
Hosehead since 31 July 2007, yippie!
Activa nasal mask + mouth taping w/ 3M micropore tape + Pap-cap + PADACHEEK + Pur-sleep
Hosehead since 31 July 2007, yippie!
- rested gal
- Posts: 12880
- Joined: Thu Sep 09, 2004 10:14 pm
- Location: Tennessee
Re: Why doesn't APAP respond to apneas?
Very interesting... seeing the data from two of Bev's nights using autopap. I don't think those look bad at all. The few apneas that happened were scattered... not hitting in solid block. I think I'd be very happy with those results and would have kept on "as is." Very nice low leak rate.
I realize you're concerned, Bev, about the average length of the few apneas that were sneaking through despite treatment. I don't think I'd worry about that, given how far apart the apneas that occur are. However, if I were going to tweak for that, I think I would simply raise the minimum pressure of the autopap another cm (or two, or three) to see if that kept the airway open better. A range of 15 - 20 (with A-flex at "3") is what I'd probably try, if that were my data.
I realize you're concerned, Bev, about the average length of the few apneas that were sneaking through despite treatment. I don't think I'd worry about that, given how far apart the apneas that occur are. However, if I were going to tweak for that, I think I would simply raise the minimum pressure of the autopap another cm (or two, or three) to see if that kept the airway open better. A range of 15 - 20 (with A-flex at "3") is what I'd probably try, if that were my data.
ResMed S9 VPAP Auto (ASV)
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Humidifier: Integrated + Climate Control hose
Mask: Aeiomed Headrest (deconstructed, with homemade straps
3M painters tape over mouth
ALL LINKS by rested gal:
viewtopic.php?t=17435
Re: Why doesn't APAP respond to apneas?
Great single-channel flow-sensor data coupled with very poor daytime cognition and perhaps ESD. And to complicate matters, those poor daytime symptoms can be entirely unrelated to CPAP therapy.
But I agree with ozij's and now Rested Gal's reinforcing suggestion: what happens when the bottom pressure gets bumped up a bit? And I would also comment that Rested Gal can sleep at 20 cm pressure with no adverse effects the following day. Rhetorically: how many of us can do that?
But I agree with ozij's and now Rested Gal's reinforcing suggestion: what happens when the bottom pressure gets bumped up a bit? And I would also comment that Rested Gal can sleep at 20 cm pressure with no adverse effects the following day. Rhetorically: how many of us can do that?